The first hour of life, particularly for newborns born prematurely or with very low or extremely low birth weight (<1500 g / <1000 g), is a critical window in neonatal care. Interventions initiated during this period play a decisive role in preventing and managing common complications while supporting the infant’s adaptation to extrauterine life.
This timeframe is referred to in pediatrics as the Golden Hour. The concept, originally applied in emergency medicine to define the first crucial hour of trauma management, was introduced into neonatology in 2009 by Reynolds et al.
The Golden hour refers to the set of early, organized and effective evidence-based interventions and treatments that are performed with the aim of improving outcomes, immediate and long-term, of the preterm infant.
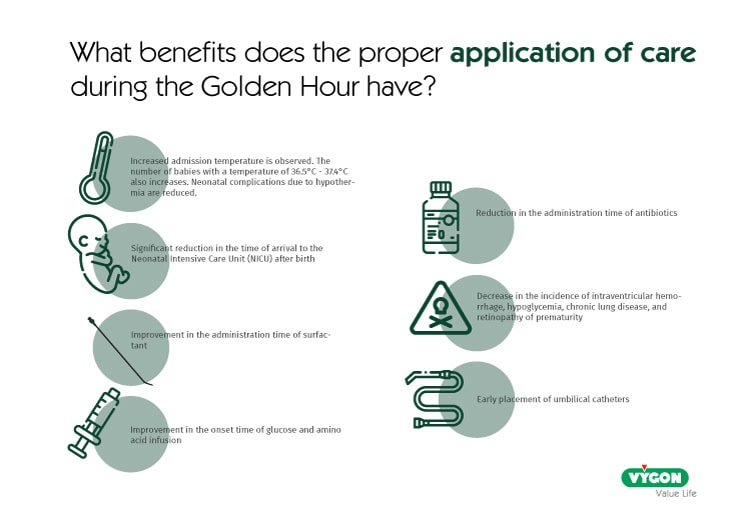
Benefits of Golden Hour Interventions
The proper application of evidence‑based interventions during the Golden Hour leads to significant clinical improvements for preterm infants. These benefits include higher admission temperatures and a marked reduction in hypothermia‑related complications, as well as a faster transfer to the Neonatal Intensive Care Unit (NICU) after birth.
Early and efficient stabilization also shortens the time required for surfactant administration and enables quicker initiation of glucose and amino‑acid infusion, supporting metabolic stability from the outset. Additionally, timely placement of umbilical catheters and reduced antibiotic administration times streamline critical early treatments.
Collectively, these measures contribute to a decreased incidence of intraventricular hemorrhage, hypoglycemia, chronic lung disease, and retinopathy of prematurity, improving both immediate and long‑term neonatal outcomes.
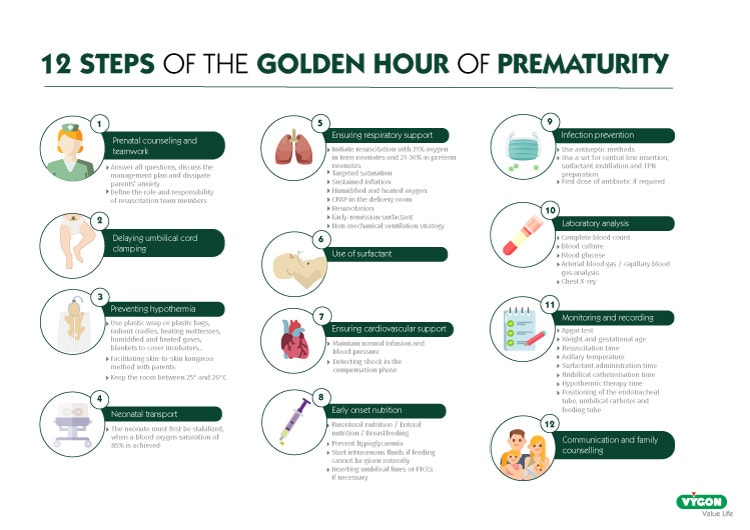
The 12 essential steps of the golden hour
The following are the essential actions to be taken during the first 60 minutes of a preterm newborn’s life:
1. Prenatal counseling and teamwork
This step is prior to the birth of the newborn; however, it should be included in the concept of the golden hour. Two aspects should be taken into account at this point:
- Team management and organization in the context of preterm labor: Pediatric and gynecology teams should work in close collaboration to prevent preterm labor and reduce associated complications. Nursing staff must be informed of the potential admission of the newborn to the NICU to ensure that all necessary equipment and medications are available for rapid postnatal care. All professionals involved in the management of preterm patients should possess the knowledge and skills required in the delivery room.
- Information and support for parents in the context of prematurity: One key objective is to keep parents fully informed. Families should be guided and have their questions addressed before the preterm birth. Healthcare professionals must assist and advise them on neonatal resuscitation and, if necessary, on palliative care.
2. Delaying umbilical cord clamping
Recent research on umbilical cord clamping recommends delaying the procedure for 30 seconds to 1 minute in preterm infants, who do not require resuscitation at birth. For those requiring resuscitation, cord clamping should not be performed.
Delayed clamping offers several benefits for these patients, including:
- Improved pulmonary blood flow
- Reduced need for transfusions
- Immediate support for hemodynamic transition
- Lower risk of intraventricular hemorrhage
- Decreased incidence of necrotizing enterocolitis
3. Preventing hypothermia
In premature infants, the risk of hypothermia during the first minutes of life is very high due to their limited capacity for thermoregulation. The incidence in low–birth weight and low–gestational age newborns ranges from 31% to 78%
- Moreover, effective thermoregulation in premature infants is essential because:
- For every 1°C drop in body temperature, the risk of death increases by 28%.
- The likelihood of an Apgar score below 7 is higher.
- The risk of intraventricular hemorrhage increases.
- The incidence of sepsis and hypoglycemia rises.
- The probability of developing Respiratory Distress Syndrome (RDS) increases
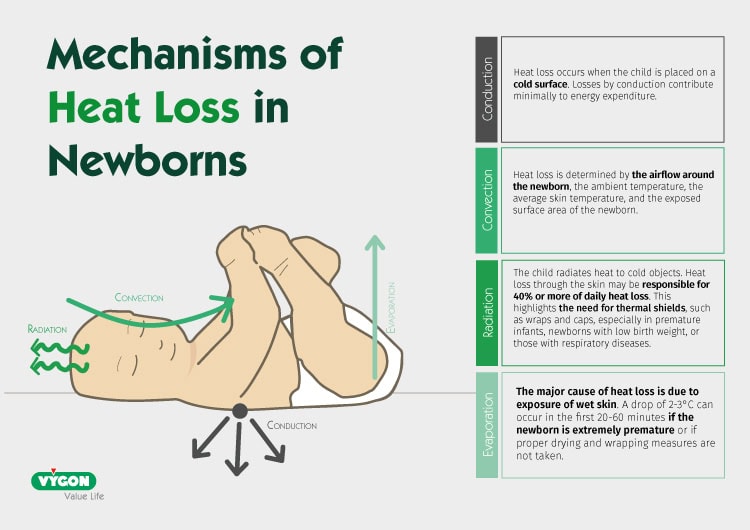
To support thermoregulation in neonatal patients and prevent hypothermia and its complications, healthcare professionals can implement several strategies within their department:
- Temperature control in the delivery room: The World Health Organization (WHO) recommendations for preventing hypothermia include a delivery room heated to 25°C.
- Use of plastic/polyethylene wraps: Multiple reviews identify covering the body and head of newborns with plastic wraps as the most effective method, at less than 28 weeks of gestation, of reducing heat loss.
- Early initiation of the kangaroo method: When clinically feasible, skin-to-skin contact in the first minutes of life improves neonatal temperature regulation compared with the use of a conventional incubator.
- Protection of the newborn from drafts: Ensuring the newborn is shielded from air currents reduces unnecessary heat loss.
- Additional heat sources can further support temperature stability: radiant warmers, heated mattresses, pre-warmed linens and incubators, humidified and warmed resuscitation gases, and blankets to cover incubators during transport can also be used.
Hypothermia in newborns, how to prevent it?
4. Transport during the golden hour
- In the Golden Hour the neonate must first be stabilized, transport will not begin until a blood oxygen saturation of 85% is achieved.
- During the transfer process, care will continue with the aim of maintaining body temperature and maintaining vital functions.
Optimal Thermal Control of the Newborn in Transport Settings
5. Ensuring respiratory support
In most cases, newborns are well adapted to extrauterine life; however, preterm infants may have difficulty initiating effective breathing after birth because of a lack of surfactant or because their lungs are not mature.
The goal of supporting the respiratory system is to assist in the transition of gas exchange from the mother’s placenta to the lung.
- In newborns with spontaneous breathing, non-invasive ventilation, like CPAP (Continuous Positive Airway Pressure) is recommended, in order to improve functional residual capacity and oxygenation.
- If the newborn is not breathing spontaneously, invasive ventilation via an endotracheal tube is recommended for resuscitation.
6. Surfactant administration
Preterm infants are born with reduced surfactant reserves, making early replacement therapy essential in managing respiratory distress syndrome (RDS). Current evidence favors “early rescue” administration within the first hour of life, combined with appropriate respiratory support. Less invasive methods, such as LISA, is preferred in infants with spontaneous respiratory effort and associated with lower rates of mechanical ventilation, bronchopulmonary dysplasia (BPD), and mortality. Animal-derived and protein-containing synthetic surfactants show comparable efficacy.
7. Supporting the cardiovascular system
Early cardiovascular support involves assessing heart rate with the goal of establishing normal heart rate, blood pressure, and perfusion in both preterm and term infants.
For newborns requiring cardiopulmonary resuscitation (CPR), continuous heart rate monitoring is recommended. This monitoring can be done using pulse oximetry or electrocardiogram (ECG), with ECG providing greater accuracy during the first two minutes of the newborn’s life.
8. Early initiation of nutrition and administration of amino acids
In utero, the placenta supplies the fetus with essential nutrients. Once the umbilical cord is cut, this supply is interrupted, making early nutritional support a priority for both preterm and term infants.
9. Prevention of sepsis
Neonatal sepsis and prematurity are the two most common causes of neonatal mortality and morbidity. While several strategies exist to prevent neonatal sepsis, the most important is maintaining strict aseptic measures during neonatal care.
10. Laboratory studies
All necessary laboratory studies for the neonate should be performed during the Golden Hour, as opportunities to intervene later are limited and decisions may fall outside the initial treatment plan.
Recommended studies include complete blood count, blood culture, capillary glucose, arterial or capillary blood gases, biochemistry, and chest X-ray.
11. Monitoring and recording
All vital parameters of the neonate should be monitored and documented in the medical record. It is essential to record interventions during the first hour of life, including the exact times, to evaluate the effectiveness of care.
Records should include the following tests and parameters:
- Apgar score
- Weight and gestational age
- Axillary temperature on admission to the NICU
- Time and details of resuscitation interventions
- Position and size of the endotracheal tube
- Ventilation and CPAP time
- Time of surfactant administration
- Umbilical catheterization time
- Umbilical catheter position
- Time of first drug administration
- Start time of fluid therapy and TPN
- Time and parameters of first feeding
- Depth of nasogastric tube fixation
- Recorded complications
12. Communication and family counseling
During this first vital hour, when numerous interventions take place in a stressful context with a vulnerable patient, it is essential to keep the family continuously informed about their child’s condition and the care being provided.
Conclusion
The Golden Hour represents a critical and evolving strategy to optimize both immediate stabilization and long-term outcomes for neonates. Evidence supports that structured and standardized protocol during this crucial first hour reduce complications such as hypothermia, bronchopulmonary dysplasia, and retinopathy of prematurity, ultimately improving survival and morbidity profiles. However, variability in practice remains a challenge, highlighting the importance of ongoing education, use of standardized checklists, and sustained multidisciplinary collaboration. Ensuring commitment to the Golden Hour principles remain essential to reach its full potential.
Bibliography
- Diaz C., M. (2018). Extreme prematurity: initial management. In F. Barrera Quezada, Guías de Práctica Clínica en Pediatría(8th ed., pp. 191-199). Santiago de Chile: Servicio de Salud Metropolitano central Hospital Clínico San Borja Arriarán and Facultad de Medicina de Universidad de Chile. Retrieved from: https://www.savalnet.ec/revistas/guias_pcp_2018/files/assets/basic-html/page-191.html
- Doyle, K., & Bradshaw, W. (2013). The golden hour. In Z. Ortiz, C. Perrotta, G. Bauer, A. Messina, J. Anciola & M. Prina, Rights of preterm newborns(1st ed., pp. 42-45). Argentina: UNICEF. Retrieved from: https://books.google.es/books?id=1Z5HAwAAQBAJ&pg=PA42&dq=la+hour+of+gold+reci%C3%A9n+borns&hl=en&sa=X&ved=2ahUKEwi-k6O15bfwAhU8BWMBHYusBV8Q6AEwAHoECAQQAg#v=onepage&q=la%20hora%20de%20oro%20reci%20reci%20C3%A9n%20nacidos&f=false
- W. Croop, S. (2019). The Golden Hour: a quality improvement initiative for extremely premature infants in the neonatal intensive care unit. Springer Nature America. Retrieved from: https://vygoncom-my.sharepoint.com/personal/tpolo_vygon_com/Documents/Posts/Golden%20Hour/s41372-019-0545-0.pdf?CT=1621940567663&OR=ItemsView
- Faunes, M., Avila, A., Soto, P., Ulloa, A., & Rojas, S. (2016). The golden hour: care of the preterm newborn under 32 weeks gestation during the first hour of life (pp. 1-5). Peru: Hospital Clínico Pontificia Universidad Católica de Chile and Universidad Austral Buenos Aires Argentina. Retrieved from: http://www.manuelosses.cl/pneo/HORA%20DE%20ORO.pdf
- Shah, V. et all. (2017). Golden hour management practices for infants <32 weeks gestational age in Canada. Toronto. Reviewed at: https://vygoncom-my.sharepoint.com/personal/tpolo_vygon_com/Documents/Posts/Golden%20Hour/pxx175_Canada.pdf?CT=1621940561643&OR=ItemsView
- Sharma D. National Institute of Medical Science, Jaipur, Rajasthan India. The golden hour in the preterm and term newborn. Matern Health Neonatol Perinatol.2017 19;3:16. DOI: 10.1186/s40748-017-0057-x Ajouter au projet Citavi par DOI. Review it: https://www.spao.es/images/publicaciones/boletinesSPAO/pdf/pdf-boletin-69.pdf
- Yui Hifume, R., Polo Gonzalez, T., Espín Galvez, J., & Diez- Delgado, J. (2016). Golden hour: preterm newborn. Boletín De La Sociedad De Pediatría De Andalucía Oriental, (Volume 10 (Nº49), 152-167. Retrieved from: https://www.spao.es/images/publicaciones/boletinesSPAO/pdf/pdf-boletin-69.pdf
- Viche Martínez, Z. (2018). Theoretical foundations for nursing care in The golden hour of the premature newborn. Universidad autónoma de San Luis Potosí.






