One in ten children with a central venous catheter (CVC) develops a device-associated bloodstream infection. 2
Want to know how to prevent bacteremia and central venous catheter-related infection? Dr. Paco Escribá, anesthesiologist FEA Anesthesiology for children, PhD at the Hospital Universitari i Politècnic La Fe de Valencia, tells you.
WHAT WILL YOU FIND IN THIS ARTICLE?
- Adverse effects related to hospitalization
- Vascular access-related infection
- Is it possible to reduce CVC-related infection?
- Hand hygiene
- Use of chlorhexidine in skin preparation
- Total barrier measures during central venous catheter placement
- Site of line placement
- Removal of unnecessary catheters
- Hygienic handling of catheters
- Use of ultrasound
Want to know more? Stay on this page and read the full post.
One in ten children with a central venous catheter (CVC) develops a device-associated bloodstream infection. 2 This problem is usually caused by inadequate maintenance of central lines and leads to increased healthcare costs, increased likelihood of sepsis or even morbidity and mortality. 3
Another major problem, which can also increase the probability of suffering a central venous catheter-related infection, is occlusion, mainly due to the interaction of fibrin, thrombus and biofilms. 2
An important indicator of patient safety is the incidence of adverse events occurring in hospitals (AE’s) including bacteremia and phlebitis among others.
ADVERSE EFFECTS LINKED TO HOSPITALIZATION
The National Study on Adverse Effects Linked to Hospitalization (NSAEH), carried out in 24 hospitals of the Spanish National Health System in adult patients, concludes that 42.8% of AE’s were avoidable. 5
- In 66.3% of all AE’s, new procedures, such as radiodiagnostic tests, were required. 5
- Additional treatments, such as medication, rehabilitation or surgery, were required in 69.9% of the total. 5
Consequently, AE’s result in higher health care costs, due to directly related hospital admissions: more days of stay, tests and treatments that could have been avoided in almost half of the cases.
Among the most common complications linked to a hospital stay that we can find in patients with a venous catheter are phlebitis and bacteremia.
VASCULAR ACCESS-RELATED INFECTION
There are two types of infectious problems associated with vascular accesses:
- Local: catheter exit site infection or thrombophlebitis.
- General: bacteremia associated with the catheter and possible distant complications such as arthritis, endocarditis, etc.
IS IT POSSIBLE TO REDUCE CVC-RELATED INFECTION?
There are several factors that can increase the likelihood of encountering central venous catheter-related infection:
- Patient: immunodeficiency, renal replacement therapy, etc.4
- Catheter: prolonged dwell time, type of material and anatomical site of insertion. 4
- Healthcare practice: during catheter insertion and management. 4
In 2009, the Quality Agency of the Ministry of Health and Consumer Affairs (MSC), in collaboration with the World Health Organization (WHO) World Alliance for Patient Safety, launched the Bacteremia Zero project. 6
The Bacteremia Zero project is created with the primary goal of reducing the statewide average catheter-related bacteremia rate (CRB) to less than 4 episodes of bacteremia per 1,000 CVC days. 6
Thanks to this initiative, the CRB has been significantly reduced, but even after more than ten years it continues to be a major problem.
BACTERIEMIA ZERO
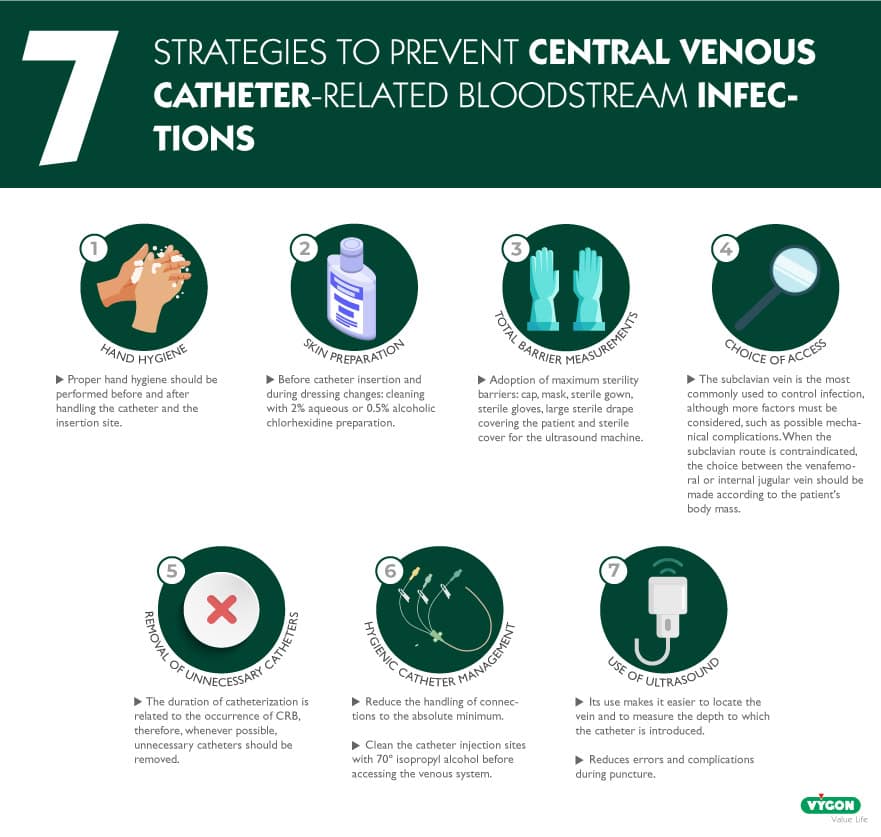
HAND HYGIENE
Proper hand hygiene should be performed before and after palpating catheter insertion sites. As well as before and after inserting, replacing, accessing, repairing or protecting an intravascular catheter. 6
This procedure shall be performed even when wearing gloves. 6
USE OF CHLORHEXIDINE FOR SKIN PREPARATION
Maximum precautions should be taken during catheter placement, and the skin should be disinfected with an appropriate antiseptic prior to catheter insertion and during dressing changes. 6
The most recommended solution is a 2% aqueous or 0.5% alcoholic chlorhexidine preparation.6
TOTAL BARRIER MEASURES DURING PLACEMENT OF CENTRAL VENOUS CATHETERS
The adoption of maximum sterility barriers (sterile cap, mask, sterile gown, sterile gloves, large sterile drape covering the patient and sterile ultrasound sheath) during CVC insertion significantly reduces Catheter-Related Bacteremia (CRB). 6
PLACE WHERE THE TRACK IS LAID
The point of insertion may influence a higher or lower risk of catheter-related infection due to differences in local skin flora density and risks of thrombophlebitis. 6
The subclavian vein is the most commonly used for infection control, although more factors such as possible mechanical complications, the risk of subclavian vein stenosis or the practitioner’s experience with the device must be considered. 6
When the subclavian route is contraindicated, the choice between the femoral or internal jugular vein should be made according to the patient’s body mass. Since, in patients with obesity, the infection rate is higher when the femoral vein is used than in the jugular vein. 6
Another aspect that must be taken into account is the risk of thrombophlebitis, since it is higher in the femoral route than in the subclavian or internal jugular veins. 6
REMOVAL OF UNNECESSARY CATHETERS
The duration of catheterization is related to the occurrence of CRB, therefore unnecessary catheters should be removed whenever possible. 6
HYGIENIC MANAGEMENT OF CATHETERS
Any intervention on the catheter involves a risk of infection. For this reason, it is also recommended to reduce the manipulation of connections to the essential minimum and to clean the catheter injection points with 70º isopropyl alcohol before accessing the venous system with them. 6
OTHER RECOMMENDATIONS
USE OF ULTRASOUND
Its use makes it easier to locate the vein and to measure the depth to which the catheter is introduced. For this reason, its use reduces errors and complications during puncture.
As we have seen, correct maintenance of the central line reduces infection and, consequently, increases patient safety, as well as reducing associated costs.
BIBLIOGRAPHY
- Cook, N. (1999). Central venous catheters: preventing infection and occlusion. British Journal of Nursing, 8(15), 980–989. https://doi.org/10.12968/bjon.1999.8.15.6524
- Rickard, C. M., & Ullman, A. J. (2018). Bloodstream infection and occlusion of central venous catheters in children. The Lancet Infectious Diseases, 18(8), 815–817. https://doi.org/10.1016/s1473-3099(18)30267-6
- A Protocol for the Prevention of Central Line Occlusion and Central Line-Associated Bloodstream Infection in Home Health Felicia C. Holston. Universidad de Carolina del Este
- Pitiriga, V., Kanellopoulos, P., Bakalis, I., Kampos, E., Sagris, I., Saroglou, G., & Tsakris, A. (2020). Central venous catheter-related bloodstream infection and colonization: the impact of insertion site and distribution of multidrug-resistant pathogens. Antimicrobial Resistance & Infection Control, 9(1). https://doi.org/10.1186/s13756-020-00851-1
- Estudio Nacional sobre los Efectos Adversos ligados a la Hospitalización. ENEAS 2005. Plan de Calidad para el Sistema Nacional de Salud. Ministerio de sanidad y consumo de España. https://seguridaddelpaciente.es/resources/contenidos/castellano/2006/ENEAS.pdf
- Bacteriemia Zero. Protocolo prevención de las bacteriemias relacionadas con catéteres venosos centrales (brc) en las uci españolas (2015). Plan de Calidad para el Sistema Nacional de Salud. Ministerio de sanidad y consumo de España. https://seguridaddelpaciente.es/resources/documentos/2015/PROTOCOLO_BACTERIEMIA_ZERO.pdf