Catheterisation of an arterial line for invasive blood pressure monitoring is a common technique, both in Critical Care Units and in the intra- and postoperative period of patients undergoing cardiac or other major surgery requiring strict blood pressure control or repeated blood sampling.
Radial artery cannulation is considered the gold standard in most pediatric patients and although the use of ultrasound has seen a large increase in the last ten years, many practitioners still continue to use the palpation technique.
Recent studies show that the use of ultrasound may improve the success rate and reduce the incidence of complications such as hematomas in pediatric patients.
STEPS FOR ULTRASOUND-GUIDED ARTERIAL CANNULATION
1. TRANSDUCER PLACEMENT
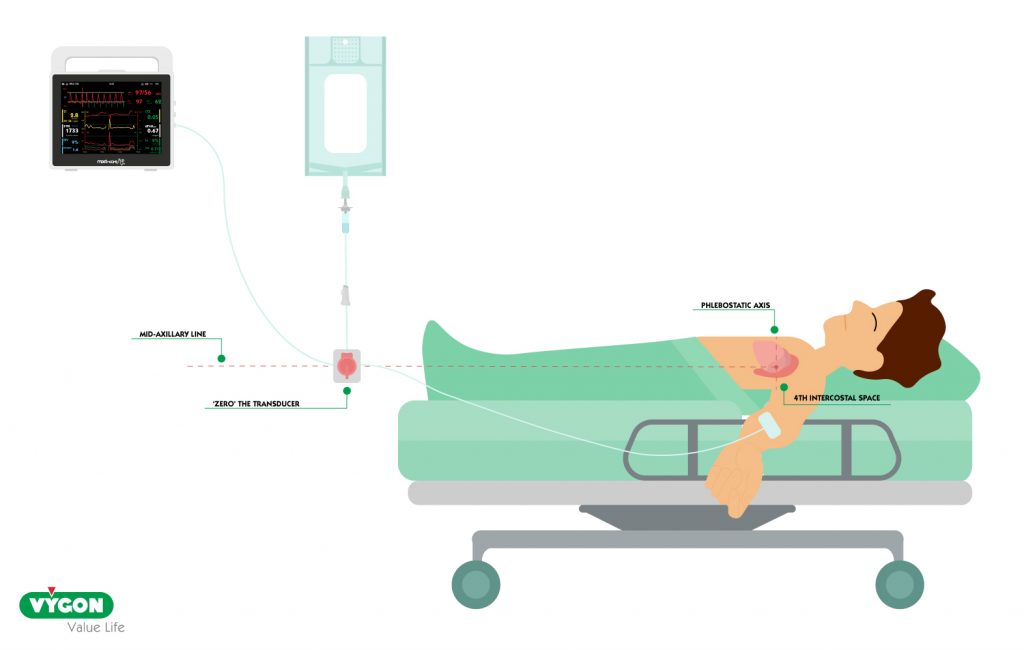
The transducer will be responsible for converting the mechanical signal from our catheter into an electrical digital signal that will provide us with a record on the monitor.
It must be inserted into the system in a vertical position as shown in the image.
2. PATIENT AND OPERATOR POSITION
We will focus on cannulation of the radial artery, as it is the first choice.
The patient under general anesthesia with endotracheal intubation, sedation, or laryngeal mask, will be positioned in supine decubitus with the arm selected for the technique in partial abduction.
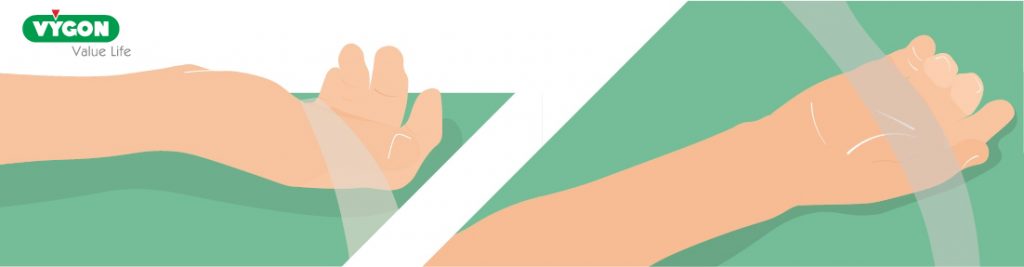
A slight dorsal flexion may be performed to facilitate access, but it is not recommended that this be forced as is often done, as it is possible that the catheter may bend and, when the hand is returned to its normal position, the invasive blood pressure value may not be reliable. It is also recommended not to puncture in a very distal area to allow greater mobility and comfort for the patient.
To perform the left radial artery approach, if the operator is right-handed, he shall position himself on the left side of the patient facing the patient’s head. In this way, the skilled hand will be used to cannulate the radial artery and the left hand will hold the ultrasound probe.
If the right artery is to be cannulated, the operator will position himself at the patient’s bedside so that he can perform the procedure with his skilled hand. If the operator is left-handed, he/she will be positioned in the opposite position.
The ultrasound machine should always be positioned in front of the operator to optimise visual and manual coordination during the procedure.
3. CHOICE OF CANNULATION SITE AND VERIFICATION OF VESSEL PATENCY
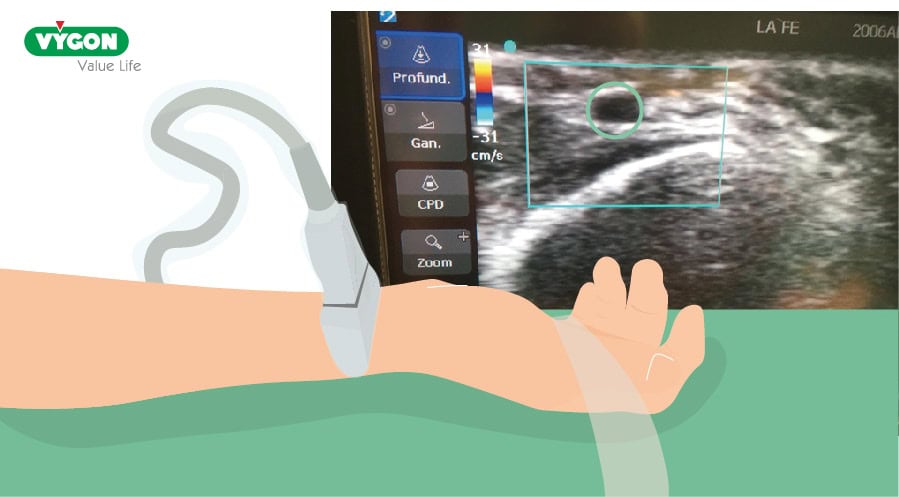
A scan of the antebrachial region on both sides is recommended in order to choose the optimal puncture site.
The sonoanatomy of the veins, arteries and adjacent structures must be recognised, possible anatomical variants identified and the patency of the vessel verified by detecting the presence of intraluminal thrombi with color and pulsed Doppler.
Similarly, using ultrasound, we will check the collateral flow before starting to cannulate the artery.
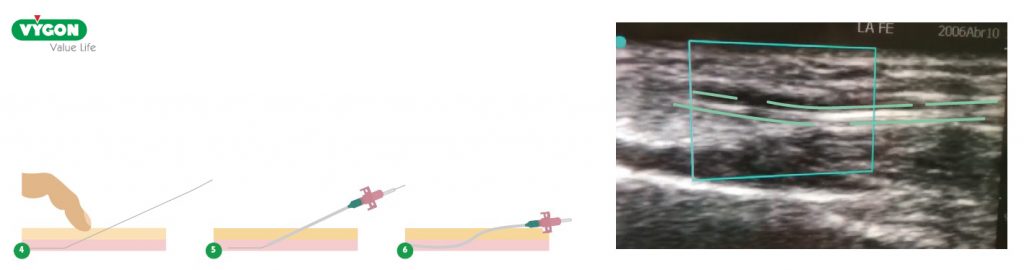
4. PERFORM ‘IN PLANE’ ULTRASOUND-GUIDED PUNCTURE OF THE RADIAL ARTERY
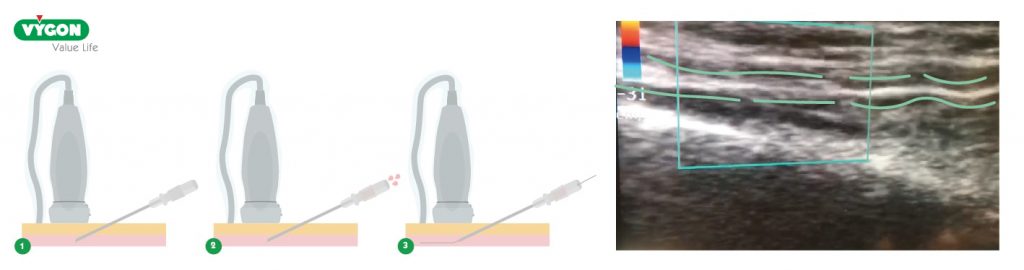
It is recommended to cannulate in plane, as although it is technically more difficult, it is always more reliable than cannulating out of plane.
Cannulation in plane allows better observation of the entry of the needle into the artery, in addition to being able to observe if any complications arise, such as the appearance of a hematoma or dissection of the arterial wall when passing the guidewire.
The steps to perform the ultrasound-guided cannulation in plan are as follows:
- Position the ultrasound machine in front of the operator.
- Flush the catheter with physiological solution on a table with a sterile field.
- Perform asepsis of the skin in the region to be cannulated and place sterile fields. Cover the 6-13 MHz linear probe with a sterile polyethylene sheath and place gel inside it to improve the interface.
- Scan the forearm region by placing the probe perpendicular to the forearm at the outer third level to obtain a short axis view of the radial artery. Slide the probe along the radial artery towards the elbow.
- Once the artery and puncture site have been identified, it is recommended, whenever possible, to turn the ultrasound probe 90° and perform the puncture ‘in plane’.
- After cannulating the artery and observing the pulsatile flow through the needle, proceed to advance the guidewire gently.
5. VERIFY THE CORRECT POSITION OF THE FIXATOR INSIDE THE RADIAL ARTERY
Once the artery is cannulated, the guidewire is slid through the needle and the correct location inside the artery is verified with ultrasound using the same ‘long axis’ view.
If we find any resistance to the passage of the guide, we can withdraw it a few millimetres and try to reintroduce it by rotating it slightly to facilitate its entry, as well as rotating the needle to try to find a better angle of entry into the vessel, taking into account the direction of the bevel.
6. VERIFY THE CORRECT POSITION OF THE CATHETER INSIDE THE RADIAL ARTERY
Once we have checked the correct positioning of the guidewire inside the artery, we remove the needle and introduce the catheter through the guidewire, removing it later.
We will use ultrasound to check its correct position in the artery in its long axis. In addition, we will obtain a pulsatile flow of oxygenated blood through the catheter, so we will be sure that it is working correctly. Finally, we will connect the catheter to the pressurised drip line at 300 mmHg and perform the ‘zero’ on the monitor.
Although the use of ultrasound for cannulation of peripheral arterial accesses is not widespread, both meta-analyses and clinical practice show its great usefulness, increasing the probability of success in the first attempt and decreasing the rate of complications.
BIBLIOGRAPHY
- Bardin-Spencer, A. J., y Spence, T. R. (2020). Arterial insertion method: A new method for systematic evaluation of ultrasoundguided radial arterial catheterization. The Journal of Vascular Access. https://journals.sagepub.com/doi/10.1177/1129729820944104
- Davies, G. (2018). Transductores arteriales y amortiguamiento. Curso de actualización en Anestesia Parte I. Universidad de Ciudad del Cabo.
- Esper, S. A., & Pinsky, M. R. (2014). Arterial waveform analysis. Best practice & research. Clinical anaesthesiology, 28(4), 363–380. https://doi.org/10.1016/j.bpa.2014.08.002
- Gershengorn, H. B., Garland, A., Kramer, A., Scales, D. C., Rubenfeld, G., & Wunsch, H. (2014). Variation of arterial and central venous catheter use in United States intensive care units. Anesthesiology, 120(3), 650–664. https://doi.org/10.1097/ALN.0000000000000008
- Imbrìaco, G., Monesi, A. Y Spencer, T. R. (2022). Preventing radial arterial catheter failure in critical care — Factoring updated clinical strategies and techniques. Anaesthesia Critical Care and Pain Medicine, 41.
- Lamperti M, Biasucci DG, Disma N, et al. (2020). European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur J Anaesthesiology (EJA), 37(5), 344-376
- Muller, J. C., Kennard, J. W., Browne, J. S., Fecher, A. M., & Hayward, T. Z. (2012). Hemodynamic monitoring in the intensive care unit. Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition, 27(3), 340–351. https://doi.org/10.1177/0884533612443562
- O’Grady, N. P., Alexander, M., Burns, L. A., Dellinger, E. P., Garland, J., Heard, S. O., Lipsett, P. A., Masur, H., Mermel, L. A., Pearson, M. L., Raad, I. I., Randolph, A. G., Rupp, M. E., Saint, S., & Healthcare Infection Control Practices Advisory Committee (HICPAC) (2011). Guidelines for the prevention of intravascular catheter-related infections. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 52(9), e162–e193. https://doi.org/10.1093/cid/cir257
- Rinehart, J. Et al. (2020). Detection of arterial pressure waveform error using machine learning trained algorithms. Journal of Clinical Monitoring and Computing, 36, 227-237. https://doi.org/10.1007/s10877-020-00642-4
- Romagnoli, S. et al. (2014). Critical Care, 18:664. http://ccforum.com/content/18/6/644
- Thomsen, K. K., Kouz, K., & Saugel, B. (2023). Pulse wave analysis: basic concepts and clinical application in intensive care medicine. Current opinion in critical care, 29(3), 215–222. https://doi.org/10.1097/MCC.0000000000001039
- Foti, L., Michard, F., Villa, G., Ricci, Z., & Romagnoli, S. (2022). The impact of arterial pressure waveform underdamping and resonance filters on cardiac output measurements with pulse wave analysis. British journal of anaesthesia, 129(1), e6–e8. https://doi.org/10.1016/j.bja.2022.03.024






