As some of the commonly recommended strategies for managing difficult airways are not optimal in the context of COVID-19, the Society for Airway Management (SAM) decided to take action. To this end, it has set up a task force to review existing literature and current clinical practice guidelines from the American Society of Anaesthesiologists (ASA). Its aim is tooptimize successful airway management while minimizing risk exposure for healthcare professionals.
The key points are as follows:
- The SARS-CoV-2 coronavirus, responsible for COVID-19, is spread via respiratory droplets. Mask ventilation, intubation and extubation of patients put healthcare personnel at risk.
- COVID-19 often causes severe hypoxemia requiring airway management.
- Unexpected airway difficulty can increase the risk of infection for caregivers if multiple attempts or multiple responders are required.
NON-ANATOMICAL CONSIDERATIONS
An airway difficulty may be due to the inability to ventilate, oxygenate, intubate or any combination of these. The incidence of airway difficulty may be increased by anatomical, physiological and contextual considerations.
Since not all COVID-19 patients have anatomical or physiological factors predictive of respiratory difficulties, it’s important to provide adequate preparation to reduce the risk of exposure and complications.
RISK OF AEROSOLIZATION, PURIFICATION AND INTUBATION EQUIPMENT
During airway management, endotracheal intubation and extubation are aerosol-generating procedures.
For patients whose airways are difficult to access, management can take longer. This means more healthcare professionals and more aerosol-generating procedures. To minimize the number of professionals in the patient’s room, the intubation team must be made up of highly qualified and strictly necessary personnel.
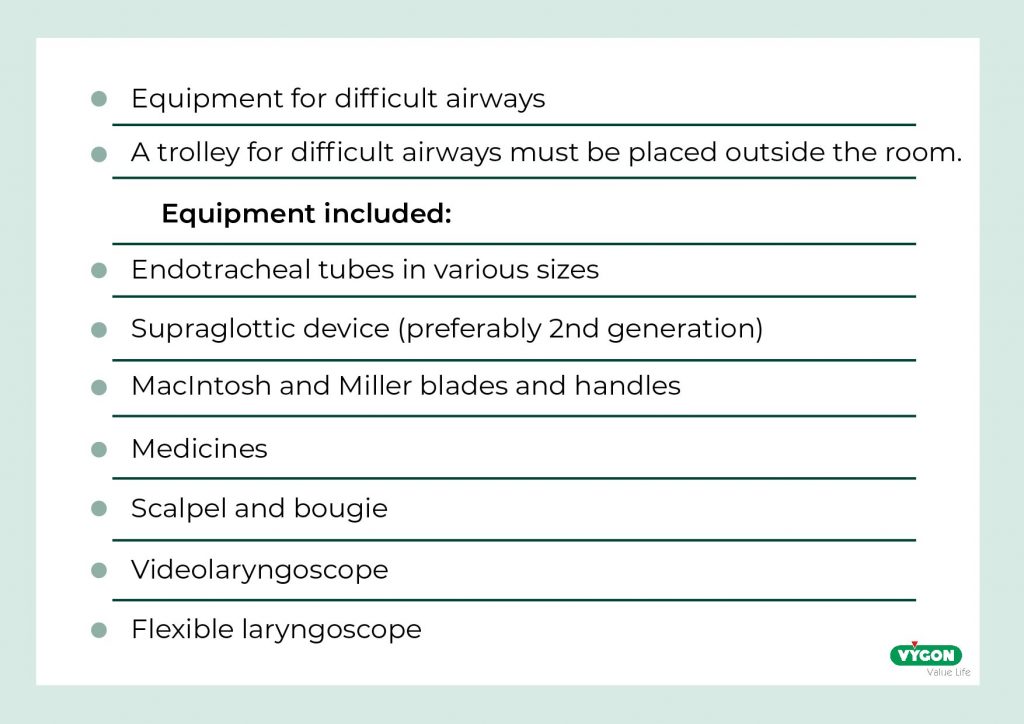
Before entering the patient’s room, the intubation team must discuss and plan the steps to be taken, and check that all the necessary equipment is available:
*SINGLE-USE EQUIPMENT IF AVAILABLE
BARRIER EQUIPMENT
In addition to PPE (personal protective equipment), so-called “barrier” equipment has been developed to protect healthcare workers from contamination by viral particles spread during aerosol-generating procedures.
This equipment was approved by the FDA (Food and Drug Administration) in May 2020 for use in conjunction with PPE, but doubts about its actual safety led to its withdrawal in August 2020.
RECOMMENDATIONS
Physiological risk factors associated with difficult airways need to be weighed up.
This includes COVID-19 patients:
- hypovolemia due to aggressive diuresis,
- chronic desaturation,
- pulmonary hypertension,
- myocardial dysfunction,
- cardiovascular collapse.
The recommendations are as follows:
- If possible, the intubation team should consist of 4 members:
- A professional with experience in advanced airway management,
- A second assistant specialized in airway management,
- A specialist in pneumology,
- An observer (who will remain outside the room).
Use the IMA as described in the COVID-19 guidelines on patient airway management for non-difficult intubations.
2. Use the IMA as described in the COVID-19 guidelines on patient airway management for non-difficult intubations.
3. S’il est disponible, utiliser un appareil à pression positive comme PEV de première intention en cas d’intubation urgente.
4. Prévoir un chariot pour les voies aériennes difficiles (qui sera placé à l’extérieur de la chambre du patient) comprenant des fournitures à usage unique, le cas échéant.
5. Barrier teams are not recommended for the management of difficult airways in patients confirmed or suspected of having COVID-19.
PRE-INTUBATION OXYGENATION
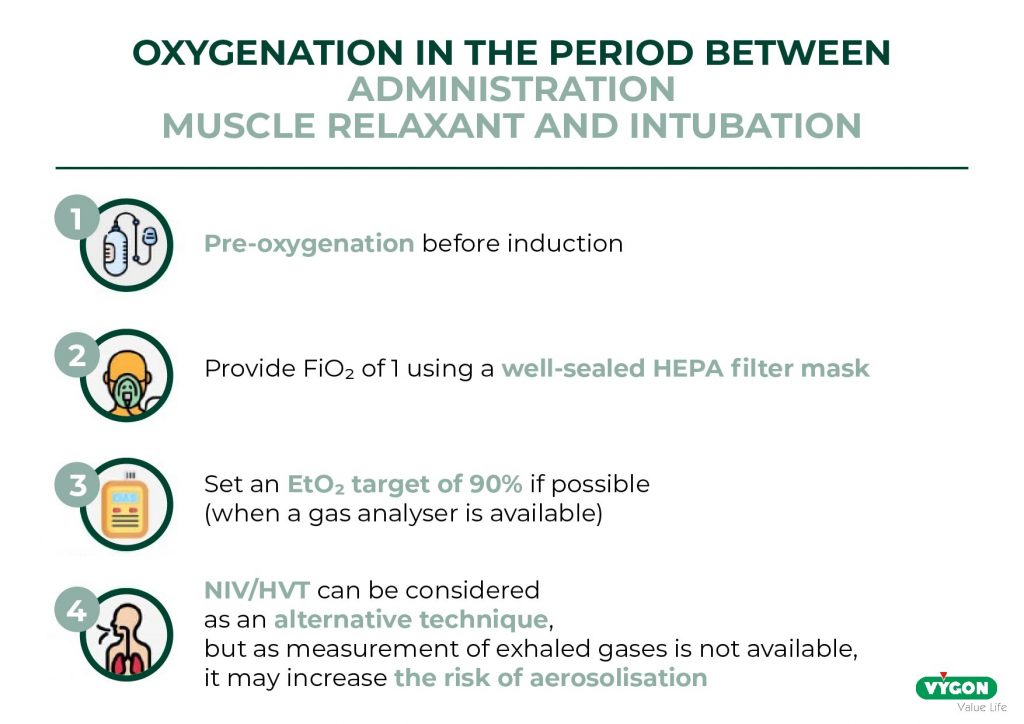
In the COVID-19 patient with respiratory difficulties, preoxygenation is of paramount importance because of the high probability of hypoxemia, and because the duration of respiratory difficulty management may be longer than in a patient without difficulties.
PRE-OXYGENATION BEFORE INDUCTION
A suitable mask with an airtight seal and attached HEPA filter enables optimal pre-oxygenation in spontaneously breathing patients. The aim is to achieve an EtO₂ level of 90% measured by a gas analyzer, or for 3 minutes if a gas analyzer is not available.
OXYGENATION DURING THE PERIOD BETWEEN ADMINISTRATION OF THE MUSCLE RELAXANT AND INTUBATION
In patients with COVID-19, desaturation may be rapid and persistent. In patients with difficult-to-reach airways, given the limited effectiveness of apnea oxygenation in preventing oxygen desaturation after induction/muscle relaxation and the potentially increased risk of aerosolization, when hypoxemia is present or imminent, mask ventilation with a tight-fitting face mask is recommended.
POST-INDUCTION OXYGENATION
- In hypoxemic patients, mask ventilation should be performed using a hermetically sealed face mask.
- If mask ventilation is ineffective, or if significant leaks occur, a supraglottic device, preferably a second-generation device, should be inserted to facilitate ventilation.
- Consider apnea oxygenation.
PHARMACOLOGY FOR AIRWAY MANAGEMENT
This technique is often used to manage difficult airways during routine anesthetic induction, with or without neuromuscular relaxation. Neuromuscular relaxation can lead to inability to intubate or ventilate, or even other complications.
In COVID-19 patients, the extra time required to perform this technique may increase the risk of severe desaturation and cardiopulmonary arrest, and prolong the exposure of healthcare professionals.
POSSIBLE INTUBATION TECHNIQUES
- Flexible endoscope
When using a flexible video endoscope, a remote screen should be used to keep the operator’s face away from the patient’s airway and reduce the risk of infectious exposure when the patient coughs or otherwise aerosolizes.
The use of a single-use video endoscope is preferable, given the difficulty of rinsing reusable devices.
An endoscopy mask can be used to close the patient’s mouth and nose during the procedure.
- Videolaryngoscope
As with the flexible video endoscope, a remote screen must be used to allow the operator to turn his or her face away from the patient’s airway during the procedure.
INTUBATION AFTER INDUCTION
- Videolaryngoscopy
Videolaryngoscopy performed by a qualified practitioner should be the technique of first choice for intubation of the sleeping patient in the event of respiratory difficulties in the COVID-19 patient, if available. If the practitioner is more skilled in direct laryngoscopy for management of difficult airways, or if videolaryngoscopy fails, these devices should also be available.
- Intubation with a supraglottic device
If initial intubation attempts fail, oxygenation with a hermetically sealed mask with HEPA filter can minimize aerosolization, while intubation with a supraglottic device, preferably a 2nd-generation device due to its higher oropharyngeal leak pressure allowing higher respiratory pressure as well as possible drainage of regurgitation, is considered.
EMERGING INVASIVE AIRWAYS
Cricothyrotomy may be required in patients with COVID-19 if non-invasive airway management fails, or in situations of CVCI or CICO. Some guidelines recommend surgical airway access for patients with COVID-19.
The recommendations are :
- Use simple surgical techniques, such as cricothyrotomy with scalpel and bulbous tube, in emergencies requiring invasive access.
- Do not use jet ventilation , as it increases aerosolization of viral particles.
- Interrupt ventilation just before cricothyroid membrane puncture to minimize aerosolization from the cricothyroid puncture site.
- Include scalpel, endotracheal tube ≤6.0 and adult candle in difficult airway cart equipment.
- Technical competence and familiarity with emergency airway access techniques can improve the successful management of rescues in emergent airway situations.
ENDOTRACHEAL TUBE EXCHANGE
In COVID-19 patients, replacement or manipulation of the endotracheal tube may be necessary due to cuff rupture, accidental extubation or acute ET tube obstruction caused by thick secretions and/or detached tissue and inflammatory cells. These obstructions can limit oxygenation and ventilation capacity, and expose the patient to the risk of increased desaturation.
Here are the recommendations:
- Use a tube exchanger through the terminal adapter between the ET tube and the fan circuit.
- Use the video-laryngoscope during ET tube exchange.
EXTUBATION CONSIDERATIONS
- The risk of contamination during extubation is potentially high, even higher than during intubation, as muscle relaxation has been reversed, the patient ventilates spontaneously and may cough or exhale forcefully.
The risk factors are :
Difficult reintubation and anatomical changes that increase the risk of difficult reintubation, such as airway edema and restricted airway access.
COVID-19 patients with any of these characteristics should be considered at high risk of extubation.
Taking into account the risks of extubation in case of difficult airways and COVID-19, the following steps are proposed:

In conclusion, unlike standard difficult airway guidelines, COVID-19 adds an extra dimension to the risk of exposure to the healthcare professional during patient intubation and extubation. Given that the difficult intubation procedure may last longer than the standard procedure, strict adherence to personal protection protocols will reduce the risk of exposure to healthcare professionals during difficult airway management. Optimal pre-oxygenation and minimization of mask ventilation can also reduce the risk of aerosolization.
For optimal intubation conditions, the patient should be anesthetized with complete muscle relaxation prior to intubation.
The use of video laryngoscopy is recommended as a first-line strategy for airway management, subject to availability and experience. If an urgent invasive airway is indicated, the use of a simple surgical technique, such as a scalpel-bulb-tube, is recommended rather than an aerosol-generating procedure such as transtracheal jet ventilation.






