Advanced hemodynamic monitoring, particularly the ability to track stroke volume (SV) and cardiac output (CO), has significantly contributed to the refinement of anesthesiologists’ expertise in hemodynamic management. Beyond serving as cardiac output monitors, these devices incorporate advanced technologies that provide crucial hemodynamic parameters, aiding clinical decision-making. One of the most recent and comprehensive parameters, Cardiac Cycle Efficiency (CCE), reflects the cardiovascular system’s ability to maintain homeostasis at different energetic levels, influenced by pump function and the electro-mechanical interactions of all cardiovascular components.
Pure efficiency is near to 1; however, CCE is always less than 1, as a portion of the energy generated by the heart is inevitably lost during cardiac activity and cannot be fully recovered.

On the other hand, CCE may take negative values in vivo, reflecting the activation of compensatory mechanisms that provide support to dysfunctional cardiovascular compartments.1
CCE not only follows changes in SV but also assesses the mechanisms through which a given SV is achieved. As it evaluates contractility and afterload conditions together, it can also be considered as a surrogate hemodynamic parameter for ventriculoarterial coupling (VAC).
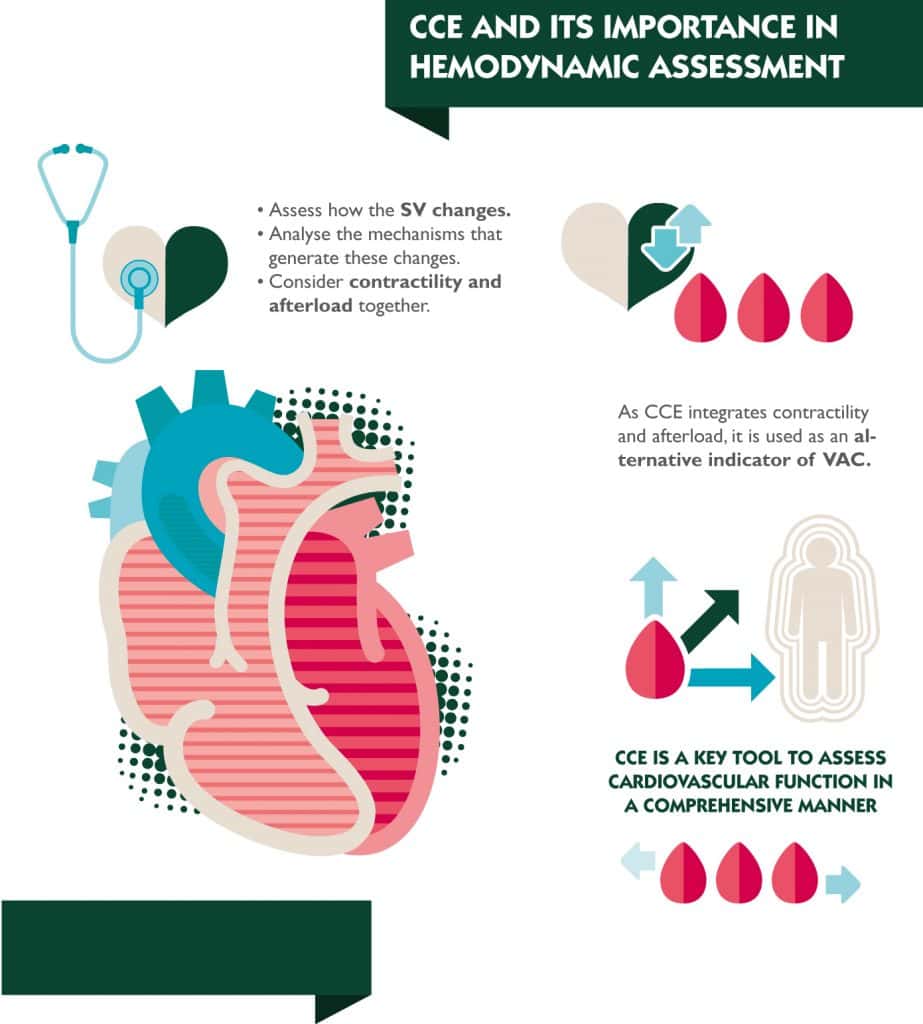
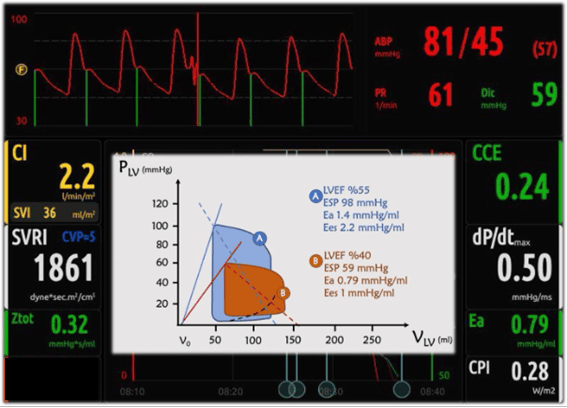
For instance, a patient with low CO and hypotension may still exhibit a positive CCE if afterload (Ea) is low, and contractility (dp/dtmax) is sufficient to generate a normal SV (Figure 1&2).
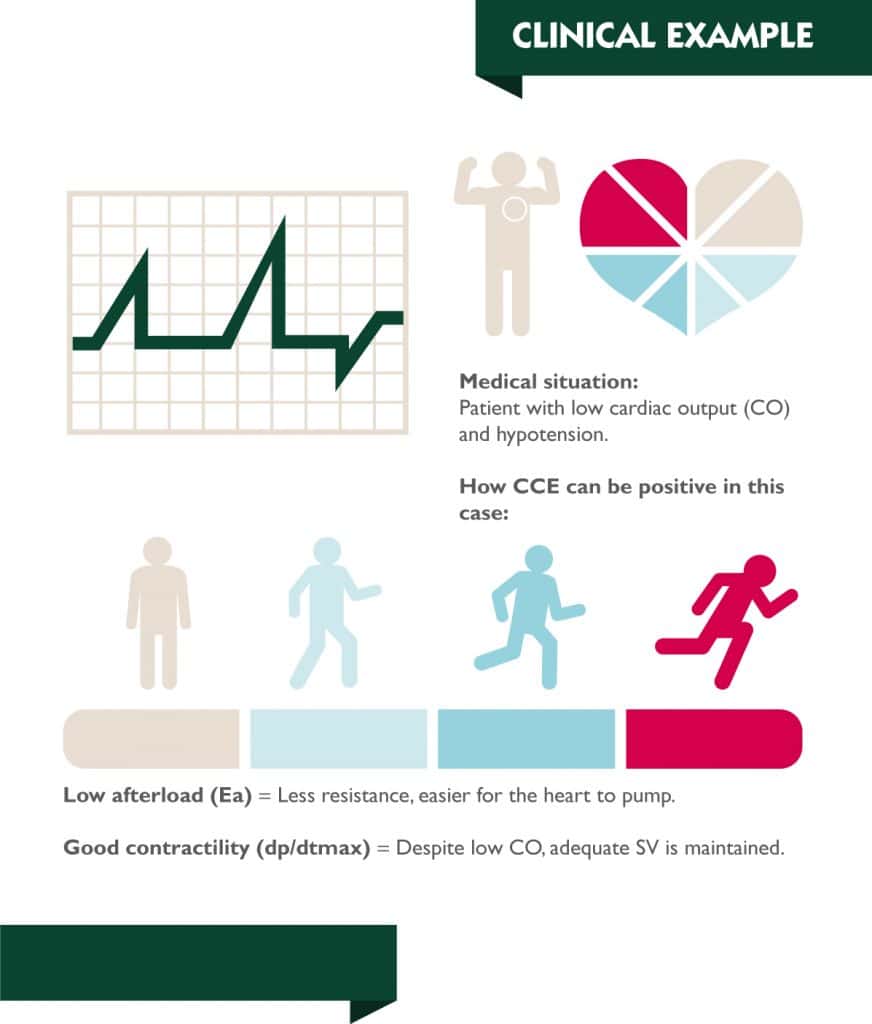
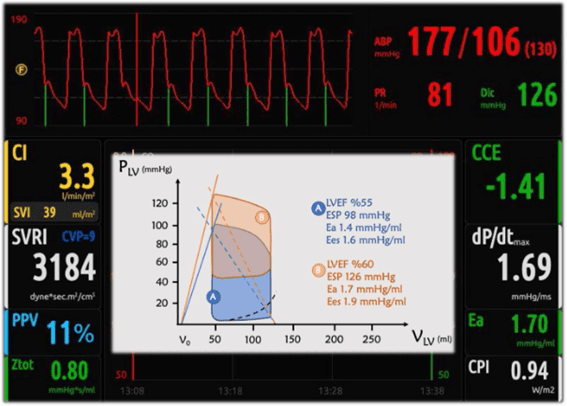
Conversely, if the ventricle compensates for increased afterload by augmenting contractility to maintain SV within normal limits, CCE may be negative even if CO remains within the normal range.
A major clinical advantage of CCE is its ability to differentiate between effective and inefficient treatment strategies. Consider a patient with tachycardia-induced low cardiac output and high afterload. Administering inotropes may transiently increase stroke volume and decrease afterload, thereby improving CO and mean arterial pressure (MAP). However, if tachycardia remains uncorrected, CCE will decline despite meeting conventional hemodynamic targets, as the system continues to expend excessive energy to sustain an unstable equilibrium. A more physiological approach correcting tachycardia to extend diastolic time, optimize stroke volume, and allow for natural afterload normalization would improve CCE, indicating a more energy-efficient cardiovascular state.
Recent studies support clinical relevance of CCE. It has been demonstrated that lower CCE values in pediatric cardiac surgery patients correlate with prolonged intensive care unit stays and increased inotropic requirements, emphasizing its prognostic value.2 Similarly, it has been found that when combined with arterial elastance, CCE enhances the assessment of fluid responsiveness, suggesting its utility in optimizing resuscitation strategies.3
A negative correlation between CCE and NT-proBNP levels has been identified, reinforcing its role as a marker for myocardial stress and ventricular function.4 The clinical applications of CCE extend from mechanical circulatory support to pharmacologic interventions. It has been shown that intra-aortic balloon counter pulsation improves CCE by reducing myocardial oxygen consumption while maintaining effective perfusion.5 Additionally, different anesthetic regimens have been reported to significantly alter CCE values, highlighting its potential role in tailoring pharmacologic therapy based on real-time hemodynamic assessments.6
Incorporating CCE into routine hemodynamic evaluations can provide a dynamic perspective on cardiovascular performance, surpassing static perfusion markers. Rather than confirming whether a hemodynamic target has been met, CCE offers valuable insight into whether the system is operating efficiently or expending excessive energy to maintain equilibrium. In this context, CCE emerges as a promising tool for hemodynamic management and various research endeavors by enabling the individualized interpretation of VAC and facilitating the development of energy-efficient therapeutic strategies.
BIBLIOGRAPHY
- Romano SM: Cardiac cycle efficiency: a new parameter able to fully evaluate the dynamic interplay of the cardiovascular system. Int J Cardiol 2012;155:326-327.
- Han D, Pan S, Li H, Meng L, Luo Y, Ou-Yang C: Prognostic value of cardiac cycle efficiency in children undergoing cardiac surgery: a prospective observational study. Br J Anaesth 2020;125:321-329.
- Messina A, Romano SM, Bonicolini E, et al.: Cardiac cycle efficiency and dicrotic pressure variations: new parameters for fluid therapy: An observational study. Eur J Anaesthesiol 2017;34:755-763.
- Scolletta S, Ranaldi G, Carlucci F, Franchi F, Romano SM, Biagioli B: Relationship between N-terminal pro-B-type natriuretic peptide (Nt-proBNP) and cardiac cycle efficiency in cardiac surgery. Biomed Pharmacother 2010;64:511-515.
- Gelsomino S, Romano SM: Cardiac cycle efficiency during counterpulsation. J Thorac Cardiovasc Surg 2013;145:889-890.
- Han D, Liu YG, Pan SD, Luo Y, Li J, Ou-Yang C: Comparison of sufentanil-midazolam and sevoflurane for anesthesia induction in children undergoing cardiac surgery by real-time hemodynamic and cardiac efficiency monitoring: A prospective randomized study. Heart Surg Forum 2019;22:E038-e044.