Neonatal tracheal intubation is a frequently performed but high-risk procedure for the baby in delivery rooms (DR) or in neonatal intensive care units (NICU)1. Despite its common use, it remains a complex procedure, particularly when faced with an unexpectedly difficult airway in neonates and infants. Due to the unique physiological characteristics of these patients, neonatologists, anesthesiologists, and critical care clinicians must respond swiftly to secure the airway2.
Difficult intubation in neonates, the need to minimize intubation attempts
Tracheal intubation in neonates is associated with risks such as bradycardia, hypoxia, and airway trauma1. A difficult intubation occurs when an endotracheal tube (ETT) cannot be successfully placed with 3 (or fewer) attempts to establish ventilation1,2. Each failed intubation attempt increases the risk of severe oxygen desaturation and related complications, further compromising a difficult airway management3.
Premature neonates are particularly susceptible to difficult intubation1. The rate of three or more intubation attempts remains high, reaching 65% in some delivery room settings. In one study, 17% of neonates were not intubated successfully despite multiple attempts, while 48% required three or more attempts for successful intubation. A multicenter NICU intubation registry reported that 14% of patients required at least three intubation attempts1.
Strategies should be implemented to limit the number of intubations attempts while ensuring effective airway management.
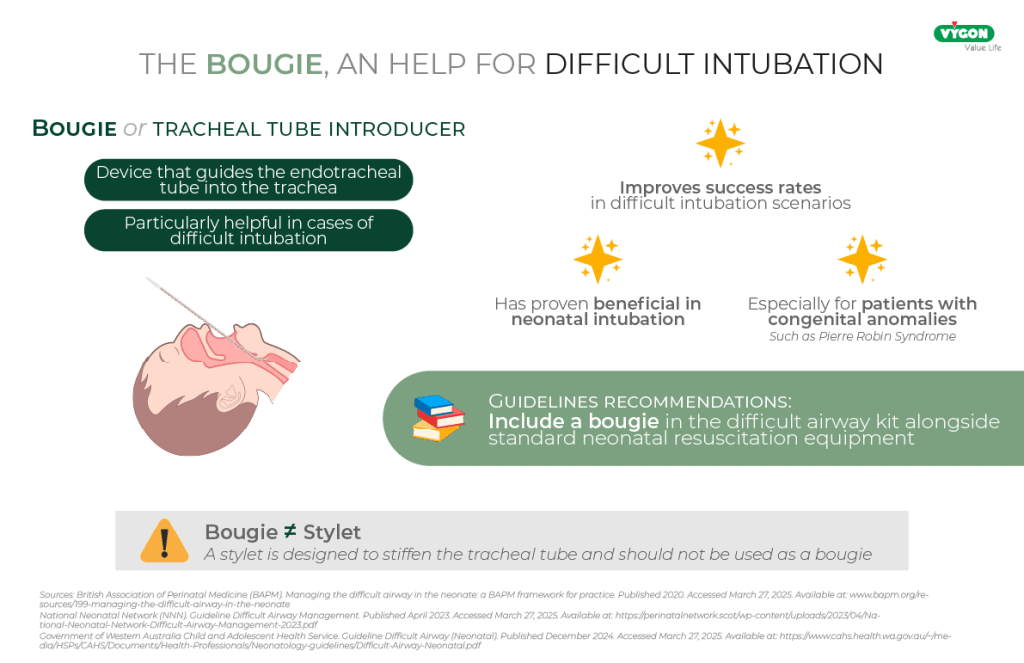
Bougie’s use can help in difficult Intubation
A bougie, or tracheal tube introducer, is a simple yet effective device that helps guide the ETT into the trachea, particularly in cases of difficult intubation. It has proven beneficial in neonatal intubation, especially for patients with congenital anomalies such as Pierre Robin Syndrome1.
However, while bougies can improve success rates, their use in neonates remains controversial due to reports of complications such as pneumothorax and bronchial trauma1. Nevertheless, it is essential to distinguish between a bougie and a stylet. A stylet is designed to stiffen the tracheal tube and should not be used as a bougie, as improper use has been associated with tracheal perforation4.
According to a literature review, combining bougie use with videolaryngoscopy can enhance success rates in difficult intubation scenarios1. Recognizing its value, several guidelines, including those from the British Association of Perinatal Medicine4, the National Neonatal Network Guideline for Difficult Airway Management (Scottish Neonatal Network, NHS)3, and the Government of Western Australia Child and Adolescent Health Service5, recommend including a bougie in the difficult airway kit alongside standard neonatal resuscitation equipment.
Managing desaturation during intubation
Neonates are particularly prone to oxygen desaturation due to their limited functional residual lung capacity and high metabolic demand2. A study from the Pediatric Difficult Intubation Registry (PeDI-R) found that hypoxemia occurred in 9% of difficult intubations. Similarly, the National Emergency Airway Registry for Children (NEAR4KIDS) reported a desaturation rate of 13% for all intubations and nearly 50% for difficult intubations. The National Emergency Airway Registry for Neonates (NEAR4NEOS) reported an even higher incidence of hypoxia, occurring in 42% of non-difficult intubations and 75% of difficult intubations6.
Hypoxia during intubation can lead to severe complications like bradycardia7 or cardiac arrest8. The primary objective is to maintain adequate oxygenation until a definitive airway is secured3.
Certain bougies enable oxygen insufflation during intubation, helping to prevent hypoxia. However, while this technique may reduce desaturation risks, caution is necessary to avoid pulmonary hyperinflation, particularly in cases of laryngospasm.
The risk of laryngospasm
Laryngospasm is a protective reflex that prevents foreign substances from entering the lower airways. It results in a sudden closure of the vocal cords, it can result in a partial or complete airway obstructionwhich can lead to hypoxia9. This reflex can be triggered during airway manipulation, such as laryngoscopy or intubation attempts. If not promptly addressed, laryngospasm may cause severe complications, including pulmonary edema or even fatal outcomes10.
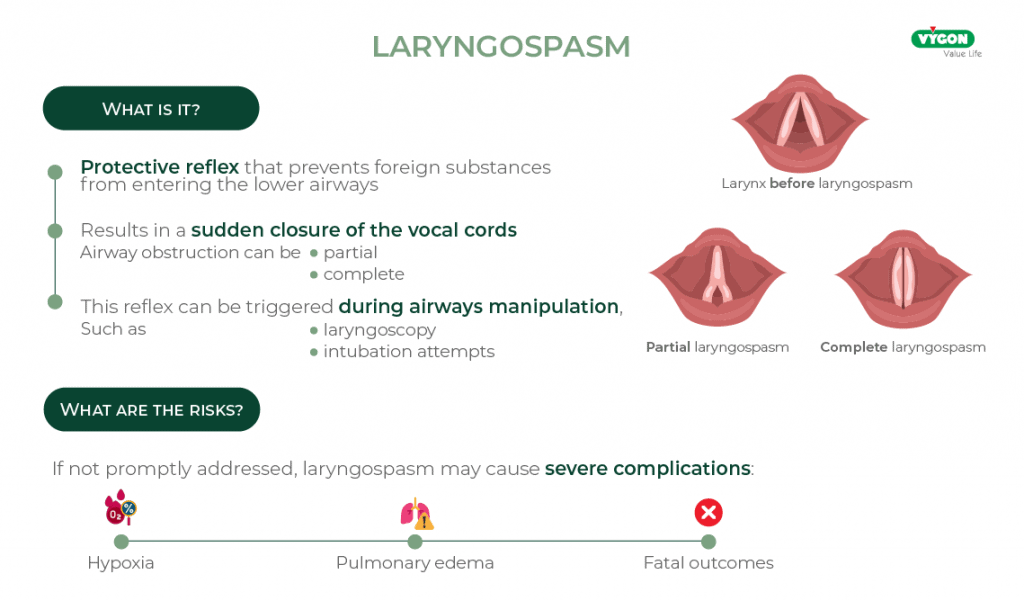
While oxygenation during intubation is essential, excessive airway pressure in the presence of laryngospasm can cause a barotrauma. Proper airway management must strike a balance between ensuring adequate oxygenation and minimizing the risk of barotrauma in the event of spasm. That’s why, an optimal bougie should incorporate decompression openings that allow excess oxygen to escape via the main tube of the bougie, thereby preventing excessive airway pressure buildup in cases of laryngospasm.
Conclusion
Difficult neonatal intubation remains a significant clinical challenge, often requiring multiple attempts that increase the risk of complications. Bougies are a useful device for improving intubation success rates. By also allowing oxygenation and decompression (through openings), in case of laryngospasm to prevent the risk of barotrauma, the use of a bougie can help improve safety during neonatal intubation.
Bibliography
- Berisha G, Boldingh AM, Blakstad EW, Rønnestad AE and Solevåg AL (2021) Management of the Unexpected Difficult Airway in Neonatal Resuscitation.Front. Pediatr. 9:699159. doi: 10.3389/fped.2021.699159
- Sawa T, Kainuma A, Akiyama K, Kinoshita M and Shibasaki M (2021) Difficult Airway Management in Neonates and Infants: Knowledge of Devices and a Device-Oriented Strategy. Front. Pediatr. 9:654291. doi: 10.3389/fped.2021.654291
- National-Neonatal-Network (NNN). Guideline Difficult Airway Management. April 2023. Online at: https://perinatalnetwork.scot/wp-content/uploads/2023/04/National-Neonatal-Network-Difficult-Airway-Management-2023.pdf
- British Association of perinatal medicine (BAPM). Managing the difficult airway in the neonate: a BAPM framework for practice. 2020. Online at: www.bapm.org/resources/199- managing-the-difficult-airway-in-the-neonate
- Government of Western Australia Child and Adolescent Health Service. Guideline Difficult Airway (Neonatal). December 2024. Online at: https://www.cahs.health.wa.gov.au/~/media/HSPs/CAHS/Documents/Health-Professionals/Neonatology-guidelines/Difficult-Airway-Neonatal.pdf
- Else, Scott D. N. MD*; Kovatsis, Pete G. MD†. A Narrative Review of Oxygenation During Pediatric Intubation and Airway Procedures. Anesthesia & Analgesia 130(4):p 831-840, April 2020. | DOI: 10.1213/ANE.0000000000004403
- Manley BJ, Hodgson KA. Addressing the subpar success rates of infant intubation. Lancet Child Adolesc Health. 2023 Feb;7(2):80-81. doi: 10.1016/S2352-4642(22)00317-0. Epub 2022 Nov 24. PMID: 36436540.
- McKown AC, Casey JD, Russell DW, Joffe AM, Janz DR, Rice TW, Semler MW. Risk Factors for and Prediction of Hypoxemia during Tracheal Intubation of Critically Ill Adults. Ann Am Thorac Soc. 2018 Nov;15(11):1320-1327. doi: 10.1513/AnnalsATS.201802-118OC. PMID: 30109943; PMCID: PMC6322012.
- D. Guillou, G. Orliaguet. Laryngospasme en pédiatrie. SFAR. 51e Congrès national d’anesthésie et de réanimation. 2009. https://sofia.medicalistes.fr/spip/IMG/pdf/laryngospasme_en_pediatrie.pdf
- Ghofaily LA, Simmons C, Chen L, Liu R. Negative Pressure Pulmonary Edema after Laryngospasm: A Revisit with a Case Report. J Anesth Clin Res. 2013 Oct 28;3(10):252. doi: 10.4172/2155-6148.1000252 . PMID: 24524005 ; PMCID: PMC3919040.






