Hemodynamic instability frequently manifests during the perioperative course of high-risk surgical patients. This instability arises primarily during surgery due to the influence of anesthetic agents on vascular tone, compounded by surgical bleeding. Post-surgery, various factors may be responsible for hemodynamic instability, including hemorrhagic complications, cardio-respiratory adverse events (such as myocardial infarction and pulmonary embolism), and infectious complications (e.g. septic shock). Hemodynamic instability can precipitate tissue hypoperfusion and hypoxia, and if prolonged, may culminate in organ failure, ultimately leading to postoperative mortality.
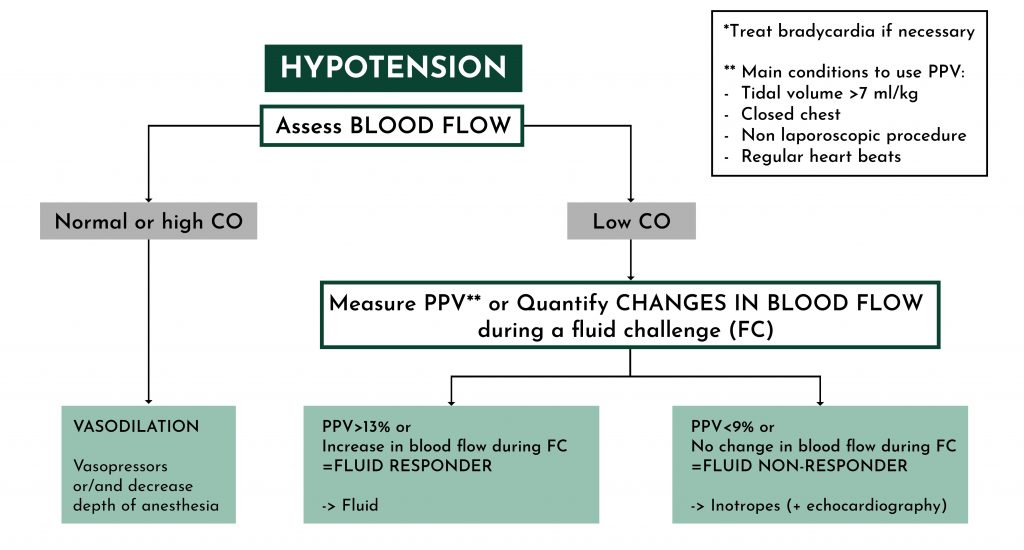
output; PPV, pulse pressure variation.
Rational hemodynamic management requires quantifying cardiac output and vascular tone to identify the underlying mechanisms of hemodynamic instability and select the right treatment (Figure 1). In patients with hypotension and preserved cardiac output, the underlying mechanism is vasodilation, and the logical treatment is the administration of vasopressors and, when possible, a reduction in the depth of anesthesia. In patients with hypotension and low cardiac output, hypotension is frequently related to hypovolemia. So that, fluid administration will result in a significant increase in cardiac output. If this is not the case, cardiac dysfunction is suspected. Of note, a low cardiac output may occasionally be explained by extreme bradycardia (heart rate < 40 bpm).
Most patients undergoing major surgery are monitored with a radial arterial catheter for continuous blood pressure monitoring. In this context, pulse contour algorithms enable the continuous monitoring of cardiac output and vascular tone. Some pulse contour algorithms work exclusively with expensive and bulky disposable pressure transducers. In Europe, the carbon dioxide emissions and cost associated with these dedicated transducers may exceed 1000 tons/yr and 1 billion euros/yr, respectively.1 Other pulse contour algorithms (including the PRAM) work with regular pressure transducers, drastically reducing carbon dioxide emissions and costs. They are part of cardiac output monitoring systems known as green
pulse contour techniques.2
In summary, all patients undergoing major surgery monitored with a radial arterial catheter should benefit from cardiac output monitoring with a green pulse contour technique.
REFERENCES
- Michard F, Romagnoli S, Saugel B. Make my hemodynamic monitor GREEN: sustainable monitoring
solutions. Br J Anaesth 2024; Online ahead of print - Michard F, Futier E, Desebbe O, et al. Pulse contour techniques for perioperative hemodynamic monitoring:
A nationwide carbon footprint and cost estimation. Anaesth Crit Care Pain Med 2023, 42:101239.






