
Nutritional needs are understood as the amount of each of the nutrients required by an individual at each stage of life to maintain a correct nutritional status and, thus, prevent disease and ensure proper growth.
Ensuring that these nutritional needs are met in the early stages of life is essential. The late start in the provision of nutritional care in a newborn who needs it exposes them, unnecessarily, to situations of metabolic emergency that can alter its mechanisms of homeostatic regulation of the internal environment having short and long term consequences in their nutritional status.
The administration of Enteral Nutrition (EN) in neonates with feeding problems aims to maintain and/or improve their nutritional status, prevent related complications and contribute to the reduction of morbidity and mortality in hospitalised sick patients1,2,3.
Methods for the administration of enteral nutrition
In order to choose the type of food administration, it is necessary to take into account the characteristics that are studied when nutritional support is established: access route, feeding schedule, tolerance, type of food, disease and specific problems of the patient…4,5
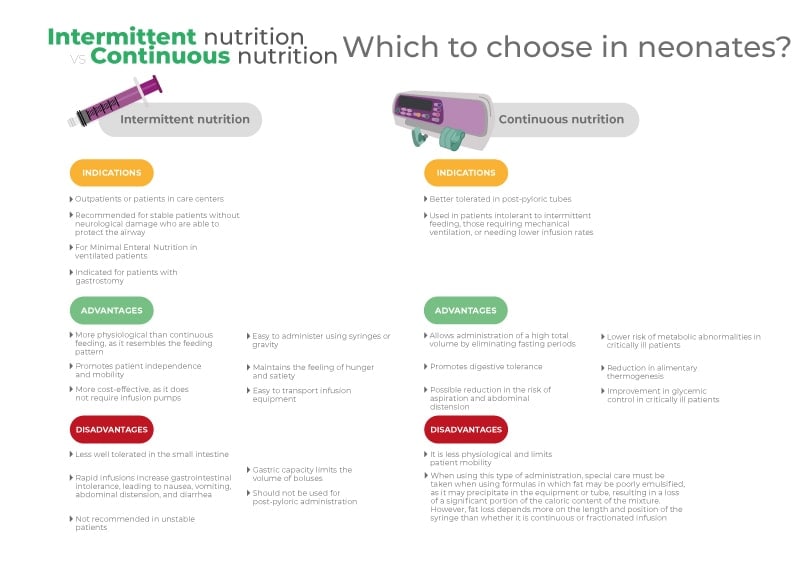
Intermittent enteral nutrition
A form of administration of nutrients periodically through the stomach. It is the most physiological form of nutrition since it is the most similar in rhythm to conventional oral feeding. It allows greater mobility of the patient and the stimulation of oral feeding by provoking periods of hunger and satiety.
It can be administered by syringe, gravity or pump for usually 15 to 45 minutes. Administration time may be longer during the transition from continuous to intermittent EN and in patients with limited tolerance.
It is indicated in gastric feeding and tolerated; in non-critical patients and without risk of aspiration; and in home nutrition whenever possible. Once administration is started, daily increases will be 25-50% of the volume of the previous day’s intake until the requirements are reached.
Children fed through this method are more likely to present bloating or abdominal pain, excess gastric residue, regurgitations or vomiting or dumping syndrome due to the larger intragastric volume4,5,6.
Continuous enteral nutrition
It consists of administering formula at a continuous rate, without interruption throughout the day. This technique involves little gastric residue and allows a more efficient energy balance than intermittent EN. In addition, the administration is of greater volume because it favors digestive tolerance.
It is indicated in patients with malnutrition, in post-pyloric nutrition, in patients with reduced absorption as in the case of short bowel syndrome, in patients at risk of aspiration, when intermittent feeding is not tolerated and in situations of high energy expenditure (lung disease, heart disease…)4,5,6
Cyclic enteral nutrition
This is a method of continuous administration, but in periods of less than 24 hours (8-12 hours), usually at night. It facilitates oral nutrition on demand during the day and nocturnal supplementation4. It is widely used in home enteral nutrition, in combination with oral or bolus feeding during the daytime5.
Enteral formula delivery systems
Gravity/gavage:
It is free-fall method of administration from a syringe (bolus) or by a drip system. The modality is used exclusively when the tube is lodged in the stomach, it is not appropriate if it is lodged in the intestine. It is simple to use, but must be monitored frequently to ensure that the desired amount of nutrition is infused, especially in the drip system4,5,6,7,8.
It is used for both intermittent and continuous feeding. In the case of intermittent nutrition, we find two modes of infusion:
- Boluses: the substance is administered at an interval of less than thirty minutes, using a syringe that will divert the nutritional formula to the implanted tube6 . In neonatal patients in the NICU, especially very immature preterm infants, fractionated administration should be slow enough (20 – 30 min) which limits gravity administration if not done by the parents.
- Conventional drip system in which formula is delivered by connecting a tube to a bag or container regulated by a thread. The infusion is given over a period of 45-60 minutes in different shots spread throughout the day. This method allows greater control in administration, is better tolerated by the patient and easier for the nursing staff. It is recommended that the feedings have a low viscosity4.
In the case of continuous gravity feeding, the rate is controlled by a mechanism that decreases the caliber of the line by increasing resistance to flow. This is not recommended in paediatric EN4,6.
Syringe pump:
The use of syringe pumps for the administration of enteral nutrition helps to improve the accuracy of the formula to be infused. They allow constant volumes to be administered, which reduces the possibility of increased gastric residue, minimizes the risk of aspiration and improves the diet, and also reduces the burden on the health professional or the family (in the case of home care)4,5,6,7,8.
They are used for both continuous and intermittent administration, as is the gravity system.
- Intermittent EN: to administer the solution by this method it is necessary to ensure that the newborn is stable and has adequate gastric emptying, as well as a low risk of aspiration. The technique is similar to conventional drip gravity, but improves control of the infusion rate and reduces the risk of overdose in the neonatal patient4.
- Continuous EN: this type of administration, of small volumes, is recommended in those patients with the tube located in the gut or in the critically ill stomach. This nutrition system improves nutrition tolerance and reduces complications related to high feeding volumes. In addition, syringe pumps feature alarm systems that make their use more convenient 4,6,7.
In many departments, most fractionated enteral nutrition is administered by pump due to lack of personnel.
There is no one method or system of nutrition administration that is better than another. When choosing among the different options, the pros and cons of each one should be analysed and it should be determined which one is the most convenient to cover the patient’s needs according to his condition and specific requirements.
Bibliography
- Soria RM. Enteral feeding in neonates. Neonatal Nursing Journal 2010;8:11-14.
- Guillen AM, Serra JD. Feeding of the healthy newborn. Neonatology Service and Nutrition and Metabolopathies Section of “La Fe” Hospital, Valencia 2008.
- Pediatric and Neonatal Nutrition by Isabel Caba Porras, Amparo Vázquez Polo. Nutricia.
- Lama More, R., n.d. Enteral Nutrition. Madrid: AEPED, pp.388-389. Available at: https://www.aeped.es/sites/default/files/documentos/nutricion_enteral.pdf.
- Palomino Pérez, L., et al. Special Methods for the Nutrition of Hospitalized Children. Madrid: Sepho, p.6. Available at: http://sepho.es/wp-content/uploads/sites/7/2016/07/M%C3%A9todos-especiales-para-la-nutrici%C3%B3n-de-ni%C3%B1os-hospitalizados.pdf.
- es. 2016. Enteral Feeding by Tube in Preterm Neonates. Available at: https://www.murciasalud.es/preevid/21059.
- Durán Parada, K., 2012. Administration Methods, Infusion Systems and Necessary Implements for Home Enteral Nutrition. Gastrohnup Journal, 14(3), pp.129-130. Available at: https://revgastrohnup.univalle.edu.co/a12v14n3/a12v13n3art7.pdf.
- Ferreyra, C., 2017. Specialization in Critical Care Nursing. Córdoba, Argentina: Faculty of Medical Sciences, pp.16-20. Available at: http://lildbi.fcm.unc.edu.ar/lildbi/tesis/ferreyra-cynthia-soledad.pdf.




