The administration of drugs can give rise to problems such as phlebitis and extravasation among others, which can force us to use various peripheral routes. Over time, different devices have emerged, including midlines. Scientific evidence shows us that this class of devices made with materials of greater biocompatibility, offer great benefits. The aim with the use of this type of catheter is, above all, to conserve the patient’s venous capital, avoid unnecessary punctures and tissue damage, ensure comfort for the patient, and help in the daily work of the nursing staff. However, like any other catheter, midlines are not without complications. In this article, we will find out about midline complications and the possible ways to avoid them.
What is the use of midlines?
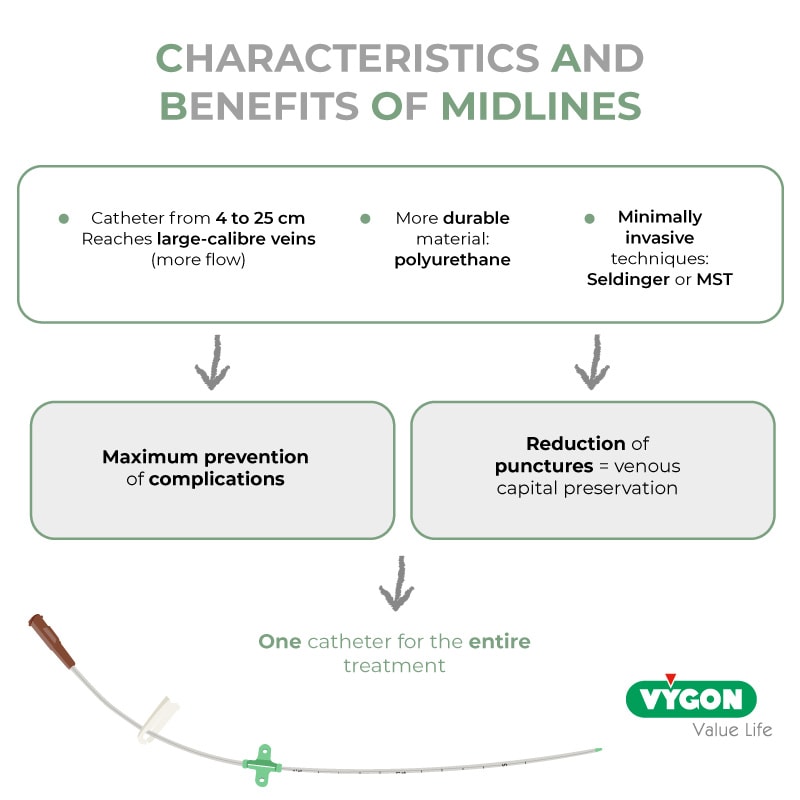
Compared to the short peripheral catheter, the midline catheter allows to:
- Extend the length of the route
- Have only one device for the entire treatment time
- Reduce complications, less risk of infection among others
But we must not forget that it is a peripheral VAD (Venous Access Device) and that it can only be used for the drug administration below:
- With a Ph between 5-9
- Not phlebitic, irritant, vesicant, or antiblastic
- With an osmolarity lower than 600-650 (according to AETSA)
What kind of care is required to avoid midline complications?
Nurses must ensure the proper functioning of the catheter. It is vitally important to proceed to a correct placement, but also to carry out adequate care. The measures below must be followed:

Failure to comply with these points or their improper use, can contribute significantly to the appearance of different complications. They can sometimes be serious and compromise the quality of life of the patient, including his life.
Most common midline complications
The most common midline complications are:
Obstruction
It is the impossibility of infusing and/or non-existence of reflux through the catheter. Obstruction can be total (we cannot infuse, and there is no reflux) or partial (we can infuse, but there is no reflux). It can be caused by not performing a correct washing or sealing (not doing the push-pause and positive pressure techniques) or by the administration of incompatible drugs that form crystals. The use of infusion pumps would also help prevent obstruction since the flow will be permanent.
The existence of an obstruction means that the nursing staff must spend more time trying to unclog it or placing another catheter if it is not successful. This may cause, if it is not done properly, other types of complications.
MARSIs
MARSI stands for Medical Adhesive-Related Skin Injury. It happens when the skin is damaged and an erythema, blister, vesicle, or erosion appears and remains for 30 minutes or more after the removal and/or placement of the dressing or adhesive fixation systems. This can cause pain and discomfort.
The characteristics of the patient’s skin (fragility, atopic skin…) may intervene in the development of this complication, as well as the drugs that are being administered which may intervene in an increased risk of the appearance of lesions (chemotherapy, immunotherapy).
This complication can be caused by the dressing or fixation system itself, as well as the disinfectant agent (chlorhexidine) because the patient may be hypersensitive or have an allergy. Another cause could be not respecting the drying time, placing the fixation devices or the dressing while the skin is wet, as well as not removing or placing the dressing correctly.
Partial or total removal of the catheter
The catheter is no longer placed in the initial position: there is a displacement of the device towards the outside which can also cause a thrombosis.
The removal may be due to an incorrect fixation of the catheter, the disorientation of the patient (the device is withdrawn) or mobilisation of the patient that may lead to the bending and stretching of the device, resulting in partial or complete removal.
Leaving too much length of catheter outside or having an inadequate exit point of the device can make fixation difficult and cause, later, a displacement of the line.
Thrombosis
It is about the existence, formation, or development of a clot in a vein.
When it happens in a vein carrying a catheter, the clot is usually located between the wall of the vein and the catheter.
We can contribute to the prevention of thrombosis by:
- The use of the ultrasound machine
- A correct choice of vein (non-thrombosed, largest possible diameter, straightest, etc.)
- A correct relationship between the calibre of the catheter and the diameter of the vein (1/3)
- Adequate use of protective mesh (not too tight)
- A well-fixed catheter to avoid movement that could erode the endothelium of the vein, cause bleeding, among other things
Apart from the discomfort it causes for the patient, such as pain in the extremity, the appearance of thrombosis entails possible oedema, redness, the appearance of collateral circulation and the need to administer anticoagulants, sometimes, over a long period of time.
Catheter removal should be considered 5-7 days after starting declotting if:
- There is no clinical improvement
- There is an infection
- The catheter does not work because of the thrombosis itself
This also implies an additional cost as it represents more time of care for the nursing staff and of use for the material (doppler ultrasound, transfers to the hospital for control, administration of anticoagulation, placement of a new catheter…).
Infection
It can be at the point of insertion or a catheter-related bacteraemia (CRBSI).
What are the symptoms when it comes to the insertion point?
Phlogosis (redness, induration, discharge) and pain appear. The existence of this infection can lead to the entry of bacteria into the bloodstream which can lead to bacteraemia.

The infection can be caused by an incorrect application of antisepsis measures (no handwashing, no disinfection, no compliance with barrier measures, not performing the care correctly) or not complying with the administration regulations (needleless connector disinfection, change of extension, infusion devices…).
In bacteraemia (systemic infection), fever is present.
When the catheter is responsible for said bacteraemia, hemoculture is also present at its tip or in the intravascular pathway.
It is especially important to avoid this type of complication as it can lead to generalized sepsis, which can compromise the patient’s life.
Other midline complications such as phlebitis and catheter breakage exist.
What is the impact of midline complications?
Non-compliance with a correct insertion procedure, in addition to a bad application of the standardized procedures of maintenance at the level of the catheter exit point, as well as the maintenance of the administration systems, can lead to the midline complications mentioned above.
The need to avoid these complications is obvious as they are a significant cause of morbidity and mortality. They contribute directly to an increase in hospital stay and healthcare costs.
There are different studies that corroborate this fact and indicate that sepsis is the in-hospital clinical process with the highest mortality and cost. According to Dr. Marcio Borges (coordinator of the multidisciplinary sepsis unit at the Son Llatzer hospital in Palma de Mallorca), an episode of sepsis in Spain costs 18,000 euros and the number of deaths caused per year in Spain for this reason is 17,000.
Regarding thrombosis, in the Gavecelt manual, we can find an interesting fact about the costs of an isolated episode: it implies an added cost of 1000 euros (this if no major complications are added).
For the other complications mentioned, the additional cost is evident since it is due to:
- A greater number of cures
- The material used
- Nursing hours
We also have to take into account the quality of life of the patient, the satisfaction with their device, as well as the satisfaction of the staff that cares for them. It is evident that, if the complications are non-existent, it will have a positive impact on all these aspects.
Correct care and maintenance play a fundamental role in the proper functioning of the catheter and in the patient’s quality of life. Compliance with standardized procedures both in insertion (hand washing, skin disinfection, maximum barrier gestures, use of ultrasound, choice of vein, insertion area, appropriate material) and in handling (hand washing, ANTT technique, push-pause technique, positive pressure…) contributes to the reduction of complications. Consequently, it will give us a smaller number of hours dedicated to nursing, reducing costs and days of admission. This will allow us to obtain greater patient satisfaction and an improvement in their quality of life.
Bibliography
- Pittiruti and Scoppettuolo, GAVeCeLT Manual on PICC and midline, Edra edition – 2016
- GAVeCELT Group, DAV Expert website, 2016 – accessed March 2021
- Infusion Nursing Society, Infusion Therapy Standards of Practice – 2021
- CDC Recommendations – 2011
- Ministry of health, social services and equality, Clinical Practice Guideline on Intravenous Therapy with Non-Permanent Devices in Adults – 2014
- Tripathi et.al, The Practice and Complications of Midline Catheters: A Systematic Review, Critical Care Medicine, Volume 49, Issue 2, p e140-e150 – February 2021





