Staying Ahead of the Risks in Arterial Cannulation
While arterial line insertion is a routine procedure in critical care, it is not without risk. Even with proper technique and training, complications can occur—some minor, others potentially life-threatening. The key to safe practice lies in anticipating these risks, recognising early warning signs, and responding swiftly and appropriately. In this series, we explore the most common complications associated with arterial lines and how to prevent and manage them effectively.
Common Complications and How to Handle Them
1. Infection
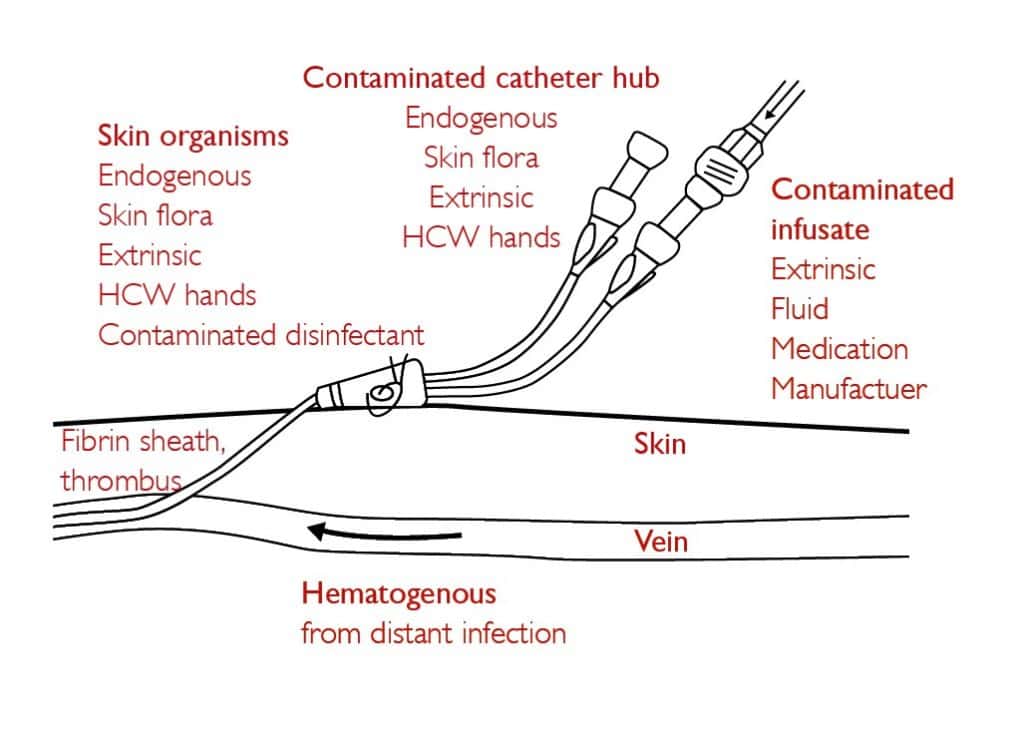
Cause: Infection is a significant complication associated with arterial lines, often underestimated. Despite being frequently handled in critical care, arterial catheters can be a source of bloodstream infections, with colonisation occurring via:
- Extraluminal routes (skin flora at the insertion site)
- Intraluminal contamination (hub manipulation)
- Haematogenous spread (from distant infections)
Risk factors include poor aseptic technique, inadequate skin disinfection, insecure catheter placement, and frequent line manipulation.
Microbial sources:
- Resident flora (e.g., S. aureus, S. epidermidis)—difficult to remove and can invade sterile sites.
- Transient flora—transferred via contact or contaminated surfaces.
Prevention:
- Strict hand hygiene before handling lines.
- Use of Aseptic Non-Touch Technique (ANTT)—surgical ANTT for Seldinger technique; standard ANTT for short-term cannulas.
- Cutaneous antisepsis with >0.05% chlorhexidine in 70% alcohol.
- Minimise line manipulation and ensure secure fixation.
Management:
- Suspected infection:
- Remove the arterial line if clinically indicated.
- Send catheter tip and blood cultures for microbiological analysis.
- Confirmed infection:
- Initiate appropriate antimicrobial therapy.
- Monitor for signs of systemic involvement (e.g., sepsis).
- Prevent recurrence:
- Review insertion and maintenance protocols.
- Educate staff on infection control practices.
By adhering to these practices, clinicians can significantly reduce the risk of arterial line-associated infections and improve patient safety.
2. Air Embolism
Cause: Entry of air into the arterial system through loose connections or unprimed tubing.
Signs:
- Over-dampened arterial waveform
- Tachycardia, hypotension
- Tachypnoea
- Loss of consciousness
Prevention:
- Prime all tubing before connection
- Avoid prolonged flushing
- Ensure all connections are tight
Management:
- Call for urgent medical assistance
- Tighten all connections
- Monitor patient closely
3. Arterial Occlusion or Thrombosis
Cause: Trauma to the vessel wall or catheter occupying too much of the lumen.
Signs:
- Cold, pale limb distal to insertion
- Loss of arterial waveform
- Pain, numbness, or paralysis
- Absent pulse
Prevention:
- Use a 20G catheter for radial access
- Minimise trauma during insertion
- Ensure adequate flushing
Management:
- Remove the catheter immediately
- Seek urgent vascular or medical review
4. Haemorrhage
Cause: Dislodgement of the catheter or loose connections in the system.
Signs:
- Visible bleeding
- Hypotension, tachycardia
- Cardiac arrest (in severe cases)
Prevention:
- Secure the catheter properly
- Keep the site visible
- Maintain pressure bag at 300 mmHg
Management:
- Apply direct pressure
- Re-secure or replace connections
- Monitor vital signs and escalate care
5. Accidental Drug Injection
Cause: Mistaking the arterial line for a venous access point.
Signs:
- Immediate pain or discomfort
- Mottled skin
- Absent pulse or limb dysfunction
Prevention:
- Never administer drugs via an arterial line
- Use red tubing and clear labelling
- Educate all staff on arterial line identification
Management:
- Call for urgent help
- Attempt to aspirate the drug
- Monitor for ischemic complications
6. Haematoma
Cause: Inadequate pressure post-insertion or removal.
Signs:
- Swelling and bruising at the site
- Pain or discomfort
Prevention:
- Apply firm pressure for at least 5 minutes after removal
- Avoid multiple puncture attempts
Management:
- Apply pressure
- Monitor for progression
- Document and report
Conclusion
Complications from arterial lines are rare but can be serious. The best defence is a proactive approach: know the risks, follow best practices, and act quickly when problems arise. With vigilance and preparation, clinicians can ensure arterial cannulation remains a safe and effective tool in critical care.



