Short Peripheral Intravenous Catheters (SPIVCs) are commonly used as default vascular access devices by practicians around the world for short and midterm therapies. However, they can be a problem in case of medium therapies as that would entail the insertion of multiple cannulas. Many professionals choose to place central lines instead. However, they can be contraindicated, and they can require expertise and additional costs. To bridge the gap between SPIVCs and central lines, midlines were introduced in the 1950s and are today referred to as “the middle ground” of intravenous therapy administration1.
In this article, we will define midlines and discuss their indications and their advantages compared to SPIVCs and/or central lines.
What are midlines?
The Infusion Therapy Standards of Practice (INS 2021) differentiate between mini-Midlines and Midline catheters. It defines them as follow:
Long peripheral intravenous catheter (long PIVC) or mini-midline: inserted in either superficial or deep peripheral veins and offers an option when a short PIVC is not long enough to adequately cannulate the available vein. A long PIVC can be inserted via traditional over-the-needle technique or with more advanced procedures, such as Seldinger and accelerated Seldinger techniques.
Midline catheter: inserted into a peripheral vein of the upper arm via the basilic, cephalic, or brachial vein with the terminal tip located at the level of the axilla in children and adults; for neonates, in addition to arm veins, midline catheters may be inserted via a scalp vein with the distal tip located in the jugular vein above the clavicle or in the lower extremity with the distal tip located below the inguinal crease.
In this article, we will refer to midlines based on the second definition.
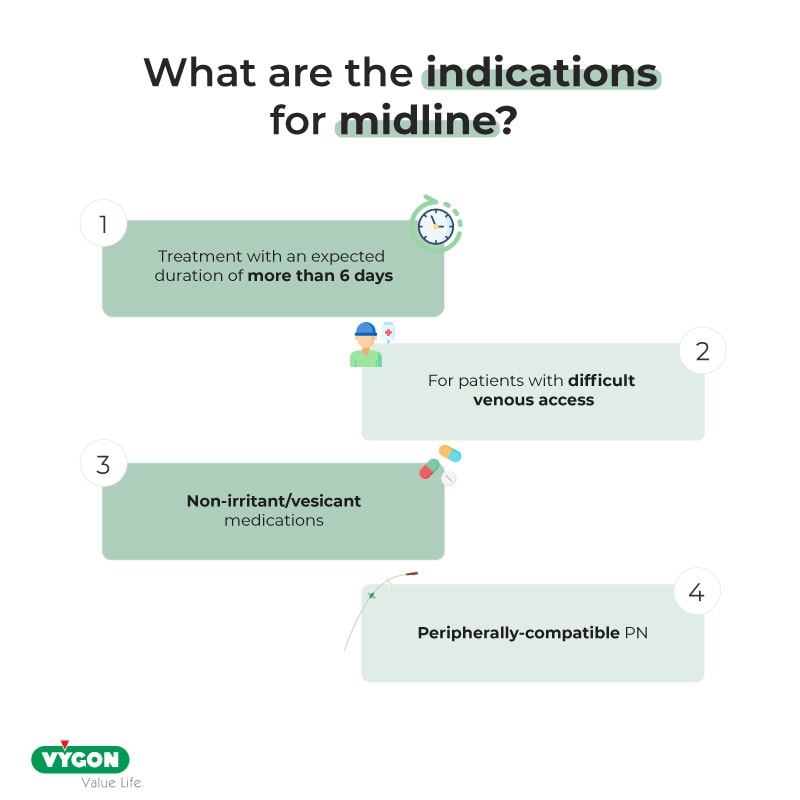
Midline indications
Midlines can be used for the administration of blood, fluids and peripherally compatible medications’ and can be used in the following circumstances:
Advantages of midlines
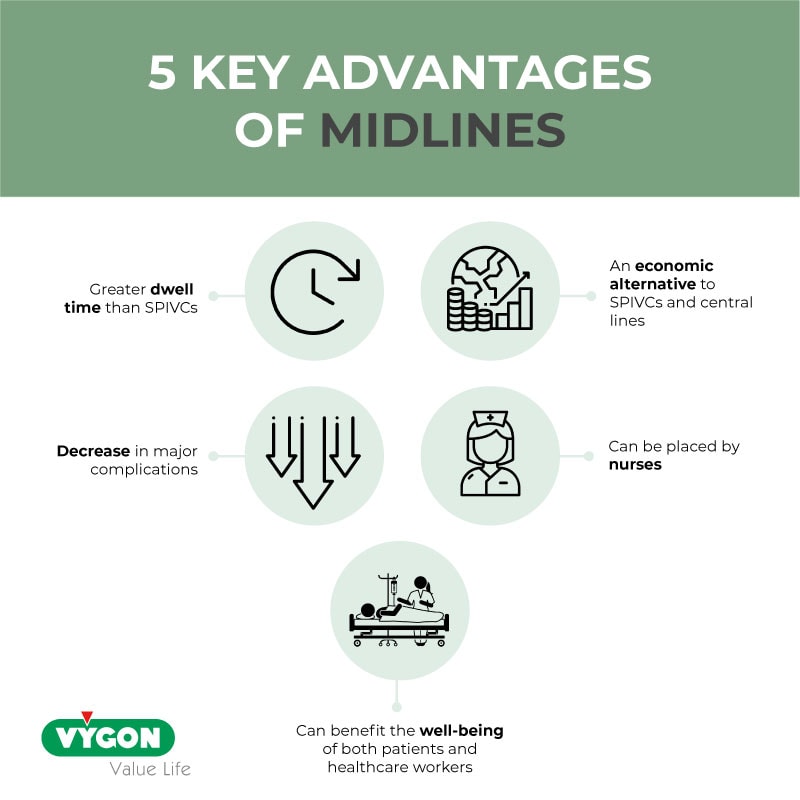
In many situations, it can be preferable to use a midline rather than an SPIVC or a central line considering their various advantages:
- Greater dwell time than SPIVCs
Midlines have a greater dwell time than SPIVCs thanks to their length.
Devries et al., (2016) suggests that SPIVCs dwell for 2.3 to 4.3 days. For midterm therapies, practicians often have to remove or replace the cannula which leads to the multiplication of punctures. This makes SPIVCs inappropriate for therapies that are longer than this period or for patients with difficult venous access.
According to Fabiani et al., Moureau et al., 2015, Midlines have a dwell time of 7.7 to 16.4 days. It is longer than SPIVCs’ and therefore more suitable for safe and secure mid-term therapies.
- Decrease in major complications
The use of midlines can lower the risk of early and delayed complications compared to SPIVCs and central lines.
A study conducted by Marsh et al., (2023) has shown that SPIVCs had a higher risk of phlebitis and PIVC infiltration. For PICCs, literature has found that the use of PICCs was associated to a higher risk of developing serious complications such as CLABSI (Central line-associated Bloodstream Infections) and catheter occlusion.2
Therefore, Midlines appear to be safer for patients that require mid-term therapies.
- Can be placed by nurses
The placement of midlines can be delegated to nurses. Not only is it timesaving for the teams, but it can also increase their use inside the units and therefore, reduce the risk of serious complications that come with the insertion of central lines.
To ensure the proper functioning of the VAD and the safety of the patient, training of healthcare workers in midline insertion, care and maintenance is a requirement.
- Can benefit the well-being of both patients and healthcare professionals
Midlines can have a positive impact on the well-being of patients and healthcare workers.
Literature demonstrates that midlines have a high rate of first-attempt success.3 This makes them a more comfortable option for patients as they do not have to undergo multiple needlesticks. This can ensure venous capital preservation.
The reduction of punctures coupled with the possible insertion of midlines in DIVA and overweight patients can also benefit doctors and nurses. It would help reduce their workload and stress linked to the difficulty of finding veins.
- An economic alternative
Midlines are a cost-effective alternative compared to SPIVCs and central lines.
Literature has found that the increase of midline placement by a trained team on a two-year period significantly reduced the cost of VAD placement. 4 The cost savings through midlines can be explained by a limited use of more costly central lines with patients that do not require them, as well as the decrease of costs linked to central line-associated complications such as CLABSI.
Moreover, midlines are a more economic option compared to SPIVCs as the latter require multiple cannula replacements in prolonged therapies, that can reach four or more repeated insertions.5 This can also be beneficial for patients with difficult-to-access peripheral veins.
With patients’ safety and well-being as a priority, midlines could be considered the most suitable VAD for midterm therapies. It offers various advantages that improve the patients’ experience and general comfort. Moreover, the device is a key asset for healthcare institutions as it has been proven to be more economic and easier to use by the personnel. Nevertheless, specific training of nurses and healthcare professionals should be conducted in order to ensure a safe patient-centred procedure.
Summary:
Bibliography:
- N Richard Anderson – “Midline catheters: the middle ground of intravenous therapy administration” – Journal of Infusion Nursing 2004 Sep-Oct;27(5):313-21 – Available online: https://pubmed.ncbi.nlm.nih.gov/15385895/
- Lakshmi Swaminathan, Scott Flanders, Jennifer Horowitz, Qisu Zhang, Megan O’Malley, Vineet Chopra – “Safety and Outcomes of Midline Catheters vs Peripherally Inserted Central Catheters for Patients With Short-term Indications: A Multicenter Study” – JAMA Intern Med. 2022 Jan 1;182(1):50-58 – Available online: https://pubmed.ncbi.nlm.nih.gov/34842905/
- Daniel Z.Adams MD, Andrew Little DO, Charles Vinsant MD, Sorabh Khandelwal MD – “The Midline Catheter: A Clinical Review” – The Journal of Emergency Medicine (Volume 51, Issue 3, September 2016, Pages 252 – 258 – Available online: https://www.sciencedirect.com/science/article/abs/pii/S0736467916301597
- Shanja-Grabarz, L. Santoriello, G. Ritter, V. Patel, J. Nicastro, R. Barrera. – “Midline Catheters: An Underutilized, Cost-Effective Means of Decreasing Central Venous Catheter Use” – Academic surgical congress abstracts archive (January, 2019) – Available online: https://www.asc-abstracts.org/abs2019/59-05-midline-catheters-an-underutilized-cost-effective-means-of-decreasing-central-venous-catheter-use/
- Emma Bundgaard Nielsen, Louise Antonsen, Camilla Mensel, Nikolaj Milandt, Lars Skov Dalgaard, Britta Skov Illum, Hanne Arildsen, Peter Juhl-Olsen – “The efficacy of midline catheters—a prospective, randomized, active-controlled study” – International Journal of Infectious Diseases (Volume 102, January 2021, Pages 220-225) – Available online: https://www.sciencedirect.com/science/article/pii/S1201971220322578
- DeVries, M., Valentine, M., & Mancos, P. (2016) – “Protected clinical indication of peripheral intravenous lines: Successful implementation” – Journal of the Association for Vascular Access, 21(2), 89–92. https://doi. org/10.1016/j.java.2016.03.001
- Moureau, N., Sigl, G., & Hill, M. (2015). “How to establish an effective midline program: A case study of 2 hospitals.” – Journal of the Association for Vascular Access, 20(3), 179–188. https://doi.org/10.1016/j.java. 2015.05.001
- Fabiani, A., Dreas, L., & Sanson, G. (2017). “Ultrasound-guided deep-arm veins insertion of long peripheral catheters in patients with difficult venous access after cardiac surgery. Heart & Lung”, 46(1), 46–53. https://doi.org/10.1016/j.hrtlng.2016.09.003
- Nicole Marsh, Emily N. Larsen, Catherine O’Brien, Robert S. Ware, Tricia M. Kleidon, Peter Groom, Barbara Hewer, Evan Alexandrou, Julie Flynn, Kaylene Woollett, Claire M. Rickard – “Safety and efficacy of midline catheters versus peripheral intravenous catheters: A pilot randomized controlled trial” – International Journal of Nursing Practice (Volume 29, Issue 2, April 2023) – Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/ijn.13110







