In acute care areas, where patients can be hemodynamically unstable (or at risk of instability), clinicians aim to optimize perfusion in order to avoid organ dysfunction, multi-organ failure, or even death. These areas refer to critical care units, perioperative areas and elsewhere, where circulatory derangements may occur.
Commonly, whensoever perfusion became important, arterial blood pressure (ABP), specifically mean arterial pressure (MAP), was considered to be a key hemodynamic surrogate for oxygen delivery, with hypotension being the clinical concern, as it associates with worsened patient outcomes. However, it is now known that hypotension does not strictly lead to organ hypoperfusion, and it has heterogenous underlying pathophysiological mechanisms (Meng, 2021).
If one breaks down the clinical concept of ABP, there are its two determinants: cardiac output (CO) and systemic vascular resistance (SVR). The heterogenicity underlying hypotension, relates to the potential changes in both ABP’s determinants, and the therapeutical action upon each possible scenario will be different.
Literature increasingly states that CO is not only a determinant of ABP, but it also strongly and independently correlates with organic perfusion, enrichening the traditional view of perfusion resulting from perfusion pressure divided by the regional vascular resistances. CO is ultimately supplied to various tissues and organs and the summation of their perfusion shares corresponds to CO (Meng, 2021).
CO is determined by single metabolic needs and varies between individuals. Thus, there is not a CO reference that can fit all patients. While ABP and CO are physiologically linked, there is no evidence of an important correlation between arterial pressure and CO in patients undergoing surgical procedures, for instance. Perioperative CO-guided management evidence suggests that CO-guided management may reduce postoperative complications and mortality, with regards that there is a need for further studies, with increased robustness (Kouz et al., 2024).
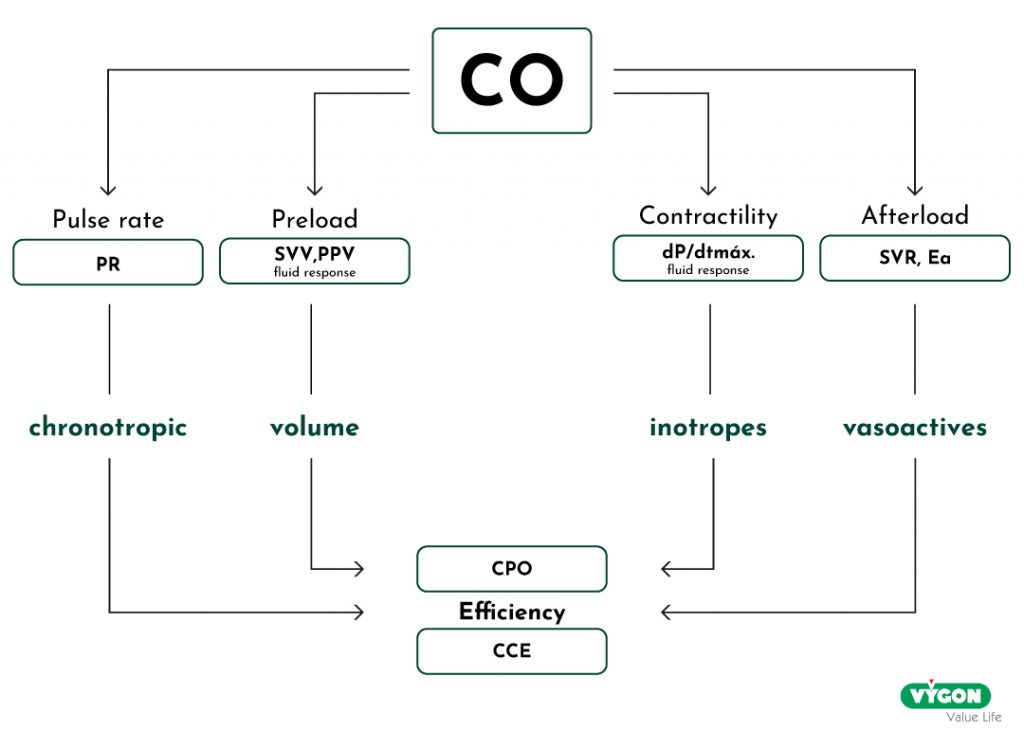
By monitoring CO and its determinants (preload, heart rate, afterload and contractility), it is possible to have additional guidance and support through different therapeutical stages, such as differential diagnoses (e.g.: shock mechanisms), treatment and response, as well as continuous evaluation (Huygh et al, 2016). Through more advanced hemodynamic values, one can simply identify the real ongoing needs of the patient, whether it is fluid resuscitation, vasopressors, chronotropic or inotropic agents, potentially enhancing patient’s outcomes by acting in a more proactive and personalized mode.
Several methods are available for the purpose of CO monitoring – including pulmonary artery or transpulmonary thermodilution, pulse wave analysis, oesophageal Doppler, and bioreactance techniques. The choice of technology will depend mostly on its clinical applicability, but also on user’s expertise and approach. Despite the choice of monitoring method, a basic physiologic and pathophysiologic understanding of relevant haemodynamic variables remains essential (Kouz et al., 2024).
As an additional note, ideally, CO monitoring technology should be reliable, continuous, non-invasive, operator-independent, cost-effective, and have a fast response. CO monitoring devices should progressively become interconnected with other types of monitoring solutions. The environmental sustainability associated to these devices is also increasingly considered (de Waal et al., 2009; Kouz et al., 2024).
BIBLIOGRAPHY
- de Waal, Eric ECa et al. (2009). Cardiac output monitoring. Current Opinion in Anaesthesiology 22(1): p71-77. doi: 10.1097/ACO.0b013e32831f44d0
- Huygh, J. et al. (2016). Hemodynamic monitoring in the critically ill: an overview of current cardiac output monitoring methods [version 1; referees: 3 approved] F1000Research 5(F1000 Faculty Rev):2855. doi: 10.12688/f1000research.8991.1
- Kouz, K. et al. (2024). Haemodynamic monitoring during noncardiac surgery: past, present, and future. Journal of Clinical Monitoring and Computing (2024) 38:565–580. doi: 10.1007/s10877-024-01161-2.
- Meng, L. (2021). Heterogeneous impact of hypotension on organ perfusion and outcomes: a narrative review. British Journal of Anaesthesia, vol. 127, Issue 6, 845 – 86. doi: 10.1016/j.bja.2021.06.048






