As the GAVeCeLT group (1) stated in their manual on PICCs and midlines regarding the evolution of PICC use, the introduction of ultrasound in the 2000s has been a breakthrough in the field.
In this article, we delve into the utility of ultrasound in the field of vascular access.
Ultrasound for internal vein visibility and complications reduction:
The damage caused by punctures used to be quite significant, given the use of blind puncture and the calibre of outdated introducers from 30 years ago. Ultrasound became crucial by integrating with the less invasive Microseldinger technique, employing a 21G needle and a flexible, thin guide.
Having access to information about the shape, diameter, and trajectory of the veins provides much clearer guidance on how to approach the insertion of a PICC or midline catheter. Thanks to ultrasound, the insertion is less traumatic and helps prevent many subsequent complications such as extravasation, phlebitis, and hematomas. It also offers a great advantage: accessing deep arm veins (basilic, cephalic) of larger calibre veins that are not visible to the naked eye.
The literature leaves no doubt about the relevance and necessity of ultrasound for the placement of medium to long-term intravenous catheters. It indeed increases the first-attempt success rate and reduces procedural time (2, 3, 4).
Understanding ultrasound waves:
In the sound wave spectrum, ultrasound waves extend beyond 20,000 Hz, surpassing the audible range of sounds to humans:
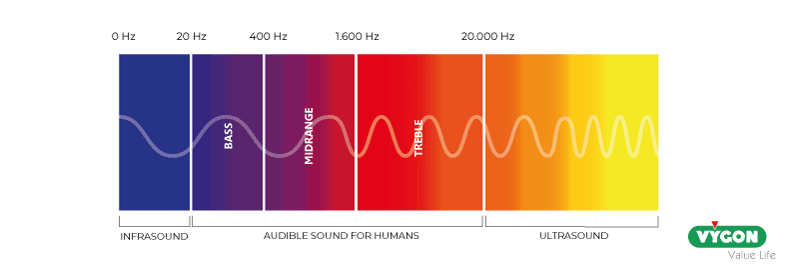
(5)
These waves are present in nature. Bats and dolphins, for example, have an internal “radar” that operates by emitting ultrasound waves. They quickly receive the echoes and, by creating a map of their surroundings, navigate accordingly.
In ultrasound imaging, waves pass through the examined tissues, with a fraction returning to the transducer to create an image. The structures’ appearance in the image depends on the density of the traversed tissues.
So, how is an image generated from ultrasound?
The ultrasound machine consists of a transducer or probe. This device converts electrical energy into mechanical energy and vice versa. The piezoelectric crystals within the transducer enable the energy conversion.
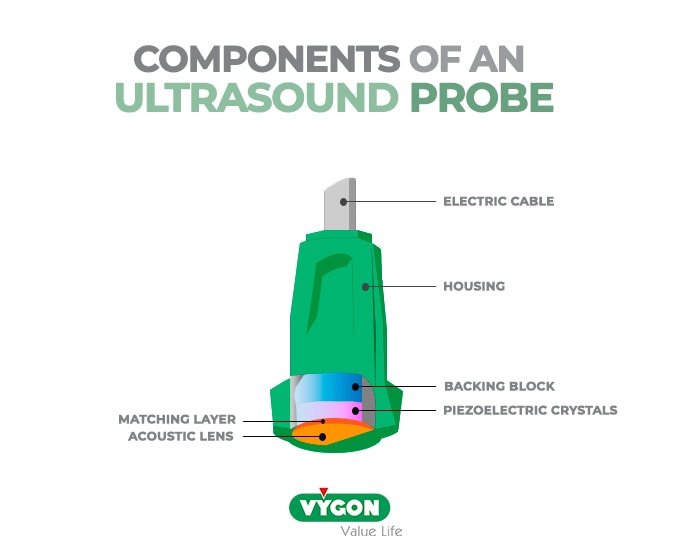
The emitted ultrasound beam from the probe is very thin, with a thickness of 1 mm.

(6)
The shape of the transducer beam is related to the footprint of the transducer. Higher frequency leads to better image resolution but less depth penetration, and vice versa.
There are three fundamental types of probes:
- Linear probe: High frequency, up to 18MHz, with a footprint of about 4cm and a depth of 5-6cm (used for vessels, nerves, muscles, etc.).
- Convex probe: Low frequency, <6MHz, with a footprint of 6cm and a depth of 30cm (used for abdominal and obstetric ultrasound).
- Sector probe: Low frequency, <6MHz, with a footprint of 21cm and a depth of 35cm (used for cardiac ultrasound). (6,7)

(6)
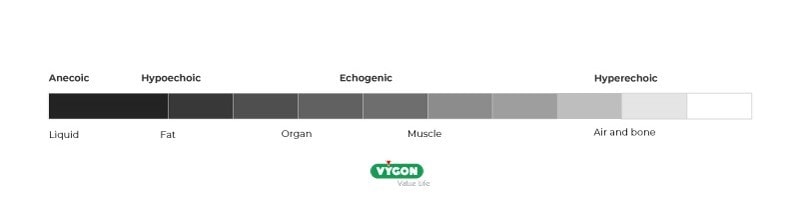
The computer system is responsible for transforming the information received by cable or Wi-Fi into interpretable images:

Depending on the amplitude of the waves that reach the transducer, the ultrasound image is formed with different shades of grey (brighter shades indicate higher amplitude received by the probe):
Characteristics and parameters of ultrasound-guided puncture:
- Manipulation of the probe:
– The position and orientation of the probe are of great importance. During the learning process, these are among the first skills to be acquired: maintaining sufficient contact with the skin using gel, adjusting the angle to visualize the desired image, and knowing how to move the probe based on the visible structures.
– Concerning probe orientation relative to the image, the probe marker should be aligned to the right of the patient in the transverse view and towards the head in the longitudinal view.
– The ultrasound beam creates a sectional view of the structures based on the position of the probe: working with the longitudinal view (“in-plane”) provides an image along the length of the vein, while the transverse view (“out of plane”) provides an image across the width of the vein (slices).
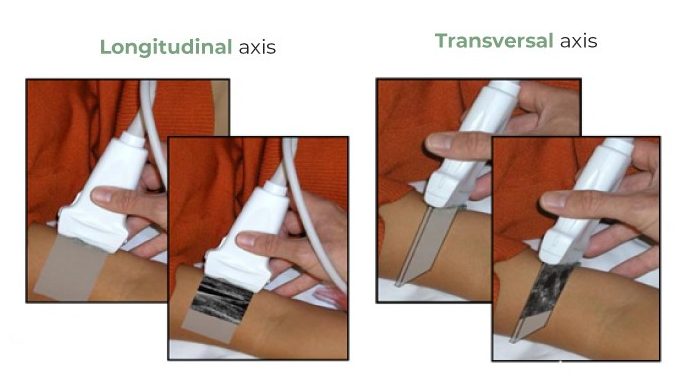
(6)
- Recognition of structures:
Another essential skill to have when using an ultrasound in vascular access is the ability to recognize different structures:
- Veins: Recognized by their circular shape in transverse view. They collapse under pressure when applying the probe to the skin.
- Arteries: Recognized by their circular shape in transverse view, pulsation, and resistance to collapse when applying pressure with the probe on the skin.
- Nerves: Recognized by their honeycomb-like structure.
An experienced eye trained to distinguish these three groups will also avoid risky areas, such as the famous “Mickey Mouse” pattern. In the arm, the brachial artery (Mickey’s head) runs close to the brachial veins (Mickey’s ears), which may be candidates for cannulation. It is however not advisable due to the proximity of the artery and the median nerve.
- Ultrasound gain:
It’s important to consider that ultrasound beams progressively weaken as they interact with tissues. The deeper the penetration, the higher the attenuation of the beam. To compensate for this phenomenon, it is important to be able to adjust the gain. Certain models have an automatic gain mode.
- Depth:
Being comfortable while placing a catheter is an important criterion, and having the best possible ultrasound image is part of it. It is necessary to adjust the image based on the depth of the target structure. It is generally recommended to start with greater depth and then adjust to the desired zone. In general, the depth is indicated in cm or mm on a scale located at the side of the image. As mentioned earlier, the depth directly depends on the frequency of the emitted ultrasound (probe types).
- Vein Measurement:
In the placement of Vascular Access Devices (VADs), it is essential to observe the following: the catheter should occupy one-third of the vein lumen. Therefore, the measurement provided by the ultrasound machine is a very useful tool. Depending on the model, this measurement can be automatic or manual (providing more precise results), allowing the appropriate catheter selection.
What type of Vascular Access devices should be used with an ultrasound?
Ideally, an ultrasound can be used with any type of catheter since it allows to visualize the procedure. For example, in the United States, the ultrasound-guided placement of medium/long-term catheters is mandatory and can also be used for short peripheral routes. In Europe, ultrasound is used for patients with Difficult Insertion of Vascular Access (DIVA) and for catheters that require deep vein cannulation, such as midlines, PICCs, PICC-ports, central catheters, ports, and Hickman catheters. With proper training, ultrasound has shown to be a reliable and nurse-controlled method for vascular access placement (9, 10).
BIBLIOGRAPHY
- Manual GAVeCeLT on PICC and midline – 2016.
- Intensive Care Med (2012) – International evidence-based recommendations on ultrasound-guided vascular access – https://link.springer.com/article/10.1007/s00134-012-2597-x
- Saldanha de Almeida (2016) – Vascular access: the impact of ultrasonography – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5221386/
- The American Journal of Emergency Medicine (2010) – Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach –https://www.sciencedirect.com/science/article/abs/pii/S0735675708008164
- Sensor ultrasonidos Arduino para medir distancias – https://programarfacil.com/blog/arduino-blog/sensor-ultrasonico-arduino-medir-distancia/
- Courtesy of Fujifilm – Sonosite
- Ecografia facil – https://ecografiafacil.com/2018/01/01/11-tipos-de-transductores/
- https://secip.com/wp-content/uploads/sites/10/2018/09/1-FUNDAMENTOS-BASICOS-DE-ECOGRAF%C3%8DA.pdf
- Competency for ultrasound-guided peripheral intravenous catheter insertion for nurses – https://www.ivteam.com/intravenous-literature/competency-for-ultrasound-guided-peripheral-intravenous-catheter-insertion-for-nurses/
- The ultrasound as a complementary method for the implantation of the central venous catheter of peripheral insertion (PICC) – https://eprints.ucm.es/49810/







