Neonatal care often necessitates reliable vascular access for the administration of parenteral nutrition, medications, and other critical therapies. The Modified Seldinger Technique (MST) has emerged as a valuable method for inserting neonatal Peripherally Inserted Central Catheters (n-PICCs), addressing many challenges inherent in traditional approaches. Recent studies underscore MST’s potential advantages over conventional techniques, including improved success rates, reduced complications, and enhanced patient outcomes.
Advantages of MST Over Traditional Techniques
Traditional methods for catheter insertion, such as the Split Needle Technique (SNT) or peelable cannula techniques, often face limitations in neonates due to the fragility of their blood vessels and the need for repeated attempts in cases of failure. These techniques also carry risks of vein transfixation, fluid diffusion, or early reduction of venous capital. Furthermore, they can lead to complications such as catheter damage, making repeated procedures necessary, thereby increasing patient stress and pain as well as the caregivers’ workload.
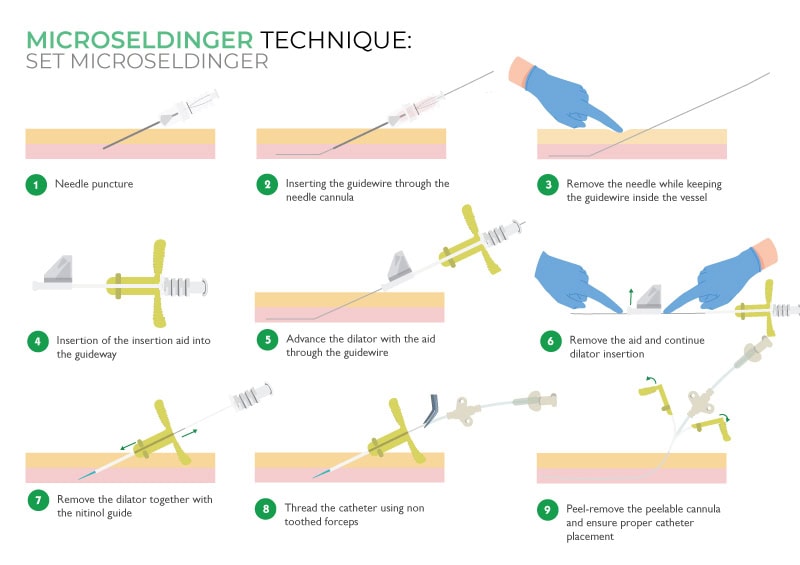
The MST, adapted from the classic Seldinger technique, involves the use of a small-gauge needle, a flexible guidewire, a dilator, and a peelable cannula. This method minimizes trauma to the vessel wall and enables the insertion of 1 to 2 Fr catheters in even the smallest and most superficial veins. MST has demonstrated a superior ability to preserve vascular integrity and facilitate first-attempt success, particularly in fragile neonatal patients. This is especially critical in very low birth weight infants, where maintaining intact vascular access is paramount.
Key Findings from Recent Studies
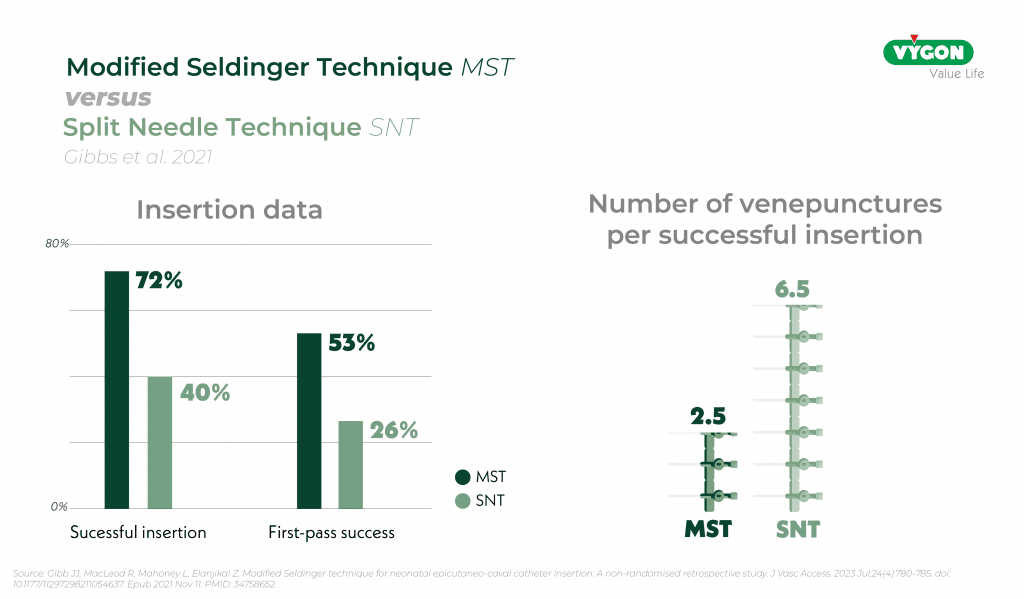
Study by Gibb et al. (2021)1
A retrospective comparison of the Modified Seldinger Technique (MST) and Split Needle Technique (SNT) for n-PICCs placement demonstrated a higher success rate with the MST technique, along with a reduced number of venipunctures. This decrease in the number of insertion attempts also helped reduce stress in premature infants, thereby improving their overall care.
Study by Van Rens et al. (2024)2
An observational study conducted over three years compared the MST technique to conventional insertion techniques. The results demonstrated higher insertion success rates, a reduction in catheter-related complications, including a significantly lower incidence of catheter-associated bloodstream infections (CLABSI).
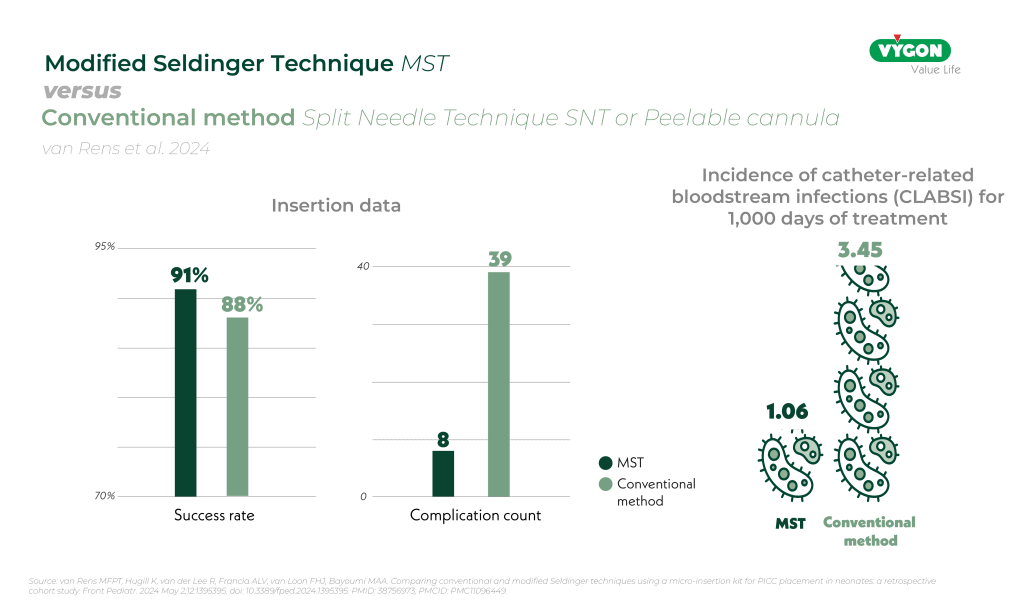
MST was associated with fewer therapy interruptions and a reduced risk of catheter failure, reinforcing its effectiveness in minimizing procedural complications and patient distress. Thanks to MST, workflows have been improved, with a progressive reduction in procedural complexity and an increase in practitioners’ confidence with continued use.
Clinical Implications
MST represents a critical advancement in neonatal vascular access. By reducing venepunctures and associated complications, MST improves neonatal outcomes by:
- Minimizing procedural pain and stress.
- Lowering the risk of CLABSI and other infections.
- Preserving venous sites for future access.
- Enhancing first-attempt success rates, particularly in neonates with difficult intravenous access (DIVA), where conventional methods frequently fail.
Additionally, MST contributes to the improvement of care delivery efficiency and patient management for hospital staff. By reducing the number of venepunctures and associated complications, MST decreases the time and resources required for repeated attempts and management of complications. This allows healthcare professionals to allocate their time more effectively, enhancing overall workflow and patient care quality.
Recommendations and Future Directions
The evidence strongly supports broader adoption of MST in Neonatal Intensive Care Units (NICUs). However, successful integration depends on:
- Standardized training programs ensuring technical proficiency.
- Availability of micro-insertion kits specifically designed for neonates.
- Establishment of multidisciplinary vascular access teams to uphold best practices and drive quality improvement, as demonstrated in the study by Van Rens et al.
Future research should focus on:
- Randomized controlled trials to further validate MST’s benefits.
- Evaluating cost-effectiveness and long-term vascular health outcomes.
- Exploring the integration of ultrasound guidance for enhanced catheter placement precision.
- Assessing the impact of infection control bundles and advanced line-securing techniques, such as tissue adhesives, in conjunction with MST.
- Expanding MST’s use in preterm neonates with extremely low birth weight, where the margin for error is smallest and traditional techniques often fail.
Conclusion
The Modified Seldinger Technique offers a safer, more effective approach for neonatal catheter insertion, by avoiding limitations of traditional methods. By improving success rates, reducing complications, and enhancing patient outcomes, MST is emerging as a gold standard in neonatal vascular access. Ongoing education, research, and technological integration will be essential to unlocking its full potential. As MST continues to gain traction, its role in setting new benchmarks for excellence in neonatal care becomes increasingly clear.
Beyond its immediate clinical benefits, the adoption of MST represents a broader commitment to improve neonatal care standards. By fostering collaboration between healthcare professionals, optimizing training programs, and integrating emerging technologies, MST can drive significant improvements in neonatal vascular access.
Would you like to learn more about the use of this technique in neonatology?
Bibliography
- Gibb JJ, MacLeod R, Mahoney L, Elanjikal Z. Modified Seldinger technique for neonatal epicutaneo-caval catheter insertion: A non-randomised retrospective study. J Vasc Access. 2023 Jul;24(4):780-785. doi: 10.1177/11297298211054637
. Epub 2021 Nov 11. PMID: 34758652
.
- van Rens MFPT, Hugill K, van der Lee R, Francia ALV, van Loon FHJ, Bayoumi MAA. Comparing conventional and modified Seldinger techniques using a micro-insertion kit for PICC placement in neonates: a retrospective cohort study. Front Pediatr. 2024 May 2;12:1395395. doi: 10.3389/fped.2024.1395395
. PMID: 38756973
; PMCID: PMC11096449.






