To mark World Heart Day, we take a look at the most significant innovations in the field of cardiology. From advances in imaging and diagnostic technology to life-saving devices, the heart of medicine is beating stronger than ever.
Cardiovascular innovation on World Heart Day
Every year on 29 September, we celebrate World Heart Day, a date that invites us to reflect on cardiovascular health, one of the main public health concerns globally.
Recent years have marked a significant turning point in the field of cardiology, characterised by revolutionary advances in the prediction, prevention and treatment of cardiovascular disease.
Although cardiovascular diseases are no longer the leading cause of death and disability in some countries—such as the United Kingdom, where they have recently been surpassed by cancer—they still account for approximately one in three deaths worldwide. Their effective treatment relies on both preventive strategies and ongoing clinical and technological advancements.
Conditions such as ischaemia, cerebrovascular disease, heart failure and hypertension continue to pose a threat to the population and justify the efforts of professionals to raise awareness of the importance of prevention and to persevere in achieving scientific advances in this field.
This article focuses on five key areas of recent transformation: prevention, advances in clinical cardiology, minimally invasive interventions, innovation in cardiovascular devices, and the threat to cardiovascular health posed by the proliferation of microplastics.
Prediction and prevention: The new frontier of cardiovascular risk
PREVENT risk calculator: Revolutionising risk assessment.
One of the most significant developments of the past year has been the validation of the PREVENT risk calculator, developed by scientific experts in collaboration with the American Heart Association. This tool represents a paradigm shift in cardiovascular risk assessment by calculating the 10- and 30-year risk of total cardiovascular disease using measures of cardiac, renal, and metabolic health.
What distinguishes PREVENT from previous calculators is its inclusive approach: it does not consider race or gender as risk factors, but it does include measures of social disadvantage. The validation of this tool used data from more than 6 million American adults, demonstrating superior accuracy in predicting cardiovascular risk compared to the previously used Pooled Cohort Equation (PCE).
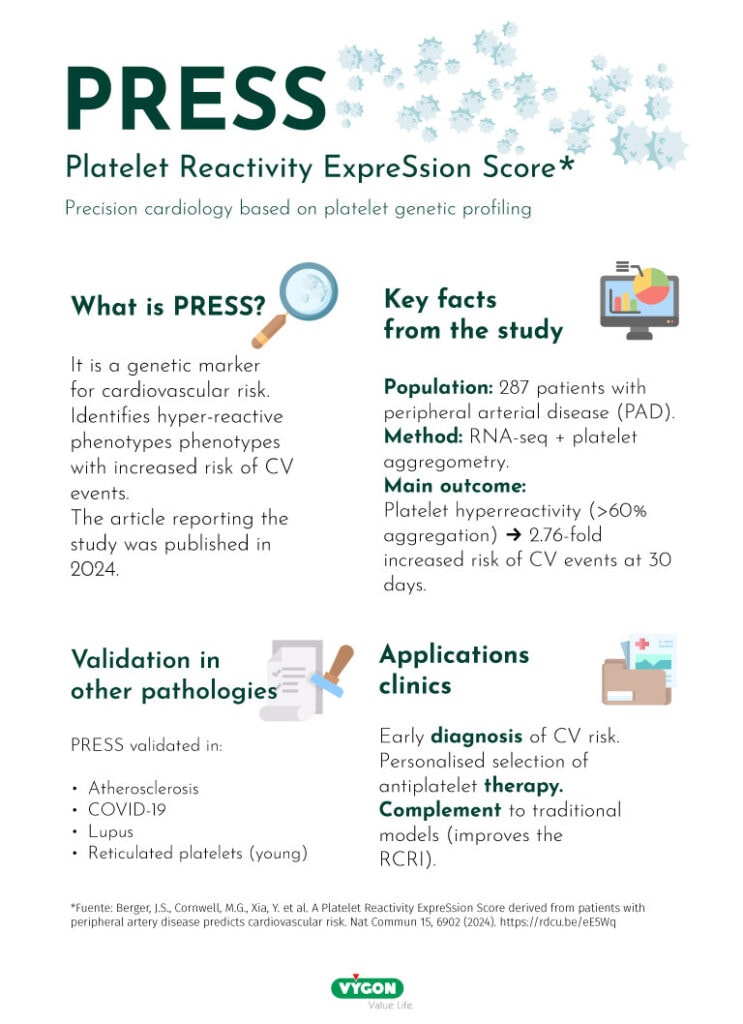
PRESS: Genetic identification of platelet hyperactivity
The development of the Platelet Reactivity ExpreSsion Score (PRESS) represents another crucial advance in personalised cardiovascular medicine. This tool uses genetic signatures to assess platelet reactivity, identifying patients at risk of platelet hyperactivity who could benefit from antiplatelet therapy.
The genetic research that led to the development of PRESS analysed genetic differences between people with peripheral arterial disease and hyperactive platelets, comparing them with healthy individuals. This approach promises to revolutionise the early identification of patients at risk of atherothrombotic events.
Recent advances in clinical cardiology
State-of-the-art cardiac imaging
Diagnostic accuracy has taken a qualitative leap forward in recent years thanks to new advanced imaging tools. For example, three-dimensional (3D) echocardiography allows real-time, high-fidelity visualisation of the heart’s structures, facilitating the early detection of valvular and myocardial abnormalities. This technique, which is particularly useful in interventional cardiology, improves the planning of procedures such as valve repairs and septal defect closures.
High-resolution cardiac magnetic resonance imaging (CMRI) has established itself as the gold standard for assessing ventricular function, myocardial fibrosis, and perfusion without the use of ionising radiation. Thanks to fast sequences and advanced reconstruction algorithms, it is now possible to obtain accurate images even in patients with irregular heart rhythms.
Another highly impactful tool is non-invasive computed tomography angiography (CTA), which has revolutionised the assessment of coronary artery disease. Using high-speed acquisition techniques and three-dimensional reconstruction software, cardiologists can visualise the coronary arteries in great detail, detect atherosclerotic plaques and assess their composition without the need for catheterisation.
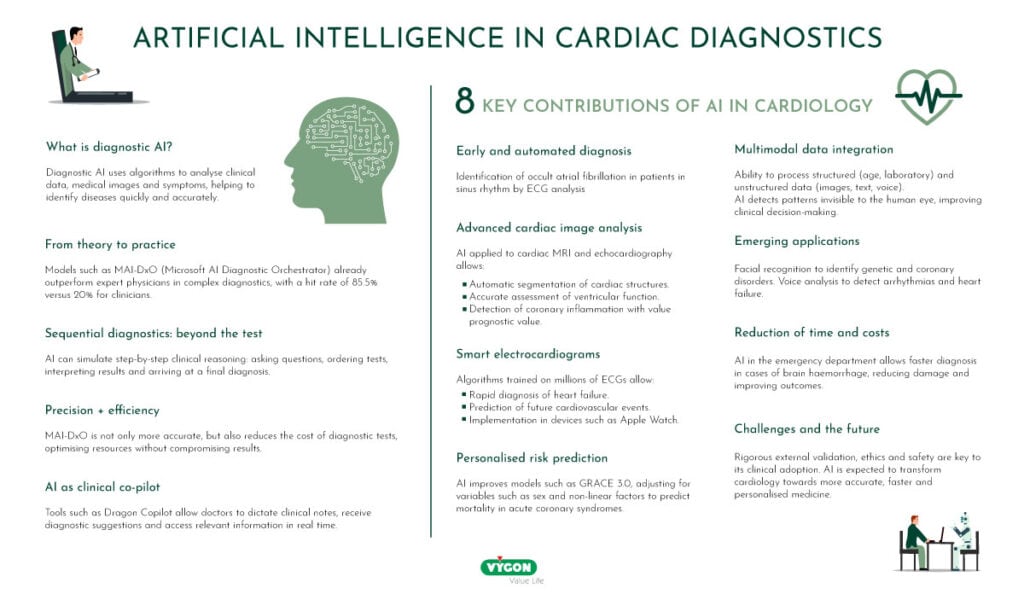
Artificial intelligence applied to diagnosis
The emergence of artificial intelligence (AI) in the medical field has opened up new frontiers in the analysis and interpretation of complex data. In cardiology, AI is used to detect subtle patterns in electrocardiograms (ECGs), predict the risk of adverse events, and optimise clinical follow-up.
Models trained with millions of records can identify arrhythmias, ventricular dysfunction, or early signs of heart failure, even before the clinician notices any abnormalities. In addition, AI applied to cardiac imaging helps to delineate structures more accurately, automatically segment cavities and tissues, and estimate volumes and ejection fractions in a reproducible manner.
Innovations in prevention and treatment: minimally invasive procedures
Structural heart therapies have evolved thanks to percutaneous techniques that reduce the need for open-heart surgery. Two prime examples are transcatheter aortic valve replacement (TAVR) and transcatheter mitral valve repair (TMVR), which have demonstrated excellent efficacy and safety, especially in elderly patients or those with comorbidities that contraindicate conventional surgery.
TAVR involves implanting a prosthetic valve through a catheter inserted via the femoral artery, avoiding thoracotomy. Studies show that this technique offers similar—and even higher—medium-term survival rates than traditional surgery, with shorter hospital stays and faster recovery.
TMVR, meanwhile, has made it possible to address secondary mitral regurgitation with devices such as clips and valve anchors that correct coaptation without the need for extracorporeal circulation. These interventions, guided by real-time transoesophageal echocardiography, are changing the therapeutic paradigm and ushering in a new era in structural cardiology.
Research and development in cardiovascular devices
Innovation in implantable devices
Progress in implantable cardiovascular devices has been rapid, both in functionality and design. Current pacemakers incorporate sensors that detect the patient’s physical activity and dynamically adjust the heart rate, promoting ventricular synchrony and reducing the risk of dysfunction.
Implantable cardioverter defibrillators (ICDs) incorporate more accurate detection algorithms that prevent unnecessary shocks and enable real-time remote monitoring, improving remote follow-up. In addition, some newer models are placed subcutaneously, avoiding complications associated with intravascular electrodes.
In the field of ventricular assistance, state-of-the-art systems offer improvements in energy efficiency, reduced size and greater biocompatibility, allowing for a longer service life with less risk of thrombosis. These pumps, in many cases a bridge to transplantation or even as a definitive therapy, are now an established reality.
Orthotopic artificial heart (Carmat)
In recent years, work has been done to improve the orthotopic artificial heart, a pump that is placed in the chest to replace damaged ventricles and valves in the heart. The total artificial heart is primarily a temporary measure (often referred to as a “bridge to transplant”) to keep the heart pumping while a person waits for a heart donor to undergo a heart transplant.
Although cardiologists and cardiac surgeons have been working on the dream of an artificial heart for more than 60 years ( ), it was not until the end of 2013 that the first implantation of an autonomous and self-sufficient heart was performed. This prosthesis, made from haemocompatible biological tissues of animal origin, generates blood circulation autonomously at a physiological level.
The heart is equipped with electronic sensors and a complex electromechanical system that detects the patient’s position—standing, sitting, or lying down—as well as the venous and arterial pressure linked to their activity, thereby adapting the heart rate and fluid to different situations.
Environmental considerations: microplastics and cardiovascular risk
A prospective multicentre study has identified a possible link between exposure to microplastics and nanoplastics and an increased risk of cardiovascular disease. The study found polyethylene in the carotid artery plaques of more than 58% of patients, with those with microplastics in their plaques showing a higher composite risk of heart attacks, strokes and death.
Researchers at the University of Jaén (UJA), in collaboration with clinicians from the Intensive Care Unit at the University Hospital of Jaén, are currently conducting a study focusing on the presence of microplastics and nanoplastics in the serum of heart attack patients.
Conclusions
The heart of cardiology is beating stronger than ever thanks to innovation. Advanced imaging tools, artificial intelligence applied to diagnosis and minimally invasive therapies are reshaping clinical practice, enabling a more precise, individualised and less aggressive approach. At the same time, new implantable devices and collaborative research projects are opening up previously unthinkable opportunities for patients with cardiovascular disease.
On this World Heart Day, it is essential not only to celebrate these achievements, but also to redouble our commitment to more preventive, technological and patient-centred medicine. The future of the heart is in good hands… and good minds.
Bibliography
- American Heart Association. AHA names biggest advances in cardiovascular research for 2024. Available at: https://www.heart.org/en/around-the-aha/aha-names-biggest-advances-in-cardiovascular-research-for-2024
- Khan SS, Coresh J, Pencina MJ, et al. Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney-Metabolic Health: A Scientific Statement From the American Heart Association. Circulation. 2024;149(11):e1-e30.
- Patel KV, Pandey A, de Lemos JA, et al. Comparison of the PREVENT equations and Pooled Cohort Equations for Predicting Cardiovascular Disease. JAMA. 2024;331(22):1896-1906.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104.
- Butler J, Filippatos G, Siddiqi TJ, et al. Effects of finerenone in patients with heart failure and mildly reduced or preserved ejection fraction. N Engl J Med. 2024;391(16):1475-1485.
- Lim HS, Gustafsson F, Merkely B, et al. Effects of transcatheter mitral valve repair in heart failure. N Engl J Med. 2024;391(24):2203-2214.
- Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389(24):2221-2232.
- Kosiborod MN, Abildstrøm SZ, Borlaug BA, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023;389(12):1069-1084.
- Perkovic V, Tuttle KR, Rossing P, et al. Effects of semaglutide on chronic kidney disease in patients with type 2 diabetes. N Engl J Med. 2024;391(2):109-121.
- Solomon SD, McMurray JJV, Borlaug BA, et al. Tirzepatide in heart failure with preserved ejection fraction and obesity. N Engl J Med. 2024;391(21):1983-1993.
- Kelly AS, Bensignor MO, Hsia DS, et al. Liraglutide for children 6 to <12 years of age with obesity – a randomised trial. N Engl J Med. 2024;391(21):1968-1982.
- Desai AS, Solomon SD, Shah AM, et al. Effect of sacubitril-valsartan vs enalapril on aortic stiffness in patients with heart failure and reduced ejection fraction. JAMA. 2019;322(11):1077-1084.
- Olivotto I, Oreziak A, Barriales-Villa R, et al. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2020;396(10253):759-769.
- Ho CY, Mealiffe ME, Bach RG, et al. Evaluation of mavacamten in symptomatic patients with nonobstructive hypertrophic cardiomyopathy. J Am Coll Cardiol. 2020;75(21):2649-2660.
- Thiele H, Zeymer U, Akin I, et al. Extracorporeal life support in infarct-related cardiogenic shock. N Engl J Med. 2023;389(14):1286-1297.
- Dominic King & Harsha Nori The Path to Medical Superintelligence https://microsoft.ai/new/the-path-to-medical-superintelligence/







