In Neonatal Intensive Care Units (NICUs), vascular access is not optional, it’s essential. Over 85% of NICU patients require some form of Vascular Access (VA) during their stay. Yet, the choice of device and insertion technique can dramatically affect outcomes. Repeated failed attempts, high complication rates, and vein depletion are common issues when conventional methods are used.
This is not only a clinical problem but also a problem of excessive variation between operators. Every failed attempt means more pain for the baby, more stress for the care team, and more anxiety for the parents. So how do we fix this?
The Solution: Modified Seldinger Technique
During the webinar led by Roland van Rens, a leading expert in neonatal vascular access, the Modified Seldinger Technique (MST) was presented as a transformative solution. MST uses a micro-puncture needle, a soft guidewire, and a dilator to insert the catheter with minimal trauma and maximum precision.
Unlike traditional methods, where catheters are inserted directly through Short Peripheral Catheter (SPC) or steel or plastic splitable introducers; MST allows for a more controlled and less traumatic approach. It’s especially suited for fragile neonatal veins and is compatible with ultrasound guidance, improving accuracy and safety.
What MST Helps Us Avoid
Using inappropriate techniques can lead to a cascade of complications:
- Infiltration and extravasation
- Infections, especially when cannulas cannot be removed
- Occlusions, particularly in thinner neonatal PICCs
- Accidental removals due to poor fixation
- Catheter damage from steel needles
- Pain and stress for both patients and healthcare professionals
If we don’t carefully choose our VA devices and our methods to insert VA devices, we might create a Difficult Intravenous Access (DIVA) patient, where veins are depleted and access becomes increasingly difficult. This not only compromises care but also increases costs and emotional strain.
MST significantly reduces these risks. It’s less traumatic, more precise, and allows for longer catheter dwell times, meaning fewer procedures and less discomfort.
Backed by Data: Evidence That Validates MST
The MST isn’t just a promising innovation, it’s a solution grounded in robust clinical evidence. During the webinar, Roland van Rens presented compelling data from a large-scale retrospective cohort study conducted in a NICU in Doha, Qatar. The study spanned three years and analysed 1,445 catheter insertions, comparing conventional techniques with MST using a dedicated micro-insertion kit.
Key Findings from the Study
1. First-Attempt Success Rate
- Conventional technique: 88%
- MST: 91%
- This improvement, though seemingly modest, is clinically significant. In neonatal care, every additional attempt increases the risk of trauma, infection, and stress for the baby. A higher first-attempt success rate means fewer punctures, less pain, and faster access to therapy.
2. Complication Reduction
- Conventional technique: 39 complications
- MST: 8 complications
- The types of complications tracked included catheter damage, accidental removal, occlusions, leakage, infections, extravasation, and infiltration. MST’s design using a micro-puncture needle and soft guidewire minimizes vessel trauma and reduces the likelihood of these adverse events.
3. CLABSI Rate (Central Line-Associated Bloodstream Infections)
- Conventional technique: 3.45 per 1,000 catheter days
- MST: 1.06 per 1,000 catheter days
- This represents a 69% reduction in bloodstream infections, a critical metric in neonatal care. Lower CLABSI rates translate to improved patient outcomes, shorter hospital stays and reduced antibiotic use.
4. Catheter Longevity
- MST also contributed to longer catheter dwell times. With fewer complications and better insertion success, catheters remained functional for extended periods, reducing the need for repeated procedures and preserving venous access.
Global Validation
The webinar also referenced multiple international studies that support MST’s effectiveness:
- Song et al. (2018): Randomized controlled trial showing MST increased success rates from 65% to 83%.
- Gupta et al. (2021): Retrospective study with 100 catheters showing fewer punctures per successful insertion.
- Gibb et al. (2021): Retrospective study with 57 catheters showing an increase of first attempt, fewer punctures per successful insertion and cost effectiveness.
- Rodriguez et al. (2023): RCT showing clinical benefits, though not statistically significant.
- Zinni et al. (2024): Prospective study reporting 100% success with no complications.
- Van Rens et al. (2024): The Qatar study cited above, with the largest cohort and most comprehensive outcome analysis.
These studies collectively demonstrate that MST is not only effective in controlled environments but also adaptable across diverse clinical settings.
As W. Edwards Deming: “Without data, you’re just another person with an opinion.” MST brings the data and the results to back up its promise.
From Technique to Strategy: VAMP
Implementing MST is not just about switching tools, it’s about changing mindset. The webinar introduced the concept of a Vascular Access Management Plan (VAMP), built on the “7 Rights of Neonatal Vascular Access”:
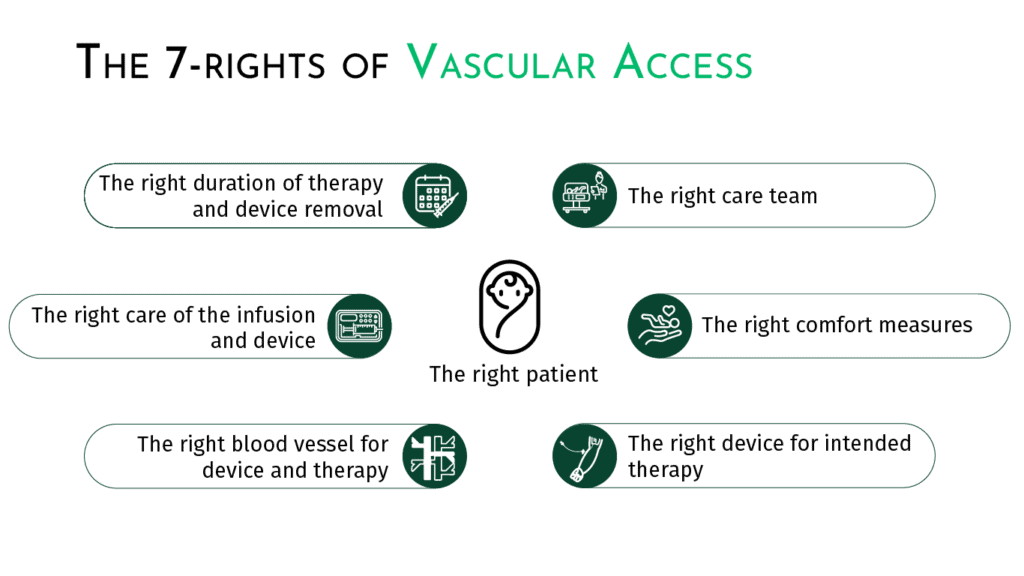
This proactive approach replaces reactive decisions made only when a catheter fails. With a global approach and a structured VAMP, teams can anticipate access needs, reduce complications, and improve the overall experience for patients, families, and healthcare professionals.
Training and Teamwork: The Key to Success
MST requires proper training. It’s not enough to have the right kit. You need the right skills. The webinar emphasized the importance of:
- Standardized training programs
- Hands-on training simulation
- Visualization of veins using ultrasound
A dedicated vascular access team including nurses, neonatologists, educators, and even parents can facilitate training, monitor outcomes, and drive continuous improvement.
Another study showed that introducing a specialized n-PICC team increased first-attempt success rates from 58.6% to 67.2%, and overall success from 81.7% to 97.6%. Therapy failure rates dropped from 7.4% to 4.8%.
What You Can Do Today
If you work in neonatal care, here’s how you can start making a difference:
- Evaluate your current practice: How many attempts does it take to insert a catheter? What complications are you seeing?
- Train your team: Organize MST workshops and simulations.
- Implement MST: Use neonatal-specific kits and follow the step-by-step protocol.
- Design a VAMP for each patient: Plan ahead instead of reacting to failures.
- Share your results: Track your data and celebrate improvements.
As W. Edwards Deming said: “It’s not enough to do your best; you must know what to do, and then do your best.”
MST is more than a technique, it’s a movement toward safer, smarter, and more compassionate neonatal care.
References
- Legemaat M, Carr PJ, van Rens RM, van Dijk M, Poslawsky IE, van den Hoogen A. Peripheral intravenous cannulation: complication rates in the neonatal population: a multicenter observational study. J Vasc Access. (2016) 17(4):360–5. doi: 10.5301/jva.50005582025-10
- Odom B, Lowe L, Yates C. Peripheral infiltration and extravasation injury methodology: a retrospective study. J Infus Nurs. (2018) 41(4):247–52. doi: 10.1097/NAN.00000000000002872025-10
- Van Rens MFPT, Hugill K, Mahmah MA, et al. Evaluation of unmodifiable and potentially modifiable factors affecting peripheral intravenous device-related complications in neonates: a retrospective observational study. BMJ Open. (2021) 11(9):e047788. doi: 10.1136/bmjopen-2020-0477882025-10
- Bayoumi MAA, van Rens MFPT, Chandra P, et al. Effect of implementing an Epicutaneo-Caval Catheter team in Neonatal Intensive Care Unit. J Vasc Access. (2021) 22(2):243–253. doi: 10.1177/11297298209281822025-10
- Van Rens MFPT, Hugill K, van der Lee R, et al. Comparing conventional and modified Seldinger techniques using a micro-insertion kit for PICC placement in neonates: a retrospective cohort study. Front Pediatr. (2024) 12:1395395. doi: 10.3389/fped.2024.13953952025-10
- Van Rens M, Ostroff M, Bayoumi MAA. The Modern Role of Neonatal PICCs Subspecialty. Nurs Crit Care. (2025) 30(4):e70111. doi: 10.1111/nicc.701112025-10
- McIntyre C, August D, Cobbald L, et al. Neonatal Vascular Access Practice and Complications: An Observational Study of 1,375 Catheter Days. J Perinat Neonatal Nurs. (2023) 37(4):332–339. doi: 10.1097/JPN.00000000000005892025-10
- D. August et al. Peripheral intravenous catheter practices in Australian and New Zealand neonatal units: A cross-sectional survey. Journal of Neonatal nursing. doi.org/10.1016/j.jnn.2019.03.002. (2019 October)
- Van Rens MFPT, Bayoumi MAA, van de Hoogen A, et al. The ABBA project (Assess Better Before Access): A retrospective cohort study of neonatal intravascular device outcomes. Front Pediatr. 2022;10:980725. (Published 2022 Nov 3). doi:10.3389/fped.2022.980725






