From delivery to the NICU, hospital to hospital and even unplanned home deliveries, neonatal transport is crucial for making sure babies receive the care they need at the right time, and at a unit suited to their needs. Maintaining normothermia during transport has its challenges though, and a 2023 study found up to one third of infants arriving at the destination hospitals are hypothermic1
Neonatal Hypothermia, A Worldwide Issue
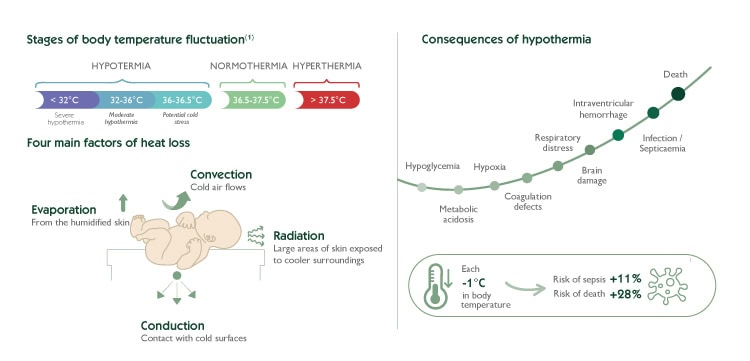
Neonates are particularly vulnerable to hypothermia due to their limited ability to regulate body temperature effectively and the fact that they can also be exposed to prolonged low temperatures. Hypothermia is an important factor in morbidity and mortality of all birthweights and gestational ages, and particularly for vulnerable preterm infants2.
Newborn admission temperature is a strong predictor of outcomes across all gestations3 as hypothermia can lead to a cascade of adverse effects, including respiratory distress, metabolic acidosis, and compromised immune function.
Therefore, ensuring optimal thermal management after birth is crucial in safeguarding the well-being and long-term outcomes of neonates
International recommendations
Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants
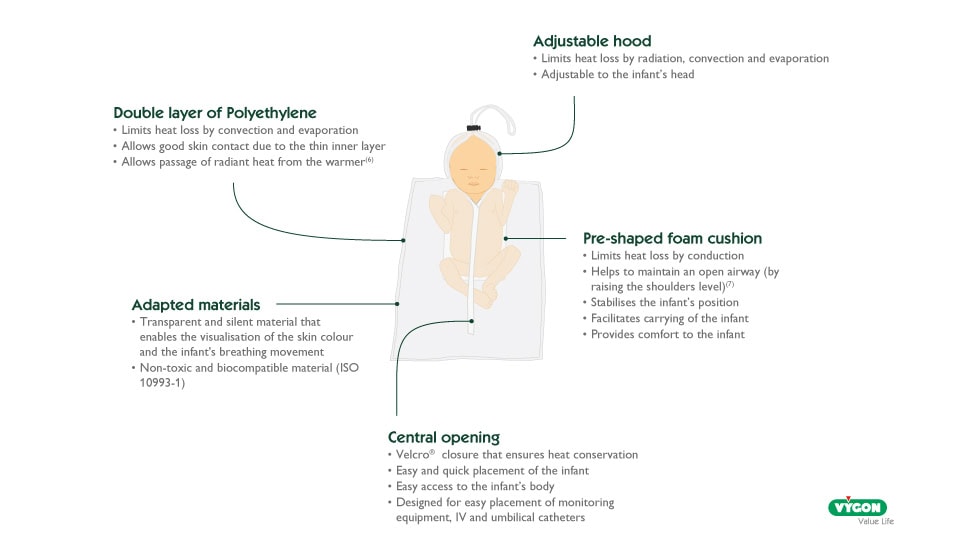
Use of an occlusive polyethylene transparent wrap or bag immediately at birth improved admission temperatures in non-randomised studies of infants at < 27 weeks’ gestation […], between 28 and 30, weeks […] and at < 33 weeks’ gestation […], as well as in very low birth weight infants and extremely low birth weight infants when compared with routine care
Cochraine Database of systematic reviews – 2018
Improvement in thermoregulation outcomes following the implementation of a thermoregulation bundle for preterm infants
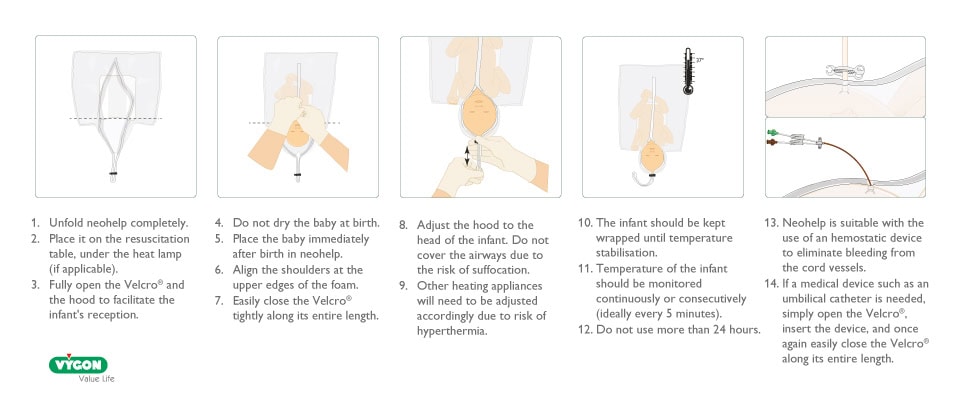
The key practice changes included: improved anticipation and staff preparedness, wrapping infant in a polyethylene sheet, using a polyethylene lined bonnet, using servo-control mode at birth and during transport.
Journal of Pediatrics and Child Health – 2022
When addressing hypothermia prevention, it is essential not to overlook thermal management during newborn transport. Indeed, without any implementation, transfer services are arriving to babies who are already hypothermic, and the transport environment makes it more challenging to warm them up, resulting in preterm infants reaching the destination hospital in hypothermia.
“These VLBW, ELBW, EGLAN and sometimes term neonates require transfer to tertiary centers for management and often hypothermic on reaching referral center due to lack of adequate precautions for hypothermia prevention during transport.”4
What care should be given to the newborn during the Golden Minute?
The use of a polyethylene plastic bag
To address the specific challenges to thermoregulation in the transport setting such as changing environment and limited ability to monitor and intervene 5, clinical evidence highlights the benefits of using a polyethylene plastic bag during transport:
- “Thermoregulation guideline included […] wrapping the infant in a polyethylene sheet […] and ensuring the infant was wrapped during transport and throughout the entire admission process in the NICU to maintain the thermal environment” 2
- “Placing VLBW infants in polyethylene plastic bags during transport reduces the occurrence of hypothermia […]” 6
- “The transport incubator used to limit heat loss can be cumbersome and difficult to obtain. It may be « replaced » by […] a transparent polyethylene bag wrapping whilst the baby is still wet. This greatly reduces the risk of hypothermia”7
- “The implementation of Velcro-closure polyethylene wrap was a helpful adjunctive tool that allowed a higher coverage of body surface area […]”5
Therefore, neonatal transfer services may implement the use of polyethylene plastic bags during transport to optimize thermal management in neonates.
The Importance of Preparation and Planning:
Nevertheless, effective thermal management during transport is part of a wide strategy and requires a multi-faceted approach:
- Anticipate the need for thermal support based on the infant’s gestational age and condition.
- Ensure that transport equipment is pre-warmed and readily available.
- Develop standardised protocols for thermal management during transport.
Optimal thermal control during neonatal transport requires a coordinated effort from all members of the healthcare team. This includes:
- Effective communication between referring and receiving facilities.
- Thorough training of transport personnel in thermal management techniques.
- Continuous quality improvement initiatives to monitor and enhance the effectiveness of thermal management protocols.
In conclusion, admission hypothermia can be reduced through the implementation of appropriate measures starting from the initiation of newborn transport. Therefore, thermoregulation should be considered among one of the key priorities for transport teams, with the ultimate goal of achieving and maintaining normothermia from birth for all patients.
Bibliography
- [1] Bird D, Edwards C. Improving thermoregulation for preterm babies weighing <1kg during hospital-to-hospital transportation, a novel use of delivery room equipment. KIDSNTS – Birmingham Women’s and Children’s Hospital – NHS Foundation Trust – Presented in 2023
- [2] Singh TS, Skelton H. Improvement in thermoregulation outcomes following the implementation of a thermoregulation bundle for preterm infants. J Paediatr Child Health. 2022 Jul
- [3] Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants, McCall EM, Alderdice F, Halliday HL, Vohra S, Johnston L Cochrane Database of Systematic Reviews 2018, Issue 2.
- [4] 2017_Golden Hour of neonatal life: need of the hour.
- [5] Glenn T, Price R. Improving thermoregulation in transported preterm infants: a quality improvement initiative. J Perinatol. 2021 Feb
- [6] Hu XJ, Wang L. Using polyethylene plastic bag to prevent moderate hypothermia during transport in very low birth weight infants: a randomized trial. J Perinatol. 2018 Apr
- [7] ) J.F.Diependaele, A.Fily. Management of a newborn baby-51st congress of French society of Anesthesia and Intensive Care-2009






