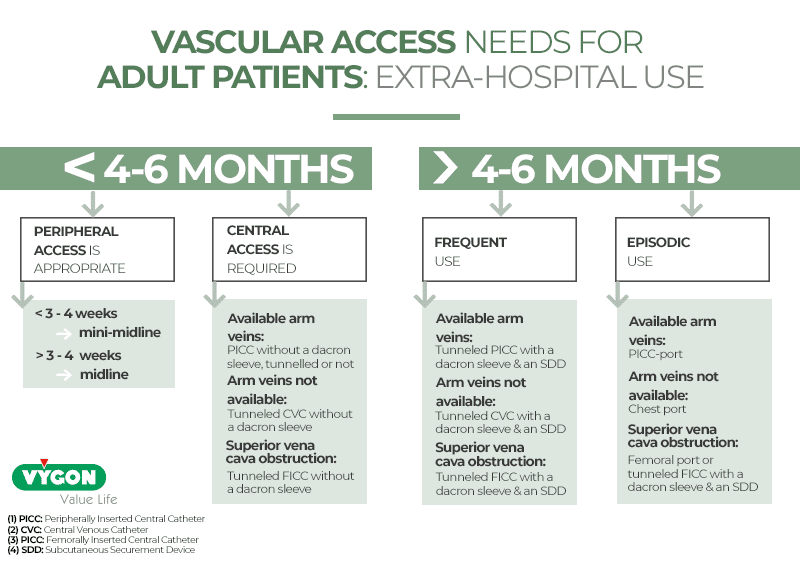
The PICC-port is the latest breakthrough in Venous Access Devices (VADs) and is now included in the DavExpert app’s solution for patients. New studies are showing it is a safe, effective, efficient and goodlooking option for cancer patients.
How has this device evolved over time, and why is it a cost-effective breakthrough today?
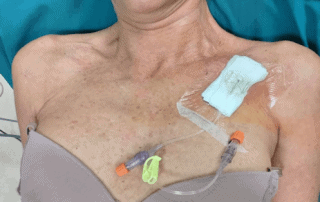
Positioning of the port
TIVADs [1] (Totally implanted vascular access devices) are central venous catheters whose reservoir is placed under the skin. A catheter is inserted into the vein and then connected to the port, which will be placed under the patient’s skin. This method provides great advantages, such as the possibility of leading a normal life since it does not require special external care.
The most popular TIVADs are chest ports, placed in veins in the chest or the neck. At chest level, a pocket can be created. Moreover, these devices are the catheters of choice for long-term but discontinuous treatments such as chemotherapy.
Before the introduction of ultrasound for puncture and insertion of vascular access devices, some ports were placed in the patient’s forearm. They were inserted in visible and palpable veins, normally in the area of elbow flexure, with a port pocket created on the internal part of the forearm. These catheters were known as arm ports or brachial ports.

The incorporation of ultrasound has allowed an evolution in the placement of these catheters and the reduction of potential complications. Thanks to ultrasound, we can approach deep veins in the middle of the arm which can be measured and adapted to the caliber (Fr) of the catheter. Thus, port placement can be done on the inside of the arm, in its upper area. These catheters placed with ultrasound in the arm are known today as PICC-ports.
Accessories for catheter insertion
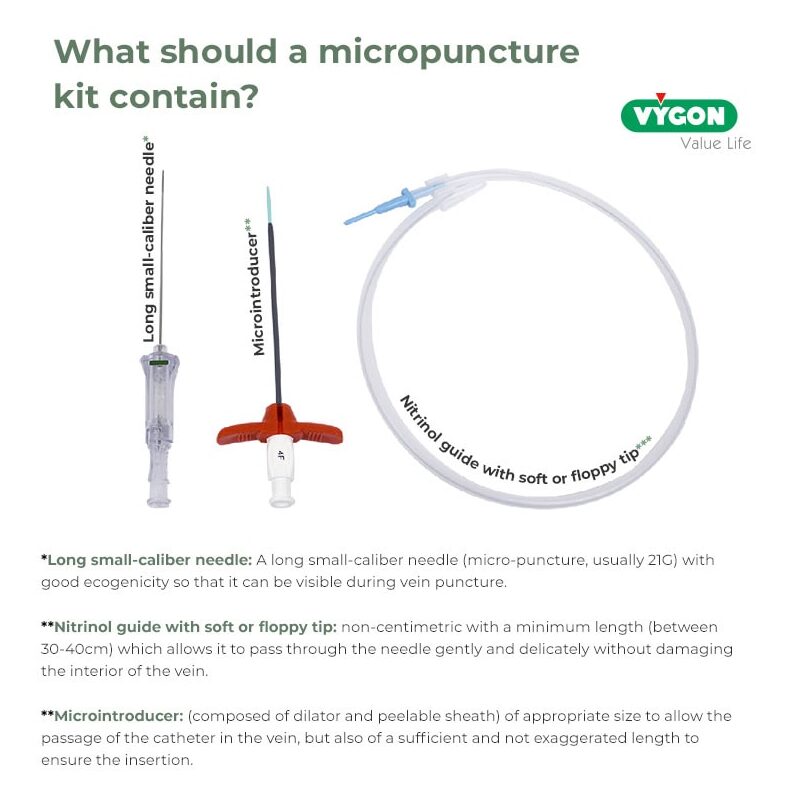
Beyond the materials that the market offers for vascular access, it is important to know about the accessories that come with the catheter, such as the insertion kit. In this case, to be able to talk about PICC-port, we have to associate the concept of the mid-arm ultrasound-guided catheter with the concept of micro-puncture and micro-introduction.
The modified Seldinger technique (recommended by international guidelines and accepted worldwide as the standard for PICC placement in general) has reduced endothelial damage when puncturing veins, especially those of limited size such as peripheral veins.
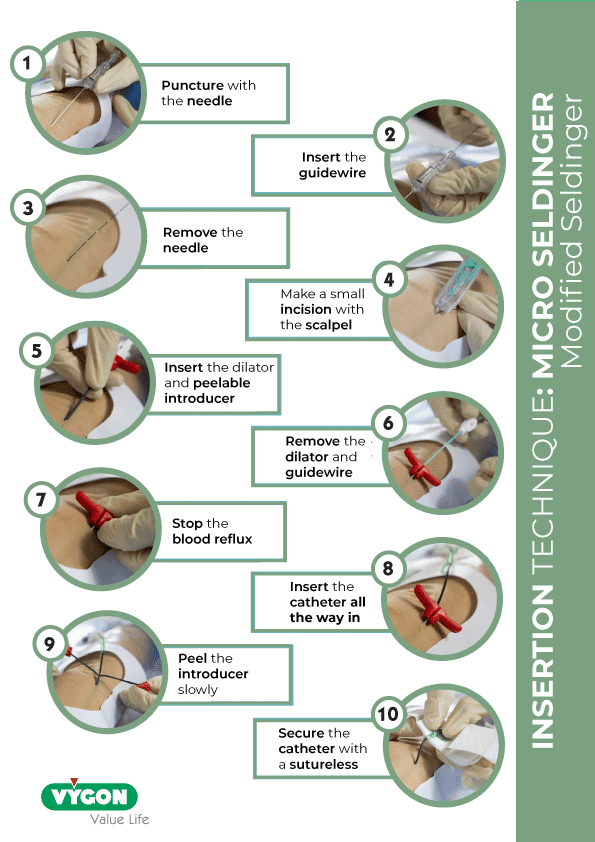
We can identify a PICC-port when its insertion set possesses these essential characteristics that allow a safe modified Seldinger technique.
Cost effectiveness of PICC-port
As we have said before, brachial ports are nothing new: they have been known and used for years in several countries with oncology patients.
However, when we talk about cost-effectiveness, it is necessary to point out certain aspects of the PICC-port compared to the brachial PICC that make it different and, in theory, more effective, such as achieving the desired goal of a safe long-term treatment at a reduced cost.
Above all, to be cost-effective, the insertion of a PICC-Port must be performed by properly trained nursing staff. Over the years, nurses around the world have acquired the skills and abilities to perform ultrasound guided PICC placement as recommended by international guidelines and studies.
Healthcare professionals have undergone theoretical and practical training processes that include aspects as relevant as a comprehensive understanding of the catheter insertion process and not just puncture. They also understand the criteria for selection, material choice, appropriate techniques and technologies for each case, correct usage, patient safety and follow-up, management of immediate and delayed complications, monitoring and care throughout the patient’s process, and removal at the end of treatment.

It has been widely demonstrated that this model of vascular equipment with trained nursing staff reduces costs, increases the efficiency of the entire procedure and brings benefits to the patient and the institution in its complexity.
Insertion of PICC-port
The insertion technique of the PICC-port catheter is similar to the one defined by the SIP-2 [2] protocol internationally recognized by the scientific community and developed by the Italian group GAVeCeLT (Italian group for long-term vascular access). This protocol is fundamentally based on the use of ultrasound for catheter evaluation and insertion and intracavitary ECG for tip location.
In addition, PICC-port insertion can be performed in a clean and controlled environment without having to go to an operating room or having to use x-rays to find the right position. These factors, combined with insertion by nursing staff, allow significant savings in terms of patient safety (no exposure to radiation, avoidance of insertion problems such as pneumothorax, etc.) and in terms of costs (no special room is needed for catheter insertion).

Another concept in the SIP-2 protocol that affects the cost-effectiveness of PICC ports is the use of cyanoacrylate for the superficial closure of the pocket: it makes it possible not to remove stitches, thus avoiding an additional patient visit to the hospital.
The PICC-port is a safe and effective option for patients undergoing prolonged and intermittent treatment. They are not intended to be a replacement for the chest port, as each device has a specific field of action and indications. These devices have evolved to adapt to:
– The need of eliminating/reducing complications
– The new technologies available
– The development of the expert nurse role
-The benefit of the patient and the health organization.
[1] Totally Inserted vascular Access Device
[2] Secure PICC insertion, Second version
Bibliography:
- Kahn, M.L.; Barboza, R.B.; Kling, G.A; Heisel, J.E. Initial Experience With Percutaneous Placement of the PAS Port Implantable Venous Access Device. J Vasc Interv Radiol. 1992, 3 (3), 459-61
- Andrews, J.C.; Walker-Andrews, S.C.; Ensminger, W.D. Long-term Central Venous Access With a Peripherally Placed Subcutaneous Infusion Port: Initial Results Radiology. 1990, 176 (1), 45-7
- Wildgruber, M.; Borgmeyer, S.; Haller, B.; Jansen, H.; Gaa, J.; Kiechle, M.; Meier, R.; Ettl, J.; Berger, H. Short-term and Long-Term Outcome of Radiological-Guided Insertion of Central Venous Access Port Devices Implanted at the Forearm: A Retrospective Monocenter Analysis in 1704 Patients. Eur Radiol. 2015, 25 (3), 606-16
- Bentolila, F.; Gallard, J. Is Radiologic Placement of an Arm Port Mandatory in Oncology Patients?: Analysis of a Large Bi-Institutional Experience. Cancer, 2007, 110 (10), 2331-8
- Fonseca, I. Y. I.; Krutman, M.; Nishinari, K.; Yazbek, G.; Passos Teivelis, M.; Zottele Bomfim, G. A.; Noronha Cavalcantte, R.; Wolosker, N. Brachial Insertion of Fully Implantable Venous Catheters for Chemotherapy: Complications and Quality of Life Assessment in 35 Patients. Einstein (Sao Paulo). 2016, 14 (4), 473-479
- Marcy, P.; Magné, N.; Bailet, C.; Gallard, J.; Valenza, B.; Schneider, M.; Demard, F.; Bentolila, F. Brachial Fluoroscopically Guided Implantation of Venous Port Devices in Oncology Patients. Bull Cancer. 2002, 89 (7-8), 707-12
- Bertoglio, S.; Cafiero, F.; Meszaros, P.; Varaldo, E.; Blondeaux, E.; Molinelli, C.; Minuto, M. PICC-PORT Totally Implantable Vascular Access Device in Breast Cancer Patients Undergoing Chemotherapy. J Vasc Access. 2019 (Ahead of print)
- Burbridge, B.; Chan, I. Y.M.; Bryce, R.; Lim, H. J., Stoneham, G.; Haggag, H.; Roh, C. Satisfaction and Quality of Life Related to Chemotherapy With an Arm Port: A Pilot Study Can Assoc Radiol J. 2016, 67 (3), 290-7
- Burbridge, B; Goyal, K. Quality-of-life Assessment: Arm TIVAD Versus Chest TIVAD J Vasc Access. 2016, 17 (6), 527-534
- Manual GAVeCeLT sobre PICC y Midline. Mauro Pittiruti, Giancarlo Scoppetuolo. 2017. Edizioni Edra.





