In 30.7% of cases, the arterial blood pressure waveform is resonant. If this happens, the reading will be incorrect and, if we base our decisions on it, they will not be the most accurate.
WHAT WILL YOU FIND IN THIS ARTICLE?
- What is resonance?
- How to avoid resonance?
- Tools: electronic dynamic filter
Do you want to know how to avoid resonance in the arterial blood pressure waveform? Stay on this page and read the full entry.
According to studies, in 30.7% of cases, the arterial pressure waveform shows resonance.2
Hemodynamic monitoring is an essential tool in critically ill patients, but… What happens when the blood pressure waveform has artefacts?
A damped or resonant blood pressure waveform will lead to an incorrect blood pressure reading and, if we base our decisions on it, they will not be the most accurate.
In this article we will learn keys and tools to prevent our arterial blood pressure waveform from being resonant and, in this way, to know the hemodynamic status of our patient and to be able to apply an optimal and individualized treatment.
ARTERIAL BLOOD PRESSURE WAVEFORM
The arterial pressure wave is the consequence of the interaction between the stroke volume, the ejection volume of the left ventricle, and the physical characteristics of the cardiovascular system at each beat.
It is a mechanical wave, similar to sound, and is therefore only transmitted through physical means. It is cylindrical in shape, starting from the heart and travelling along a wave front through the arteries until it reaches the arterioles. This wave passes through a viscous medium, blood, and a much less viscous medium, the saline, to the transducer.
After applying a Pulse Contour Method algorithm to the morphology of the arterial pressure waveform, it is possible to obtain information that allows clinicians to analyze the cardiovascular status of patients.
In order to identify artefacts in the arterial pressure wave, it is essential to know its shape and parts. To a greater or lesser extent, every blood pressure waveform must consist of 6 points:
- Systolic rise.
- Systolic blood pressure.
- Systolic fall.
- Dicrotic point. This is one of the most important parts as it represents the closure of the aortic valve and divides the cardiac cycle between systole and diastole.
- Diastolic descent.
- Diastolic blood pressure.
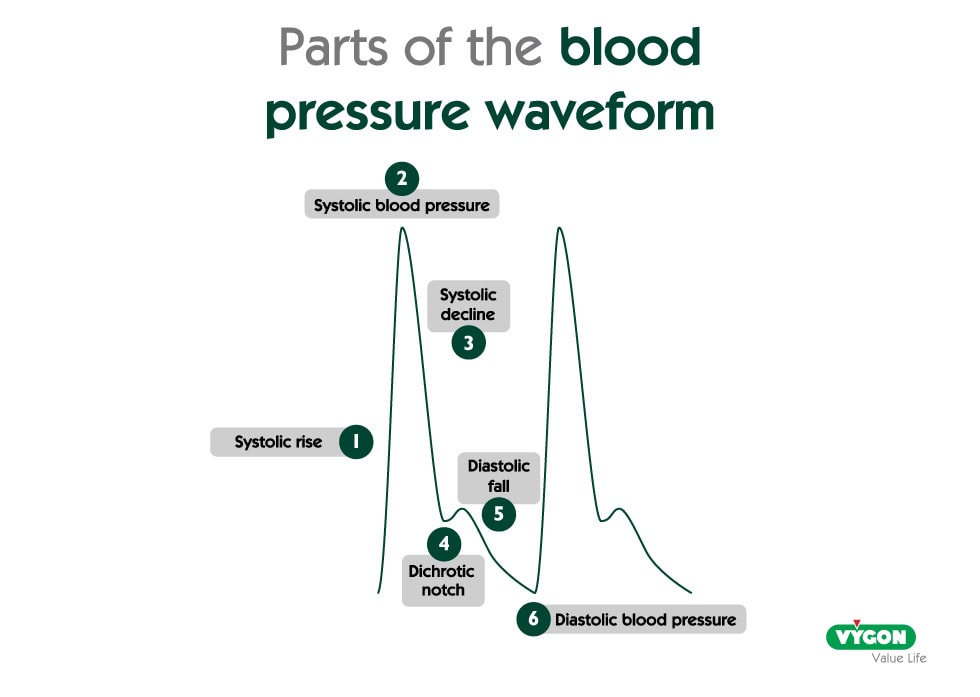
Resonance can alter its morphology, so knowing its parts will allow us to quickly identify artefacts.
WHAT IS RESONANCE?
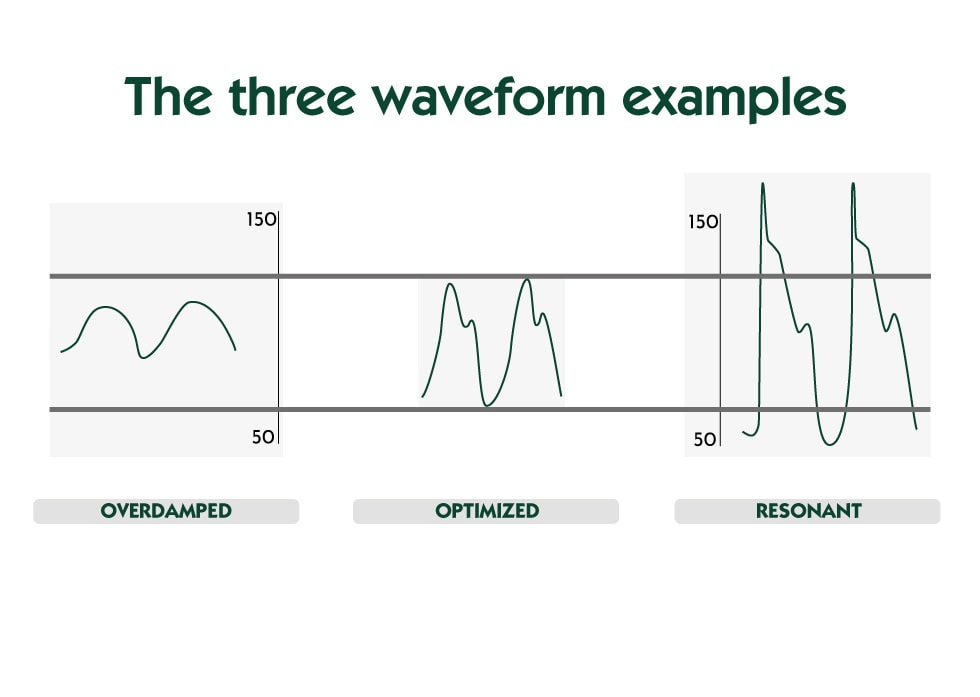
When we look at a resonant blood pressure waveform, we find oscillations that are very sharp and that may lead to an overestimated systolic pressure and/or a lower estimated diastolic pressure values, while the dicrotic notch is usually well visible and pronounced.
IS MY BLOOD PRESSURE WAVEFORM RESONANT?
There are a number of maneuvers that can be performed to determine if the invasive arterial blood pressure waveform (ABP) is reliable:
- If dP/dt> 1.7 mmHg/msec, it invites us to suspect that the signal presents resonance phenomena (also called underdamping)2
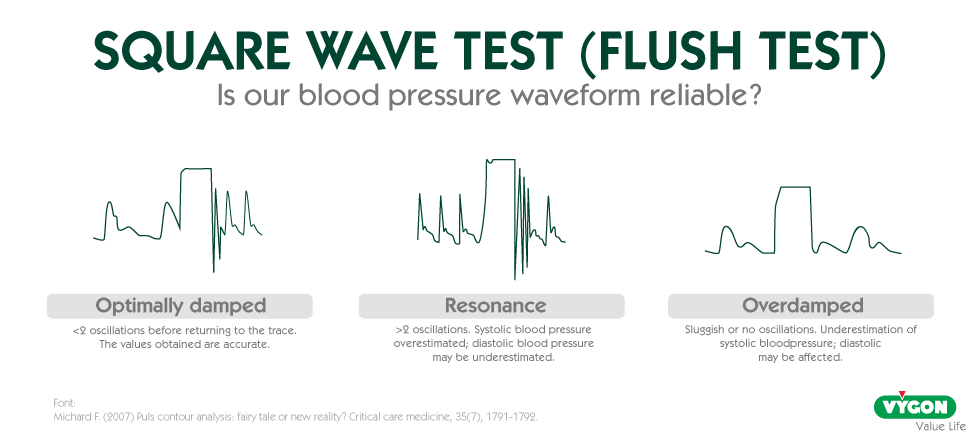
- Square wave test (Flush test): depending on the number of oscillations, resonance or overdamping phenomena can be suspected. Thus:
- Few oscillations follow the release of the flush value before reaching the normal trace the values obtained are accurate: this is a sign of adequately damped arterial waveform. >2 oscillations may be a sign of resonance, resulting in overestimated systolic pressure and underestimated diastolic pressure values.
- Sluggish or no oscillations, in this case the waveform may be damped with underestimation of systolic pressure and where diastolic pressure may be unaffected.
4 KEYS TO AVOID RESONANCE PHENOMENA
To avoid resonance phenomena, we must take into account different devices that are part of the blood pressure system.
1. APPROPRIATE ARTERIAL CATHETER
A catheter of appropriate length, diameter and material should be used.
Polyethylene is an intermediate material in terms of hardness and memory, so, being relatively rigid and not very heat-sensitive, it allows for good transmission of the blood pressure wave over time.
2. CATHETER PLACEMENT
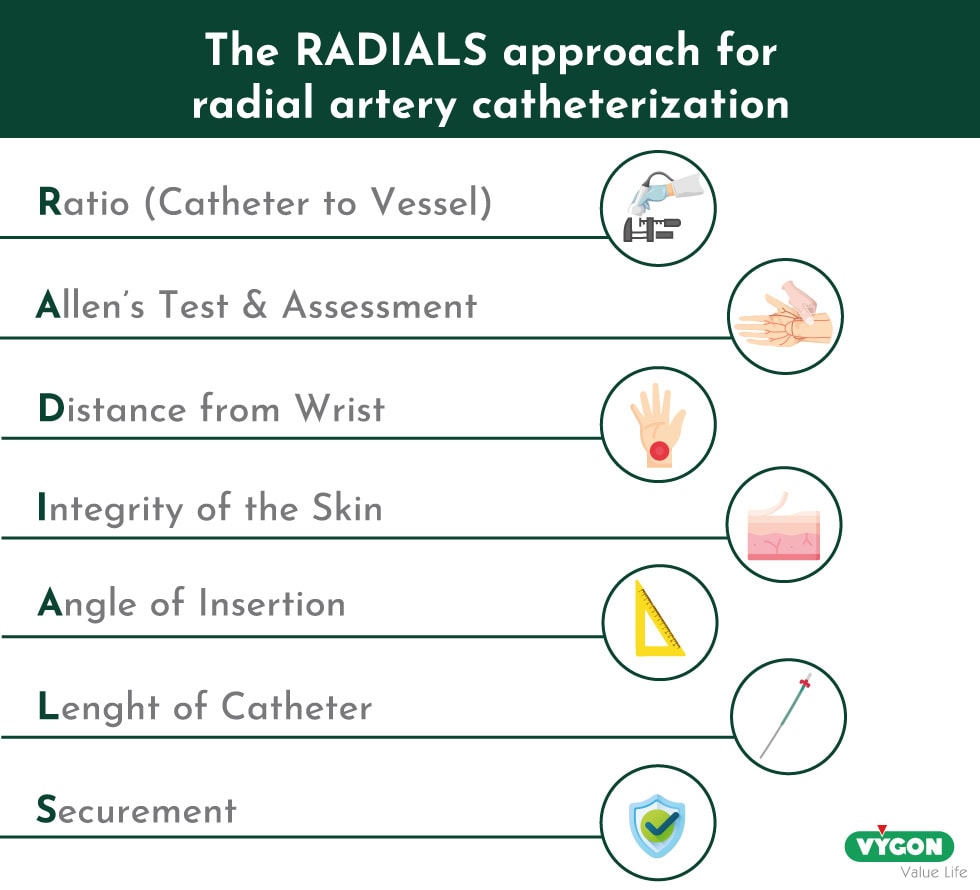
In Europe, an average of 2.5 million arterial lines are placed each year. However, like any technique or procedure, it is not free from complications. In order to avoid them, there are some good practices that we can incorporate like the RADIALS approach for radial artery catheterization:
- Ratio (Catheter to Vessel): Measure the arterial vessel diameter & maintain a CVR<45%.
- Allen’s Test & Assessment: Assess region & evaluate for collateral circulation.
- Distance from Wrist: Insertion site >4cm proximal from wrist crease & avoid areas of flexion.
- Integrity of the Skin: Inspect wrist & forearm for any redness, bleeding, hematoma or localized swelling.
- Angle of Insertion: Measure vessel depth and insert with ultrasound <30º. Avoid angles >45º.
- Length of Catheter: Consider total catheter length, relative to artery depth & angle of insertion.
- Securement: Stabilization & securement to prevent inadvertent catheter removal or dislodgment. Avoid sutures.
3. GOOD QUALITY TRANSDUCER ADAPTED TO THE PATIENT
Monitoring systems are characterized by the natural frequency, which quantifies how fast the system oscillates and will generate possible resonance phenomena; and the attenuation coefficient, which quantifies the friction forces acting on the system and determines how quickly it returns to rest, generating possible damping phenomena.
4. DAMPENING OPTIMIZATION
There are hemodynamic monitors currently in the market that already have an automatic internal software recognizing and optimizing resonance. A dynamic electronic filter is available in the P.R.A.M. method, which has been validated and tested in studies demonstrating its usefulness in eliminating resonance. 1
The software automatically analyses specific features of the pressure waveform and, when necessary, applies a filter to optimize the signal. Once activated, it automatically and continuously corrects the resonance in the arterial pressure waveform. 1
BIBLIOGRAPHY
- Foti L, Michard F, Villa G, Ricci Z, Romagnoli S. The impact of arterial pressure waveform underdamping and resonance filters on cardiac output measurements with pulse wave analysis. Br J Anaesth. 2022 Jul;129(1):e6-e8. doi: 10.1016/j.bja.2022.03.024. Epub 2022 Apr 19. PMID: 35459533.
- Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, Romano SM, De Gaudio AR. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Crit Care. 2014 Nov 30;18(6):644. doi: 10.1186/s13054-014-0644-4. PMID: 25433536; PMCID: PMC4279904.






