The first definition of sepsis was made in 1980 and was based on the concept of Systemic Inflammatory Response (SIRS). Despite advances and new definitions over the years, it was then that the basis for the management of the septic patient was established.
Sepsis is one of the most serious diseases with the highest mortality rates in existence, and although the triggering element is usually bacteria (in 85% of cases), parasites, fungi or a virus such as Ebola or coronavirus can also trigger this terrible pathology. 1
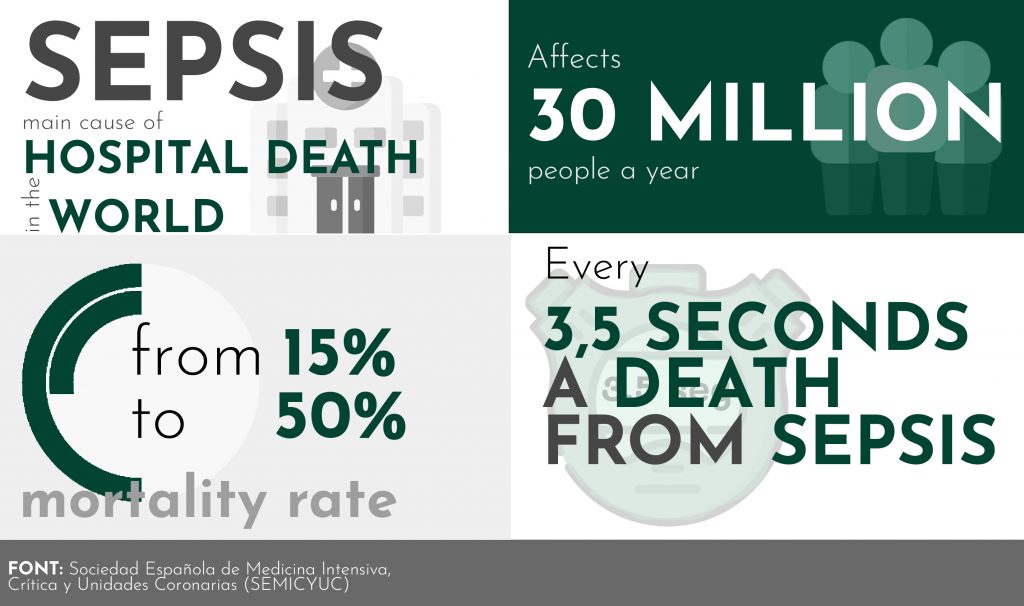
Many professionals are now talking about the need for a sepsis code to improve recovery rates for these patients, as currently only about 150 out of 700 hospitals have such a code1.
Multicentre studies have shown a decrease in mortality of more than 25% in departments where these measures have been implemented. 2
In this article we will explore one of the important points to take into account in this disease: the parameters that suffer alterations during treatment.
Therapeutic objetcives

Treatment of septic shock requires an in-depth analysis of the patient’s condition. In such severe cases, goal-directed therapy is advised, where the patient’s response to treatment is measured at all times.
A mandatory first step in the initial assessment of the critically ill patient is to determine the state of tissue perfusion.
Cellular oxygenation problems can lead to the development of organ damage, multi-organ failure and, ultimately, death of the patient.
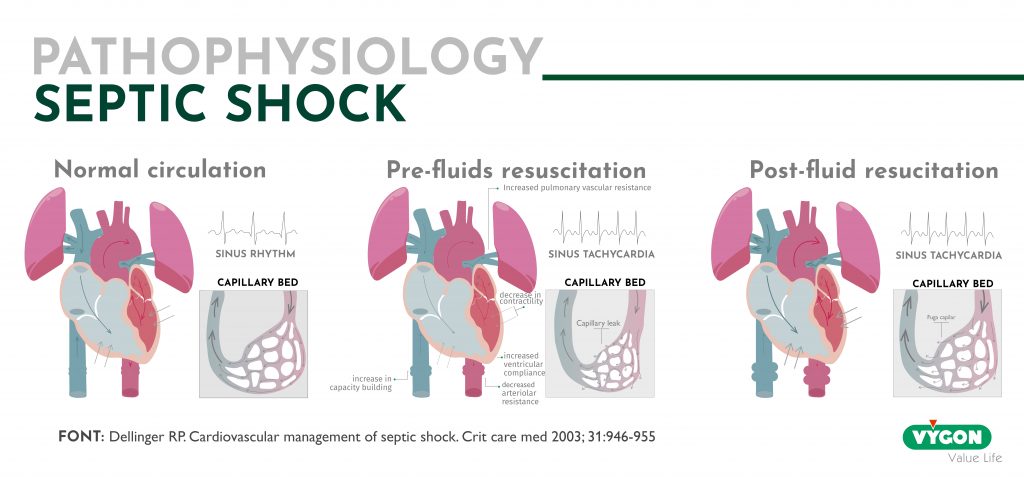
What we commonly refer to as hemodynamic instability generally refers to the presence of clinical signs suggestive of hypoperfusion (sensory disturbances, poor capillary filling, etc.), and especially arterial hypotension.
Failure to maintain adequate tissue perfusion results in increased peripheral oxygen extraction and less efficient anaerobic pathways are involved in order to maintain cellular respiration.
In fact, when we speak of shock or cardiovascular failure, it is because there is evidence of tissue hypoperfusion and/or increased lactic acid, beyond arterial hypotension.
Hemodynamic parameters
The goal in shock patients should be to restore the balance between oxygen transport (DO 2) and consumption (VO 2) by tissues, with subsequent reversal of anaerobiosis.
Failure to achieve this adjustment early is associated with serious consequences and poor prognosis.
Arterial pressure
Mean arterial pressure (MAP) is an indicator of tissue perfusion pressure.
Physiologically, the vascular system loses its ability to self-regulate at MAP values below 60-65mmHg.
Therefore, the target value to aim for is 65mmHg or higher.
Tissue perfusion
As mentioned above, adequate tissue perfusion is vital. Therefore, it is very important to know how much oxygen the organism is receiving.
There are some indirect indicators such as hourly diuresis, capillary refill, skin temperature, the existence of lividity or the patient’s mental state that can provide an approximation.
However, values such as central venous saturation, mixed venous saturation or lactate are used to determine tissue perfusion more accurately.
Venous saturation
A decrease in cardiac output or an increase in metabolic needs leads to a compensatory increase in oxygen extraction, with a consequent decrease in venous saturations.
Mixed venous saturation or central venous saturation are two values that provide information about tissue perfusion.
Mixed venous oxygen saturation is measured in the blood through a pulmonary artery catheter and its value provides information about systemic oxygen consumption.
Mixed venous saturation values are not the same as central venous saturation, which represents the oxygen saturation measured in the blood through the superior vena cava at the entrance to the right atrium.
Although they are different values, as they are not measured in the same location, they both provide the practitioner with information that serves the same purpose: to know how much oxygen is reaching the cells.
During the first 6 hours of septic shock, the values to be sought are: ScO2 ≥65% or a ScvO2 ≥70%.
Lactic acid
An increase in lactic acid, in addition to providing information on cellular hypoxia and anaerobic metabolism, may also be related to hypermetabolism, pyruvate dehydrogenase deficiency and decreased hepatic clearance. All of these may be present in septic shock.
Lactate/pyruvic ratio greater than 15 is more appropriate than lactic acid alone to differentiate hyperlactacidemia due to hypoxia from increased aerobic glycolysis in situations of high metabolic stress, as is the case in these patients.
Oxygen transport
Not observing a global perfusion mismatch does not mean that there are no regional alterations (regional dysoxia), so it is important to know and adapt the OD2 to prevent organ dysfunction.
The reason why splanchnic perfusion has been the target of regional O2 monitoring is because the intestinal mucosa has a high vascularity characteristic associated with it. It is very sensitive to hemodynamic instability and prone to imbalance between O2 supply and demand.
On the other hand, its high metabolic activity, the important immunological activity and its ‘barrier’ function have an impact on multi-organ failure.
In patients at high surgical risk, the following levels are recommended as a target for hemodynamic optimisation before, during and after surgery: OD 2 > 600mlO 2 / min / m 2.
Sublingual capnography
Recent studies have shown that a decrease in blood flow at the sublingual level is proportional to that perceived in the mesenteric territory in shock. Sublingual PCO2 (PSLCO2) is related to gastric mucosal PCO2.
Mainly the difference between measured sublingual PCO2 and arterial PCO2 (PSLCO2-PaCO2) has been considered a good prognostic indicator.
Cardiac output
Cardiac output (CO) is considered a marker or assessor of global cardiac function.
It is also one of the most widely used parameters as it provides information on the cause of shock and organ failure.
However, cardiac output must be integrated with other hemodynamic variables (preload, contractility and afterload measurements), biological signs and tissue oxygenation parameters. The complexity and heterogeneity of septic shock patients implies individualised approaches to hemodynamic management. Therefore, in-depth knowledge of the most relevant variables in the course of this disease will provide the professional with the necessary tools to start treatment as early as possible.
Bibliography
- Laura Tardón. La sepsis causa la mayoría de las muertes por coronavirus. Diario El Mundo. 24 de marzo de 2020
- Dr. M. Borges Sá. Dr. F.J. Candel González. Dr. R. Ferrer Roca. Dr. P. Vidal Cortés. Dr. R. Zaragoza Crespo. Código Sepsis. IMC. ISBN: 978-84-7867-282-0
- F. Valenzuela Sánchez, R. Bohollo de Austria, I. Monge García, A. Gil Cano. Shock séptico. Revista de Medicina Intensiva. Vol. 29. Núm. 3. páginas 192-200. Abril 2005.






