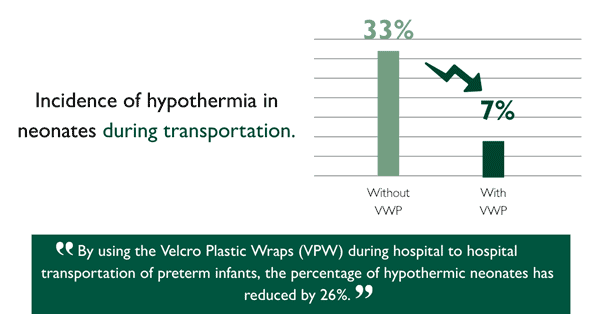
From delivery to the NICU, hospital to hospital and even unplanned home deliveries, neonatal transport is crucial for making sure babies receive the care they need at the right time, and at a unit suited to their needs. Maintaining normothermia during transport has its challenges though, and a 2023 study found up to one third of infants arriving at the destination hospitals are hypothermic1.
Neonates are particularly vulnerable to hypothermia due to their limited ability to regulate body temperature effectively and prolonged exposure to low temperatures can have grave implications for both mortality and morbidity. Newborn admission temperature is a strong predictor of outcomes across all gestations2 as hypothermia can lead to a cascade of adverse effects, including respiratory distress, metabolic acidosis, and compromised immune function.
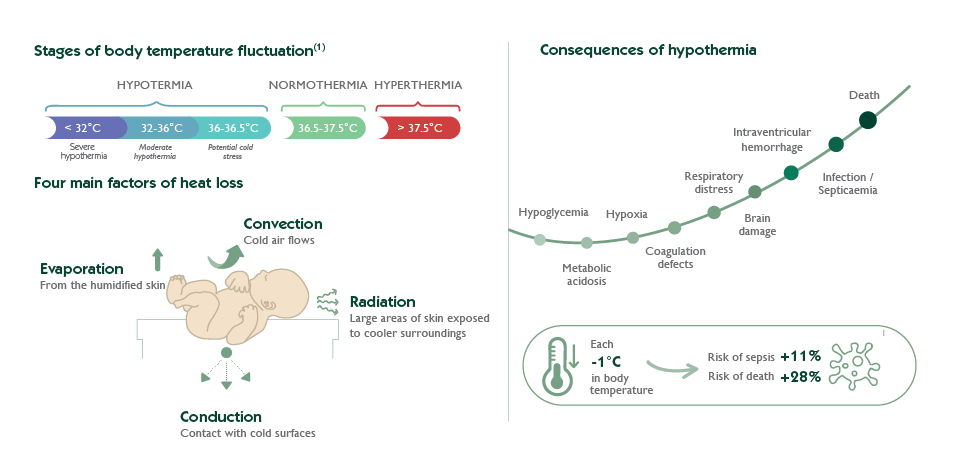
Therefore, ensuring optimal thermal management after birth is crucial in safeguarding the well-being and long-term outcomes of neonates.
International recommendations
Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants
Use of an occlusive polyethylene transparent wrap or bag immediately at birth improved admission temperatures in non-randomised studies of infants at < 27 weeks’ gestation […], between 28 and 30, weeks […] and at < 33 weeks’ gestation […], as well as in very low birth weight infants and extremely low birth weight infants when compared with routine care
Cochraine Database of systematic reviews – 2018
Improvement in thermoregulation outcomes following the implementation of a thermoregulation bundle for preterm infants
The key practice changes included: improved anticipation and staff preparedness, wrapping infant in a polyethylene sheet, using a polyethylene lined bonnet, using servo-control mode at birth and during transport.
Journal of Pediatrics and Child Health – 2022
Neonatal Transfer services across the UK are introducing bespoke polyethylene occlusive suits into their practice and noticing drastic improvements to the temperature of preterm babies arriving at destination hospitals. Before the implementation, the transfer services found they were arriving to babies who were already hypothermic, and the transport environment was making it more challenging to warm them up.
“There are specific challenges to thermoregulation in the transport setting such as changing environment and limited ability to monitor and intervene.”
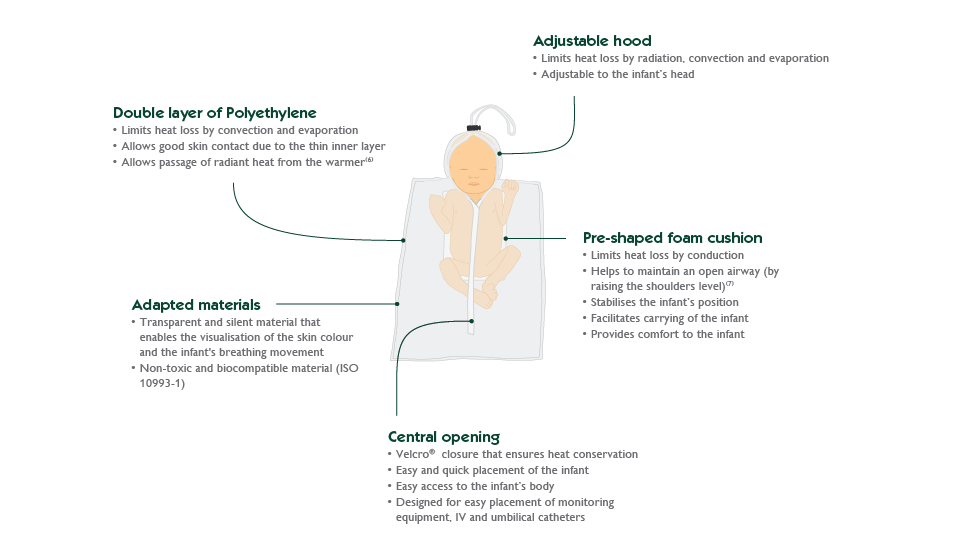
These suits create a microenvironment, minimising heat loss and providing easy access for medical interventions.
Advantages of Polyethylene Occlusive Suits for Neonates
- Easy-to-Access Velcro Central Opening:
- Designed for easy placement of monitoring equipment, IV, and umbilical catheters.
- Tight Closure and Built-In Adjustable Cap:
- Limits heat loss by radiation, convection, and evaporation.
- Adapted Material:
- Transparent and silent material that enables visualisation of the skin colour and the infant’s breathing.
- Sterile, non-toxic material.
- Pre-Shaped Foam Cushion:
- Limits heat loss by conduction.
- Helps maintain an open airway by raising the shoulders level.
- Stabilises the infant’s position.
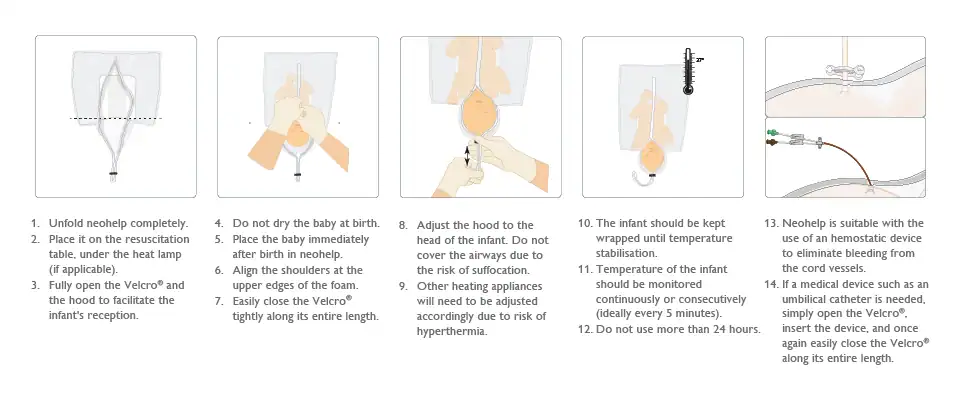
In conclusion, effective thermal management during transport requires a multi-faceted approach and the introduction of polyethylene occlusive suits for neonates during transport has proven to support neonatal care, however it is part of a wider strategy.
The Importance of Preparation and Planning:
- Anticipate the need for thermal support based on the infant’s gestational age and condition.
- Ensure that transport equipment is pre-warmed and readily available.
- Develop standardised protocols for thermal management during transport.
Optimal thermal control during neonatal transport requires a coordinated effort from all members of the healthcare team. This includes:
- Effective communication between referring and receiving facilities.
- Thorough training of transport personnel in thermal management techniques.
- Continuous quality improvement initiatives to monitor and enhance the effectiveness of thermal management protocols.
These suits address the critical need for maintaining normothermia, thereby reducing the risks associated with hypothermia. By ensuring that newborns arrive at their destination hospitals in a stable condition, these suits not only improve immediate health outcomes but also contribute to better long-term health and quality of life for these vulnerable infants. The continued adoption and refinement of such innovative solutions are essential in advancing neonatal care and ensuring the best possible outcomes for our youngest patients.
Bibliography
[1] Improving thermoregulation for preterm babies weighing <1kg during hospital to hospital transportation, a novel use of delivery room equipment, D Bird et al.
[2] Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants, McCall EM, Alderdice F, Halliday HL, Vohra S, Johnston L Cochrane Database of Systematic Reviews 2018, Issue 2.
[3] ANZCOR Guideline 13.4, Management and mask ventilation of the newborn infant, 2016.



