The thoracic reservoir has been widely used for vascular access in chronic patients for many years, particularly in oncology. It is a reliable device, and when not in use, it requires relatively low maintenance care. However, as indicated by the recent study by Moralar et al. carried out in 1198 patients, complications exist. One of the most frequent is occlusion, which can reach up to 36%¹.
Christian Dupont, an international reference nurse in the field of vascular access, president of GIFAV and member of the WoCoVA committee, helped us understand why fully implanted devices such as the chest reservoir and the PICC-port can suffer complications and how to prevent them.
Main errors observed in the handling of Totally Implantable Venous Access Devices (TIVAD)
Inadequate practices may persist in services handling these devices, such as oncology day units and oncology wards, in addition to others.
1 Poor palpation
Throughout his long career as a clinical nurse and trainer, Christian has often observed that many individuals express troubles, such as, “I can’t puncture the reservoir.”
“That can happen because the TIVAD has been turned around, but in general, one of the things that can be improved in this aspect is palpation.”
To ensure proper palpation, the following guidelines are recommended for the reservoir:
- Palpate the entire catheter path, including both the reservoir and the subcutaneous tunnel.
- Go all the way around the reservoir during palpation.
- Apply light pressure on the connection between the catheter and the chamber. This allows the catheter to lift slightly, providing a two-dimensional perspective.
By following these three steps, the health professional has all the references prior to the puncture.
“If we see that the implantable chamber sinks when pressing, that the tissue is soft, the patient is asked to change position to achieve a more stable base.”
2 Inadequacy of needle length
Christian reminds us that the selection of products in relation to the patient’s characteristics is also paramount. In this case, it is essential to adapt the length of the needle to the reservoir because a needle that is too long will cause the dressing to be unstable and will not be able to remain on the skin.

Photo: courtesy of Paloma Ruiz.)
To do this, palpation plays a very important role because it will also determine the thickness of the patient’s adipose tissue and the size of the chamber.
3 Ineffectiveness of fixation
Needle fixation occupies a vital place. Christian tells us the following:
“To achieve optimal fixation, it has to involve two parts: adhesive strips to fix the Huber needle and a transparent dressing with a non-adhesive centre to cover it.”
As Christian reminds us, it is key to always make the insertion point visible to detect possible complications early.
4 Lack of interest in blood backflow
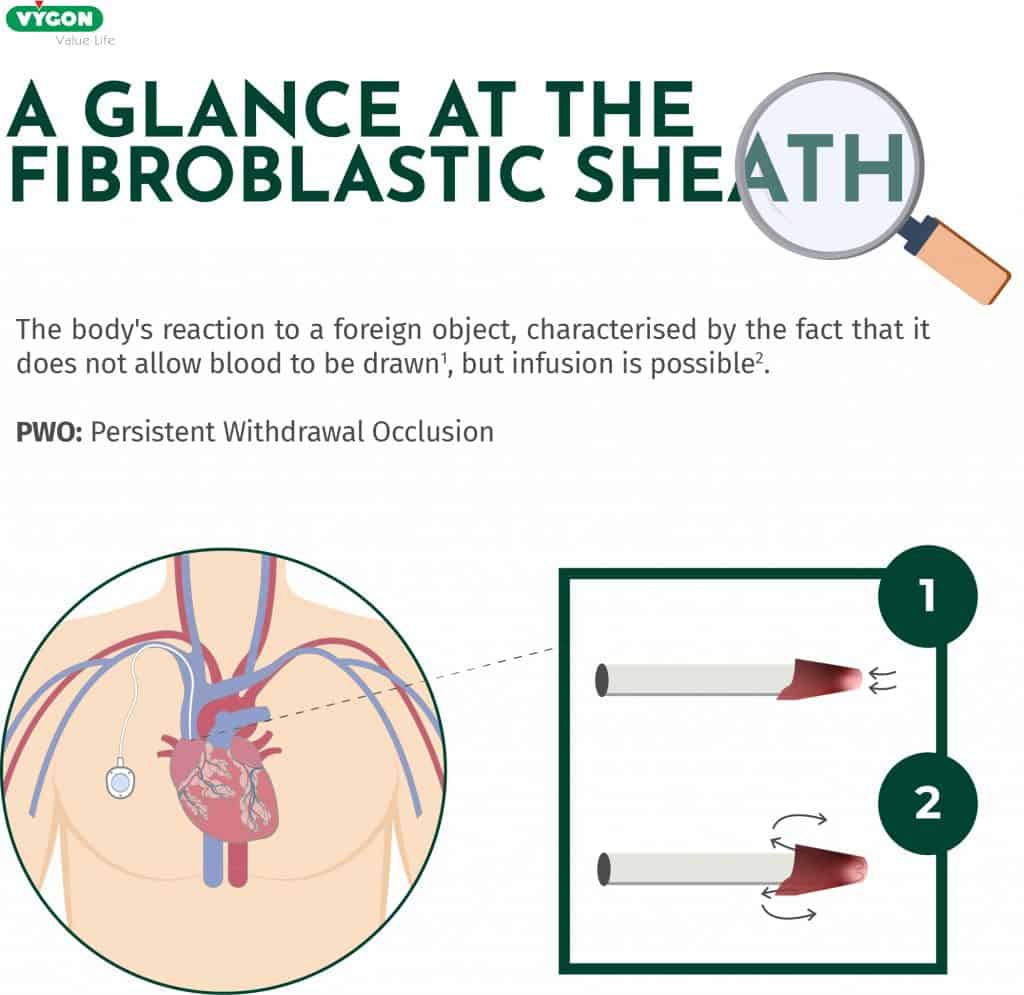
“If the catheter does not allow venous return, we have to know why.”
As mentioned earlier, a common complication of this device is the difficulty in obtaining blood return or infusion. Christian emphasises that the nurse responsible for managing the reservoir or PICC-port should not view the obstruction of the device as a normal occurrence, regardless of how frequently this complication arises.
Possible causes of occlusion of a reservoir/PICC-port.
When complications arise, it is typically due to partial or complete obstruction of the device. Christian outlines the possible causes of obstruction:
1. Blockage of the catheter lumen by deposits, which can often be resolved by flushing the line.
2. Formation of a fibroblastic sheath around the catheter.
3. Use of an improperly sized needle.
4. Venous thrombosis
5. Change in the position of the catheter tip, which may no longer be at the cavo-atrial junction.
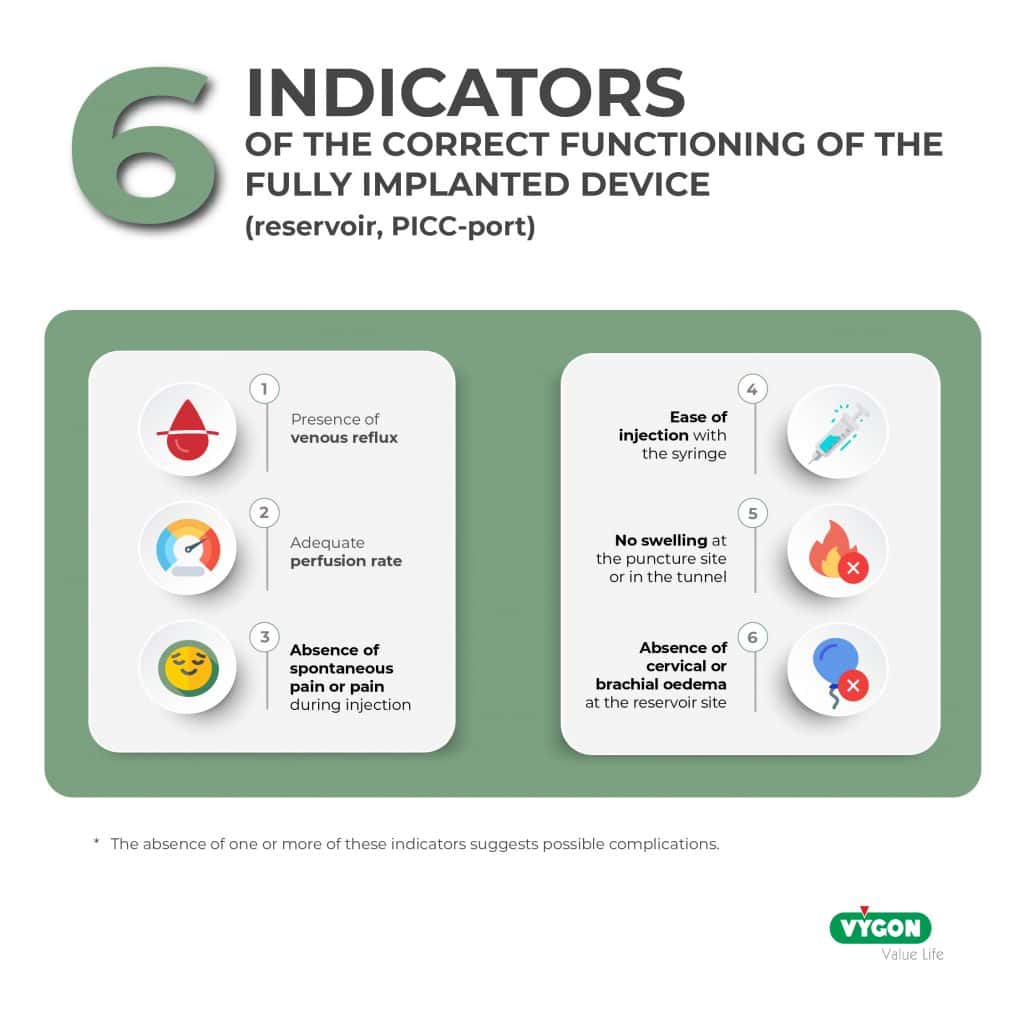
In the event of an occlusion, Christian advises that if a healthcare professional encounters difficulty with injection and the administration of medication is not urgent, it should be postponed. He also notes that, if reflux is absent and under specific conditions, administration may be safe if:
- There’s no resistance.
- There is no swollen area.
- There is no pain.
These precautions are especially relevant for non-vesicant drugs.
Importance of Withdrawal with Respect to Catheter Tip Blood Return
In Christian’s experience, one factor that can lead to blood remaining in the catheter lumen is the improper removal of the Huber needle.
Compared to other devices, flushing a PICC catheter is easier when a syringe or infusion set is disconnected, as it has a linear design. In contrast, an implantable chamber features a septum, and when the needle is removed from this membrane, it creates a phenomenon known as aspiration. Due to this configuration, purging the reservoir or PICC port while removing the Huber needle becomes more complicated.
To counteract the suction effect during removal, it is necessary to purge at that moment. While performing positive pressure is an option, most devices require three hands: two to remove the needle and one to purge. However, there are positive pressure Huber needles designed to accomplish this task using just two hands.
Frequency of washing and sealing of the fully implanted device.
The most recent vascular access guidelines, such as those from the INS2, are based on the latest research and recommend the following for catheter flushing:
- Flush the catheter before and after each infusion of solutions or drugs.
- If the reservoir or PICC-port is not in use, it can be washed and sealed every 4-12 weeks. The Lang study3 indicates that there is no increased risk of complications when establishing the frequency of care at 12 weeks.
International recommendations from organisations like GAVeCeLT4 and WoCoVA emphasise that the use of heparin is obsolete:
“There is no evidence to use a heparin sealant. Prevention of catheter obstruction is based on effective saline washing and sealing.”
For effective flushing, similar to other vascular accesses, it is essential to use the push-pause technique: inject 10ml of saline solution using small boluses of 1.2ml to create a turbulent effect inside the catheter lumen, ensuring that all residues are cleared. In cases involving transfusions, parenteral nutrition, contrast, or blood collection, the wash should be carried out with 20ml of saline.
Expert tips for proper care of reservoirs and PICC-ports
1. Updating your knowledge and practices
As a professional, it is essential to regularly evaluate your work methods and update your protocols and daily practices. Understanding and applying the recommendations from authoritative organisations is important. Additionally, having the appropriate materials is crucial for implementing best practices in vascular access care.
2. Catheter tracking
It is important to ensure traceability of the vascular access that the patient has. However, it is not necessary to perform an exhaustive follow-up by tracking numerous parameters, as this can cause the professional to lose focus and create a sense of being overwhelmed.
To effectively monitor a catheter, you should keep track of the following information:
1. The date the vascular access was placed.
2. The date it was removed.
3. The reason for removal, such as the end of treatment or a complication.
4. Be clear about the 6 Indicators of the correct functioning of the fully implanted device:
5. Record any issues regarding the removal of the needle and note if it has been sealed with a solution other than saline (such as citrate or a similar solution).
Accessing a reservoir in a PICC-port requires the consideration of several straightforward and effective measures. Failing to adhere to the management and care protocols for a fully implanted device can put the patient at risk. These risks may lead to situations where the reservoir cannot be utilised, forcing the patient to undergo a new catheter placement, which entails additional resources and expenses.
In the world of vascular access, thanks to expert professionals such as Christian Dupont, there is access to clear and secure information through guides and protocols. Nowadays, implementing them is within the reach of any professional who wants to apply best practices.
References:
- Moralar DG, Turkmen UA, Bilen A, Turkmen S, Feyizi H, Altan HA. Our central venous port catheter system practice – a retrospective study. J Pak Med Assoc. 2021 May;71(5):1442-1445. doi: 10.47391/JPMA.03-240. PMID: 34091631.
- Infusion Therapy Standard of Practice Guides – 2021
- Lang et al., Is There a Relationship Between Frequency of Port-Care Maintenance and Related Complications in Patients With Cancer? , JCO Oncology Practice, Volume 18, Issue 9 – July 2022
- Pittiruti et al., Evidence-based criteria for the choice and the clinical use of the most appropriate lock solutions for central venous catheters (excluding dialysis catheters): a GAVeCeLT consensus , J Vasc Access, Nov 2;17(6):453-464. – 2016