PICC-port is gaining prominence as a primary vascular access device for oncology patients, surpassing traditional chest ports and outdated brachial ports. Dr. Bertoglio’s recently published multicentre study, which examined over 4000 PICC-ports, demonstrates the safety of this alternative.
Nevertheless, like any medical device, PICC-ports carry a risk of complications. Ensuring proper placement is crucial in minimizing potential issues.
To ensure a safe and cost-effective procedure, it is important to consider the following key steps when inserting a PICC-port.
Use of ultrasound
Given the current evidence, the use of ultrasound for venous puncture is essential.
-
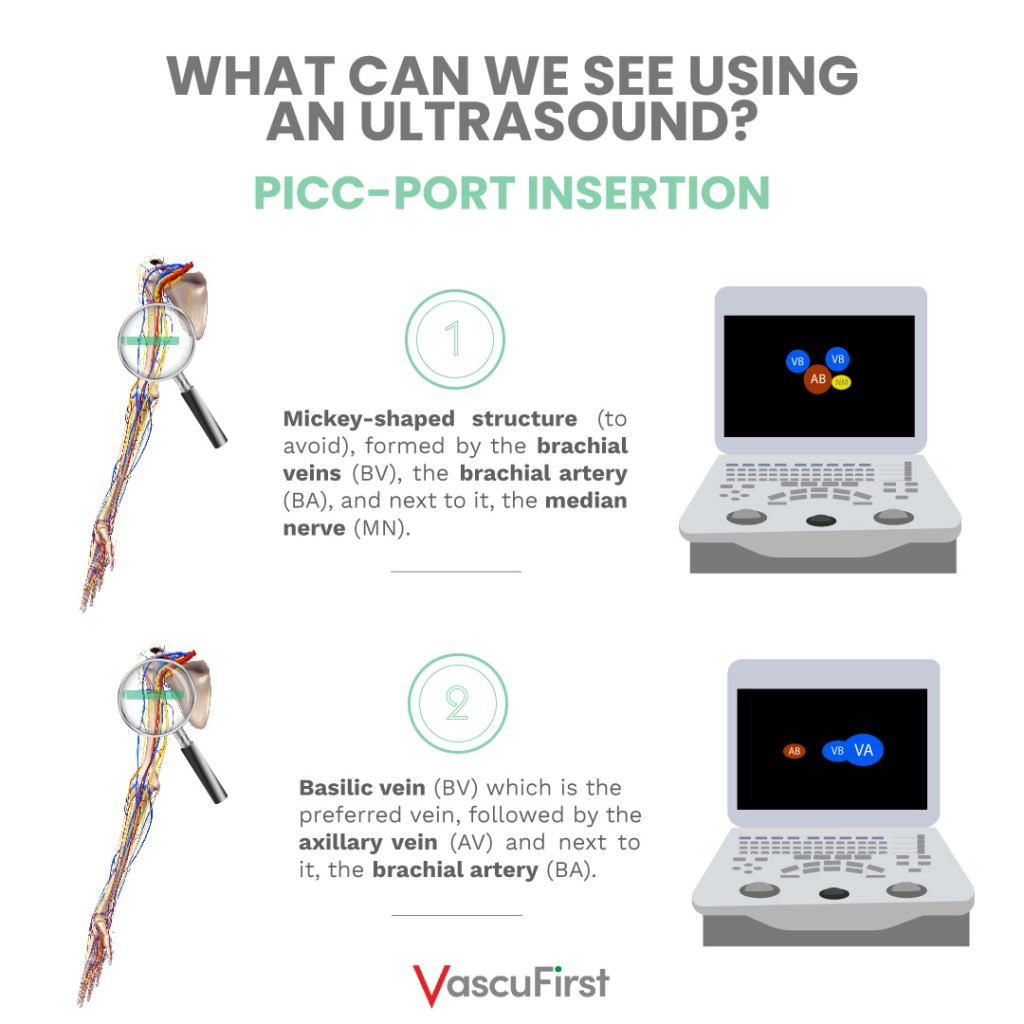
What can we see using an ultrasound?
Ultrasound provides a significant advantage by allowing us to visualize the hidden parts. When using it, we can observe deep structures such as:
> Veins in the arm from the middle third to the armpit.
> The bundle formed by the brachial veins, the brachial artery, and the median nerve.
> The basilic vein and the axillary vein, which are formed by the union of the basilic vein and the brachial veins in the upper third of the arm.
> Also, thrombus, vein circumference and valves.
In recent years, a substantial body of literature has highlighted the advantages of ultrasound not only for ultrasound-guided punctures but also for the pre-assessment of patients using evaluation protocols or mapping techniques like RaPeva and RaCeVA protocols, developed by GAVeCeLT.
-
What are the benefits of ultrasound?
Thanks to the mentioned protocols, we can accurately assess the patient’s vascular anatomy, considering:
> The depth of the vessels.
> The relationship between these vessels and with other adjacent structures like nerves or the pleura.
> The size (calibre) of the vessels and their collapsibility under pressure.
> Thrombosis.
Furthermore, ultrasound allows us to precisely determine the proper placement of the guide in the vessel, the catheter in the vein, and even confirm the absence of the catheter in veins like the internal jugular.
Ultrasound-guided puncture significantly improves the first-attempt success rate and reduces complications such as thrombosis or infection and failed attempts.
USE OF INTRACAVITARY ECG
-
What do international recommendations say?
International guidelines now recommend replacing radiological tests like chest X-rays or fluoroscopy to confirm the tip position of central catheters with alternative methods of confirmation.
One of the methods that is gaining popularity is the recent use of ultrasound with a convex probe for trans-thoracic echocardiography in adults, children, and neonates. Although it requires technical and manual skills, as well as access to the appropriate probe, it is considered as a fast and safe intraoperative method.
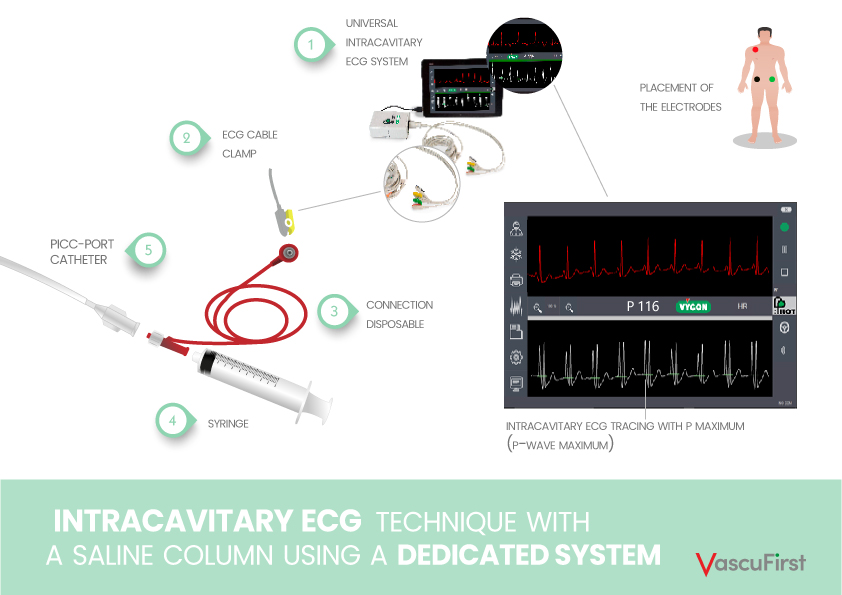
The intracavitary ECG (Image 2 and 3) emerges as an attractive alternative. It offers a rapid and safe option that eliminates the need for X-rays and is harmless for the patient. Moreover, it provides precise results and is cost-effective with a shorter learning curve compared to echocardiography.
-
What are the advantages of the ECG-IC method?
This technique, described over 70 years ago and refined over the decades, is the most effective method for achieving a central position of the catheter.
For the PICC-port specifically, its use offers notable advantages, including:
> Verification of the catheter tip by nurses, completely independent of other healthcare professionals such as medical staff, X-ray technicians, or orderlies. Therefore, the procedure is more economical and faster.
> Catheter placement in a clean environment, not necessarily in a radiology room. This leads to substantial cost savings by avoiding the need for fluoroscopy, X-rays, patient transportation between departments, and involvement of various healthcare personnel. Moreover, it significantly reduces personal risks associated with exposure to radiation.
> The verification of the catheter tip by nurses, independent of other healthcare professionals like medical staff, X-ray technicians, or orderlies, makes the procedure more cost-effective and expeditious.
> High precision, quickly excluding the possibility of placing the tip in tributary veins (e.g., azygos vein or internal mammary vein) that could be mistaken for the superior vena cava in antero-posterior radiological tests due to overlapping planes.
Suitably sized pocket above the biceps
-
How is the pocket created?
One of the advantages of the PICC-port is its compact reservoir size. Its proper placement ensures that it:
> Does not cause pressure ulcers on the skin due to being in a pocket that is too small for its size.
> Does not flip or rotate due to being in a pocket that is too wide.
A practical tip is to create the subcutaneous pocket gradually, beginning with a small incision and then expanding the space while testing the port. This process helps obtain the optimal space required to avoid complications such as the ones mentioned above.
-
Why should you place the port above the biceps?
To ensure easy puncturing (port access with Huber needle) later on, it is crucial to position the port in a stable area. As a result, the recommended ideal location for placing it is:
> In the middle of the inner arm.
> Above the biceps muscle, which serves as a solid base, offering comfortable support for both the patient and the healthcare professional performing the puncture.
For a Vascular Access Team, the PICC-port serves as a valuable and highly useful device for oncology patients. The steps of its placement technique resemble those of the PICC catheter.
However, inadequate training in ultrasound management may result in complications. It is essential to correctly apply the steps and techniques to ensure the safest possible placement.
Moreover, relying on radiological methods to confirm the catheter tip position does not guarantee accurate catheter location, potentially leading to complications. In contrast, the ECG system provides a safe and cost-effective method.
When compared to a PICC, the new learning aspect for the PICC-port lies in creating the pocket. Adhering to recommendations regarding its location and size can help prevent later challenges with needle access and potential complications.
BIBLIOGRAPHY:
-
Bertoglio et.al, A multicenter retrospective study on 4480 implanted PICC-ports: A GAVeCeLT project, J Vasc Access. January 2022
-
Greca et.al, ECHOTIP: A structured protocol for ultrasound-based tip navigation and tip location during the placement of central venous access devices in adult patients, J Vasc Access. September 2021
-
Zito Marinosci et.al, M. ECHOTIP-Ped: A structured protocol for ultrasound-based tip navigation and tip location during the placement of central venous access devices in pediatric patients, J Vasc Access. July 2021
-
Barone et.al, Neo-ECHOTIP: A structured protocol for ultrasound-based tip navigation and tip location during the placement of central venous access devices in neonates, J Vasc Access. April 2021.