Introduction
This educational framework, developed by Maciej Latos and Linda Kelly and published in the European Journal of Infusion Nursing, is highly relevant in today’s healthcare landscape, where nurses and health professionals are increasingly taking on advanced clinical roles. As Midlines and Long Peripheral Catheters (LPCs) become more common due to their extended dwell times and cost-effectiveness, ensuring safe and competent insertion is critical.
The framework addresses a key gap in current practice: the lack of standardised, longitudinal training models for vascular access. Combining theory, simulation, and supervised practice, with innovation supports safer patient outcomes, reduces complications, and empowers clinicians to deliver high-quality care.
Framework Structure:
The training model is divided into four key phases:
1. Theoretical Training
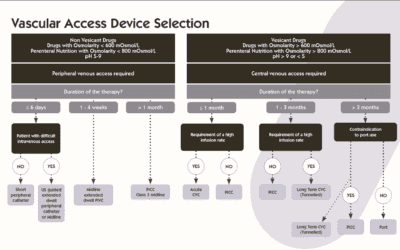
Covers essential knowledge including vein anatomy, device selection, patient assessment, infection control, and complication management. Delivered through lectures, online modules, and pre-distributed materials, this phase ensures foundational understanding before hands-on practice.
2. Practical Skills Development
Focuses on ultrasound-guided vein selection using the RaPeVA protocol and mastery of Seldinger techniques (Direct, Modified, Accelerated). Training includes simulation with gel phantoms and structured practice environments to build confidence and competence.
3. Supervised Clinical Practice
Trainees perform procedures under supervision, with competency typically achieved after 10–30 insertions. Proficiency is documented using standardised forms, ensuring readiness for independent practice.
4. Simulation and Innovation
Simulation-based learning is central to the framework, promoting safe skill acquisition through repetition and feedback. Integrating virtual reality and AI tools enhances accessibility, engagement, and scalability of training.
Why This Framework is Relevant
The educational framework for Midline and LPC insertion is highly relevant in the context of modern healthcare for several compelling reasons:
1. Rising Use of Midline and Long Peripheral Catheters
Over the past decade, Midlines and LPCs have steadily increased due to their extended dwell times, cost-effectiveness, and reduced complication rates compared to short peripheral catheters (SPCs). These devices are particularly valuable for patients requiring intravenous therapy for more than five days or those with difficult intravenous access (DIVA), which affects up to 59% of hospitalised patients, especially women with a history of challenging access.
2. Lack of Standardised Training
Despite their growing use, there is a notable gap in standardised, evidence-based training for clinicians performing Midline and LPC insertions. The review highlights that only one study to date has described a comprehensive training process for Midline insertion. This lack of structured education contributes to variability in practice and increases the risk of complications.
3. Impact on Clinical Outcomes
The framework addresses a critical need for competency-based training. Studies cited in the review show that:
- 25% of patients may experience early complications during Midline insertion.
- Late complications such as catheter occlusion, thrombosis, and infection occur in 8–38% of cases.
- Simulation-based training has demonstrated a 97% success rate in cannula insertion after just a 60-minute session.
These findings underscore the importance of structured training in reducing adverse events and improving procedural success.
4. Economic and Operational Efficiency
Midline catheters offer a cost-effective alternative to central venous access devices (CVADs) like PICCs and tunnelled catheters. Their use can reduce the need for more invasive procedures, lower the incidence of central line-associated bloodstream infections (CLABSIs), and shorten hospital stays. However, these benefits are only realised when insertion and maintenance are performed competently—hence the need for a robust educational framework.
5. Alignment with Evolving Nursing Roles
As nurses increasingly take on advanced clinical responsibilities, including vascular access, this framework supports their professional development. It moves beyond outdated models like “see one, do one, teach one” and embraces simulation, supervised practice, and competency validation, aligning with modern educational standards and regulatory expectations.
Potential Impact on Patient Outcomes
Implementing this educational framework can significantly improve patient outcomes by:
- Reducing complications such as infection, thrombosis, and catheter dislodgement through better technique and device selection.
- Improving first-attempt success rates, minimising patient discomfort and procedural delays.
- Enhancing patient satisfaction by reducing painful, repeated cannulation attempts, especially in patients with difficult intravenous access (DIVA).
- Supporting continuity of care, as well-trained staff can maintain catheter patency and manage complications more effectively.
- Lowering healthcare costs by reducing the need for central lines and associated complications.
Ultimately, this framework elevates clinical practice and contributes to a safer, more patient-centred healthcare system.
Conclusion
The Educational Framework for Midline and Long Peripheral Catheter Insertion: A Narrative Review represents a timely and essential advancement in clinical training. As the use of these vascular access devices continues to rise, there is a pressing need for structured, evidence-based education to ensure their safe and effective use.
This framework addresses a critical gap in current practice. Moreover, the emphasis on structured documentation and competency validation aligns with modern healthcare standards, making this framework a valuable blueprint for institutions aiming to implement or improve Midline Catheter programs.