Laying the Groundwork for Safe Arterial Line Insertion
Before a needle touches the skin, a thorough patient assessment and clear communication are essential. These early steps are not just procedural—they are foundational to patient safety, ethical practice, and clinical success. In this section, we explore how to assess patients for arterial line insertion and how to approach consent, even in high-pressure environments.
Why Assessment Matters
Arterial cannulation is an invasive procedure. While generally safe, it carries risks that can be mitigated through careful pre-procedural evaluation. A well-conducted assessment helps clinicians:
- Identify contraindications
- Choose the most appropriate site
- Anticipate complications
- Build trust with the patient or their family
Key Factors to Assess Before Insertion
The following factors should be considered before inserting an arterial line.
🩸 Medical History
- Diabetes – May affect vascular integrity and healing
- Peripheral vascular disease – Increases risk of thrombosis or occlusion
- Raynaud’s syndrome – Contraindicated due to poor peripheral circulation
- Previous surgeries or trauma – May alter anatomy or compromise access
💉 Local Considerations
- Infection or burns at the proposed site
- Previous arterial line placements (especially within the last 2 weeks)
- Presence of AV fistulas or grafts
🧠 Cognitive and Physical Status
- Is the patient conscious and able to give consent?
- Can they cooperate with positioning and remain still during the procedure?
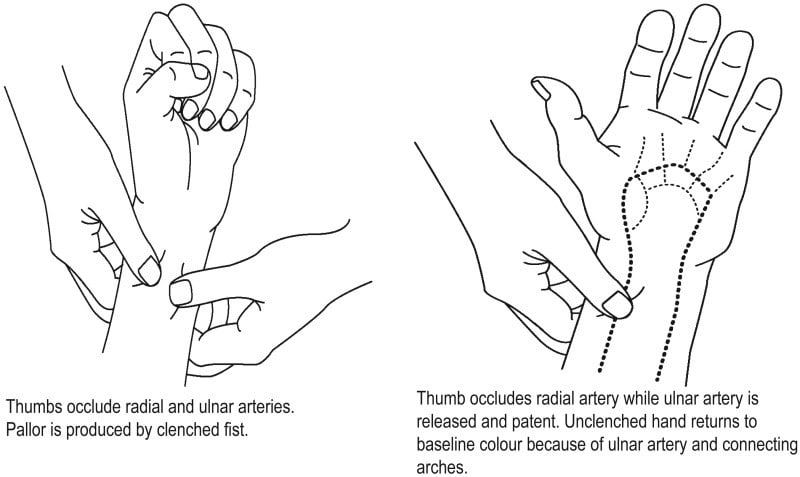
The Allen’s Test: A Simple but Vital Check
Before radial artery cannulation, it’s essential to confirm that the hand has adequate collateral circulation via the ulnar artery. The modified Allen’s test is a quick bedside assessment:
- Ask the patient to clench their fist (or close it for them).
- Occlude both the radial and ulnar arteries using firm pressure.
- Ask the patient to open their hand—it should appear pale.
- Release pressure on the ulnar artery only.
- Positive test: Hand flushes within 15 seconds → proceed with radial cannulation.
- Negative test: No flush → avoid radial artery on that side.
If the test is negative, assess the other arm or consider an alternative site.
Communicating with the Patient
Even in urgent settings, patients (or their families) deserve to understand what’s happening. A clear explanation should include:
- Why the arterial line is necessary
- What the procedure involves
- Risks: bleeding, infection, occlusion, discomfort
- Expected duration of the line
- What to expect during and after the procedure
In emergencies or with unconscious patients, verbal consent may not be possible. In such cases, document the clinical justification and proceed in the patient’s best interest.
Documentation Essentials
Record the following in the patient’s notes:
- Assessment findings (e.g., Allen’s test result)
- Site selection rationale
- Consent discussion (or reason for implied consent)
- Any anticipated challenges or precautions
Conclusion
Patient assessment and consent are not just checkboxes—they are acts of clinical diligence and respect. By taking the time to evaluate risks, communicate clearly, and document thoroughly, clinicians lay the foundation for a safe and successful arterial line insertion.



