In this article, we present the case of a triple-negative breast carcinoma T2N0M0 with negative genetic testing and a Ki67 proliferation index of 80%, indicating an aggressive cancer. Despite the initial recommendation to use a peripherally inserted central catheter (PICC) for treatment, the patient opted to use a midline due to her concerns about potential complications associated with the PICC, such as deep vein thrombosis (DVT). This decision was made in conjunction with the medical team, considering both the risks and benefits. Treatment included neoadjuvant therapy and immunotherapy, achieving a significant reduction of the tumour from 47mm to remnants of 2mm and 1mm after surgery, with a negative sentinel node. In this article, based on the experience of the Intravascular Therapy Team at Basurto Hospital in Bilbao, nurse Oscar Parrado answers the question of whether it is possible to use a midline catheter to administer irritating and vesicant drugs, since in the treatment of triple-negative breast carcinoma, the midline catheter has emerged as an effective option, offering a viable alternative to the traditional peripherally inserted central catheter (PICC).
Read on to find out how and why…
Diagnostics and Procedure
The clinical case discussed is a diagnosis of triple-negative infiltrating ductal carcinoma of the left breast in a 51 year-old woman.
A ductal carcinoma is one in which the neoplastic cells are confined within a duct. In the case of breast cancer, there are two types of ductal carcinoma: ductal carcinoma in-situ (it cannot spread to the lymph nodes in the armpit, and axillary dissection is not indicated) and infiltrating ductal carcinoma (IDC). In the case of IDC, the origin is in the milk ducts and being infiltrating implies that it affects surrounding breast tissue. It is the most common type of breast cancer, around 75-80% of cases, according to the American Cancer Society. In many cases it is asymptomatic and can be detected through a mammogram. Life expectancy depends on the subtypes.
In this case, we are dealing with a triple-negative breast carcinoma T2N0M0 with a negative genetic study. With a Ki67 proliferation index of 80% (30% or more is considered high). Therefore, we are dealing with a case in which the cancer was quite aggressive.
Learn more: Ki67 is a protein found in dividing cells, so a Ki67 proliferation index means that many cells are dividing rapidly, and the cancer is likely to grow and spread.
Treatment Based on Diagnosis
The treatment proposed for this patient was neoadjuvant treatment (treatment focused on reducing the size of the tumour prior to the primary treatment, usually surgery) and immunotherapy. Because the tumour was initially 47mm in size, the patient was to begin treatment with chemotherapy (doxorubicin and paclitaxel) and immunotherapy (pembrolizumab) in January 2024.
After the first cycle, the patient began to have episodes of fever since the administration of the second cycle of pembrolizumab-carboplatin-paclitaxel, so she went to the emergency room with fever, nausea and up to three vomiting episodes after starting CT the previous day thus developing a systemic inflammatory response syndrome (SIRS) secondary to the administration of Pembrolizumab.
Inflammatory Response Syndrome
It is a consequence of the activation of the immune system and a massive inflammatory reaction caused by a systemic release of cytokines (cytokine storm) that can lead to multi-organ failure and the death of the patient.
Learn more: SIRS when at least 2 of these alterations are present: fever or hypothermia, tachypnoea (>20 breaths per minute), tachycardia (>90 beats per minute), Leucocytosis (>12,000 leukocytes/mm³) or Leukopenia (<4,000 leukocytes/mm³) or left shift (immature neutrophil count in blood ≥10%).
The aetiology is very diverse; it can be caused by an infection, physical agents (burns, radiation, etc.), chemical agents (drugs, pesticides, etc.), multiple traumas, surgery, a myocardial infarction, thromboembolic disease, an autoimmune disease, etc. When it is caused by a known infection, it is called sepsis.

ICU Admission
Due to this inflammatory response for which she went to the emergency room, the patient was admitted to the ICU (Intermediate Multipurpose Care Unit) from 03/03/2024 to 03/05/2024, where a CVC catheter (antecubital) was placed on the same day 03/05/2024 and was removed on 11/03/2024 due to suspected catheter-associated bacteraemia, the catheter tip was collected which was finally negative.
During her stay in the ICU, a PICC (antecubital catheter) was placed in the right upper limb. She developed recurrent fever, leading to the removal of the antecubital catheter, and the catheter tip was collected on 11/03/2024.
After performing blood tests, the diagnosis was SIRS post-immunotherapy. After several days of admission and stabilisation, the patient was admitted to the oncology ward and subsequently admitted to the ward until 15/03/2024.
On the 8th day of admission, the patient began to have fevers of up to 38.5ºC with no apparent focus, the only focus being the CVC with haematoma in the right upper extremity. Blood cultures were negative on the 10th day. It was decided to remove the CVC and collect the catheter tip (the culture was negative). A new CT scan was requested to look for a possible focus, in which PTE was observed in LSD. After the PTE was found, an echo-doppler was also requested to assess other possible thromboses on 14/03/2024, the culture of which was negative.
Choosing a New Route: Midline for The Treatment of Breast Carcinoma
With the need for a new central line, the patient is offered the option of inserting a PICC or a port to continue with the chemotherapy treatment. However, the patient, a radiologist by profession, refuses both the placement of a new PICC and the placement of a reservoir for fear of developing complications, especially DVT.
In a first ETI consultation, we explained all the options available at that time. On the other hand, she was a DIVA patient, and her colleagues at the Day Hospital had a lot of problems injecting her.
The main risks/complications of short venous catheters are:
- Insertion technique, blind technique. Patients with low venous capital suffer from multi-tasking (appearance of multiple haematomas, impact on patients) and depletion of venous capital.
- Catheters made of rigid plastic (Teflon, polyethene) and poor biocompatibility can cause phlebitis. In addition, they have reduced chemical resistance. The catheter lasts less than six days.
- Extravasation.
- The tip is placed in a small vein with a low flow rate (60ml/min). In larger veins, the tip is placed in the cephalic or basilic veins (250ml/min). The size of the vein also affects the speed of drug infusion. In many cases, with short peripheral catheters, more than a third of the vein’s calibre is occupied, resulting in a risk of thrombosis.
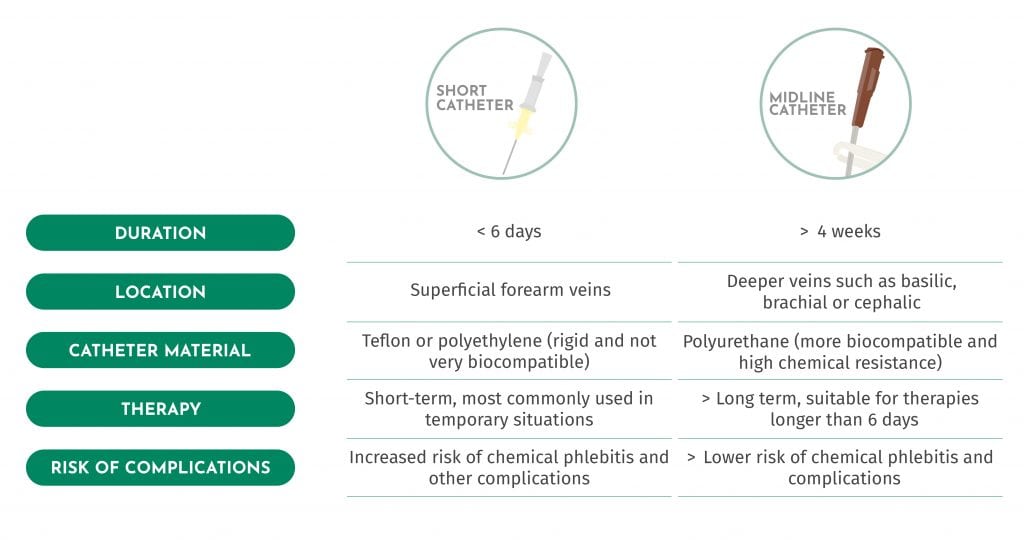
Therefore, taking into account the risks, benefits and recommendations, and assuming that ultrasound-guided puncture is safer because the vein can be channelled using an ultrasound scanner and the catheter tip is correctly positioned, the only possible alternative for administering the treatment is via a peripheral route, despite the risks involved. Therefore, in order to guarantee maximum safety when administering the treatment, it was decided to opt for a mini-midline, specifically a 4Fr and 10cm long one, to guarantee safety in the event of extravasation. The main reasons for deciding to opt for this type of vascular access are: 1. the patient was a DIVA, and 2. it was a decision agreed with the patient, who was aware of the risks and benefits.
Catheter Insertion
Throughout the treatment, a total of 10 catheters were placed between 03/05/2024 and 29/07/2024, which were removed after 24-48 hours at the request of the patient herself since she was afraid of developing a new DVT or some type of complication related to the catheter, as pointed out above. In addition, the patient did not want to have any device that would make her daily life difficult for personal reasons.
The only reason for maintaining the catheter for at least 24 hours after treatment is that the patient had very poor venous access and a great fear of developing a new SIRS and not having quick venous access. In other words, the catheter could have stayed inserted in the patient, however, the entire team felt it was more important to respect the patient’s decision.
Use of Midline to Prevent Venous Wear
The correct choice of device must be made. The main point to keep in mind is that the inserted devices have never occupied more than one third of the vein. In this case, the vein was more than 0.4cm and less than 0.5cm, so a 4 Fr catheter was inserted.
RAPEVA method prior to each insertion. During the procedure we check that there have been no significant changes in the venous capital, nor stenosis of the vein calibre or damage to the endothelium. By repeatedly puncturing the same area, small scars that reduce over time can be seen.

The procedure is the same as for common midline insertion:
We review the patient’s medical history, collect relevant information, review the most recent tests, and review the treatment that the patient will receive. A checklist is filled out, and we conduct a first interview with the nurses, “first ETI”.
First, we perform a functional assessment of the limb to be punctured and carry out an ultrasound examination using the RAPEVA method. Then, we insert the catheter using the modified Seldinger technique and check the position of the catheter tip. We explain to the patient the route and final location of the catheter, as well as the warning signs and symptoms so that any adverse effects can be quickly identified, and immediate intervention can be taken.
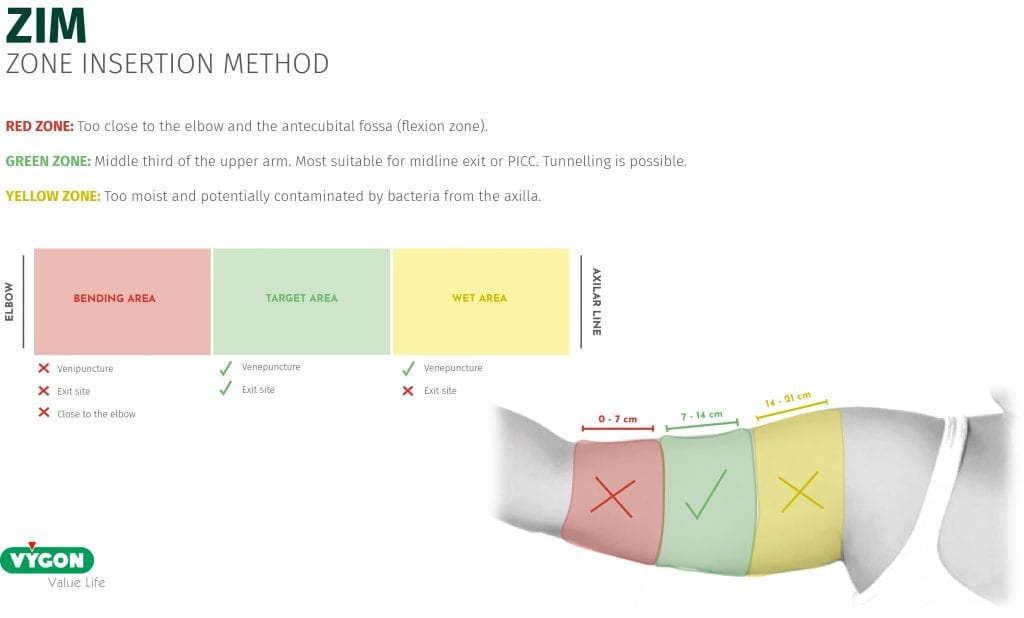
WHY IS THE PUNCTURE SITE DIFFERENT FROM WHERE A MIDLINE INSERTION IS USUALLY PERFORMED?
The choice of catheter exit site is determined by rapid visualisation of extravasation.
Following the ZIM method (Zone Insertion Method), we chose the lower part of the green zone (close to the red zone). Despite not being the ideal site for the puncture, we ensure that the tip of the catheter (10cm) is lodged on the inner side of the arm at the level of the vein itself that we punctured (in this case, we chose the basilic vein), so that, if an extravasation occurs, the patient would notice pain, burning, heat, erythema and/or swelling in the area. At the level of the subclavian, this is much more difficult to objectify and surely, by the time the patient notices it, there will already be damage.
Once the catheter has been inserted, the patient goes to the Day Hospital to administer the treatment. Afterwards, she returns home with the catheter in place in case any complications arise in the 24 hours following chemotherapy. The next day, the patient returns for a check-up and removal of the device. If there are no incidents, a date is set for the next insertion of the catheter, in accordance with the next chemotherapy cycle. This procedure is repeated weekly until the chemotherapy cycles are completed.
Throughout the duration of the treatment, we monitored the patient’s case to assess the appearance of complications (there have been none), having direct contact with both the patient and the colleagues at the Day Hospital.
The patient has currently been discharged and is recovering favourably from the entire process.
Can Irritating and Vesicant Drugs be Administered via a Midline Catheter?

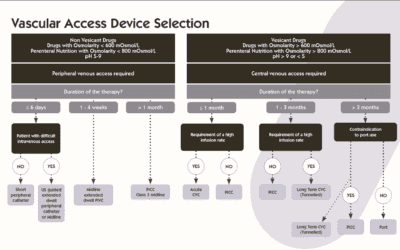
Scientific evidence shows that CVCs, PICCs, and reservoirs are the only safe options for administering irritating and vesicant drugs.
The administration of irritant and vesicant drugs through the midline is not recommended due to a high risk of complications that may cause harm to the patient. Based on our experience, its use can be considered in very specific cases, always carefully analysing the risk-benefit of each case. In addition, it is essential to take extreme precautions by establishing strict protocols and homogenising clinical practice as much as possible in order to avoid variability in care. In our daily practice, the 10cm midline ultrasound-guided insertion and with correct monitoring of adverse effects has allowed us to administer vesicant drugs in patients who, due to pathology, therapeutic ceiling or their own decision, are not candidates for other VADs.
Conclusion
In conclusion, the use of the midline catheter in the treatment of triple-negative breast cancer has been shown to be a viable alternative to the peripherally inserted central catheter (PICC), especially in patients with concerns about complications such as deep vein thrombosis. Throughout treatment, significant tumour shrinkage was achieved, and serious complications were avoided, suggesting that with appropriate monitoring and patient selection, the midline catheter may be a safe and effective option in certain cases of breast cancer.