The importance of good blood pressure waveform morphology
In our daily practice in anesthesia and intensive care, we continuously use monitors that reproduce the blood pressure waveform and measure its values, reporting systolic, diastolic, and mean blood pressure data to the clinician. However, in 1 out of 3 patients the morphology reproduced by the pressure transducer and monitor is incorrect, resulting in inaccurate diagnoses and potential therapeutic errors.
Therapeutic error is one of the major risks in clinical practice and understanding the correct morphology of the arterial pressure waveform and the artifacts that can affect it is the first step to avoid it.
This article summarizes Prof. Stefano Romagnoli’s lecture at VYHEMDAYS 2025, which makes us remember the importance of good blood pressure readings and the magnitude of the problem. He also shares practical and clear solutions on what we can do to diagnose distortion of the waveform and improve its representation and analysis.
If you don’t have time, we summarize the article for you in 1 minute
Many professionals rely on the readings from their monitors without verifying the quality of the visualized blood pressure waveform. However, about 30% of waves contain artifacts, leading to misdiagnosis and, in many cases, incorrect treatment of the patient. Selecting a suitable arterial catheter, using a damping device or using an electronic filter are three measures that can be taken to obtain a good waveform.
BLOOD PRESSURE = CARDIAC OUTPUT?
Although it is common in clinical practice to use blood pressure (especially mean arterial pressure) as a surrogate for cardiac output, we must be clear that these parameters do not necessarily have a clinically significant correlation, since flow and pressure are NOT the same thing. Systemic vascular resistances (or vascular tone, or vascular impedance) play a key role in the relationship between pressure and flow, modifying the interaction between them.
We always refer to direct, continuous blood pressure measurement with an arterial catheter as the gold standard for high-risk surgical patients. However, even this method is prone to artifacts… Why?
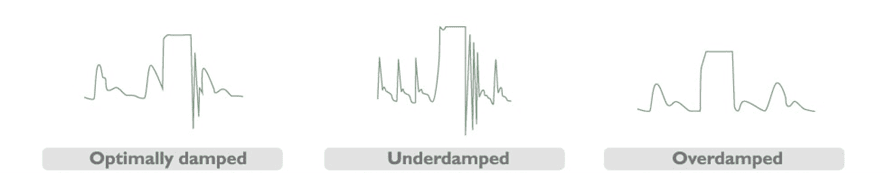
There may be an inadequate dynamic response in the catheter-tubing-transducer system, whereby the visualized signal is significantly influenced, thus giving rise to the well-known phenomena of over-damping and under-damping (or resonance).
About 30% of our arterial pressure waves, detected in the operating room or intensive care unit, show underdamping artifacts (resonance)
On this occasion, I would like to focus on resonance, as it is more difficult to identify than overdamping. We must bear in mind a striking figure:
Waveform resonance artifacts affect about 30% of our patients during surgery or in the intensive care.
This means that about 3 out of 10 patients could be subject to erroneous diagnoses and therapeutic decisions.
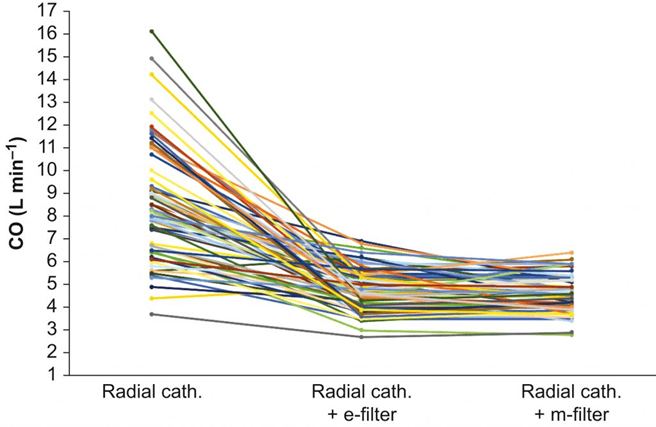
We know that the physiology of the blood pressure waveform is very complex and derives from the dynamic interaction of systolic volume, arterial compliance, flow resistance, vascular stiffness… there is a great deal of information in each heartbeat. Therefore, artifacts imply erroneous data in the different parameters we observe on the monitor. In a 2022 study1, we referred to the overestimation of systolic overshoot that commonly occurs in cases of resonance and often leads to an overestimation of cardiac output when a flow calculation (estimation) algorithm (called pulse wave or pulse contour analysis) is applied to the waveform:
“By comparing resonant waves with and without the application of an innovative dynamic electronic filter (specifically designed to identify and correct resonating arterial signal), we observed that the analyzed wave had a 91% overestimation of cardiac output.”
An overestimation of systolic blood pressure and/or cardiac output can lead to misdiagnosis, which, in turn, can lead to under- or over-treatment of the patient and, ultimately, to harm to the patient and possibly a loss of confidence on the part of the doctor in the monitoring system he or she relies on.
REAL CASE IN THE OPERATING THEATRE: WHEN THE WAVE LIES
I want you to join me in a real case and to imagine that you are with me in the operating theatre.
- This is a 15-year-old low-risk patient who was undergoing high-risk liver surgery. Initially, hemodynamic parameters were stable.
- Following a hemorrhage of approximately 2,000 ml, she developed tachycardia associated with an unexpected increase in systolic blood pressure (from 91 to 136 mmHg), cardiac output (from 4 to 11 l/min), max dP/dt (from 0.66 to 1.55 mmHg/ms), CCE (from 0.38 to 0.50) and a reduction in arterial elastance (from 0.93 to 0.83 mmHg/ml).
- These values, especially the increase in cardiac output during bleeding, are physiologically implausible.
- Activation of the autonomic nervous system alone could NOT justify a change in systemic hemodynamics in this direction.
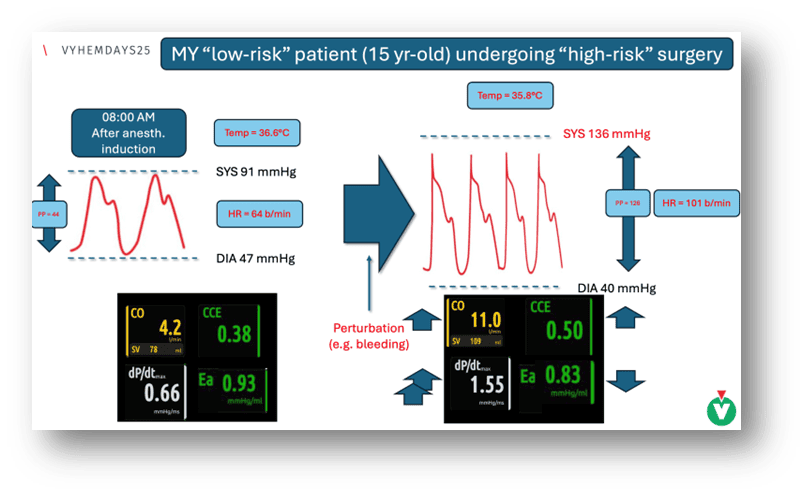
- A resonance artifact in the waveform was suspected and confirmed.
- After correcting the signal, the numbers obtained were, although ‘worse’ (more pathologic), more consistent: a significant decrease in cardiac output, an increase in PPV (pulse pressure variation), a decrease in blood pressure, an increase in arterial elastance, and a decrease in CCE.
This case illustrates how an artifactual waveform can mask a low-flow condition2. Incorrect information will lead us to perform incorrect treatments and make wrong decisions.
HOW TO DETECT ARTIFACTS IN THE BLOOD PRESSURE WAVEFORM?
There are several ways to suspect a resonance or over-damping artifact:
- Analyze the morphology of the blood pressure waveform.
- Measure the difference between non-invasive (in this case more reliable) and invasive blood pressure (NIBP-IBP).
- dP/dtmax: A value greater than 1.67 mmHg/msec may indicate the presence of a resonance artifacts3.
ARTIFACTS DO NOT BIRTH ON THE MONITOR; THEY ARE REFLECTED ON IT
Artifacts are not a problem exclusive to one brand of monitor but rather result from distortion generated by the entire signal transduction system (transducer, extension tube, catheter, artery, etc ), they affect ALL monitors that measure blood pressure and even more those monitors that use the pulse contour to estimate stroke volume and cardiac output.
Artifacts are not a problem exclusive to one brand of monitor, but rather, as they are caused by distortion generated by the full system of signal transduction (transducer, extension line, catheter, artery, …), they affect all monitors that measure blood pressure and even more those that use the pulse contour to estimate cardiac output and stroke volume.
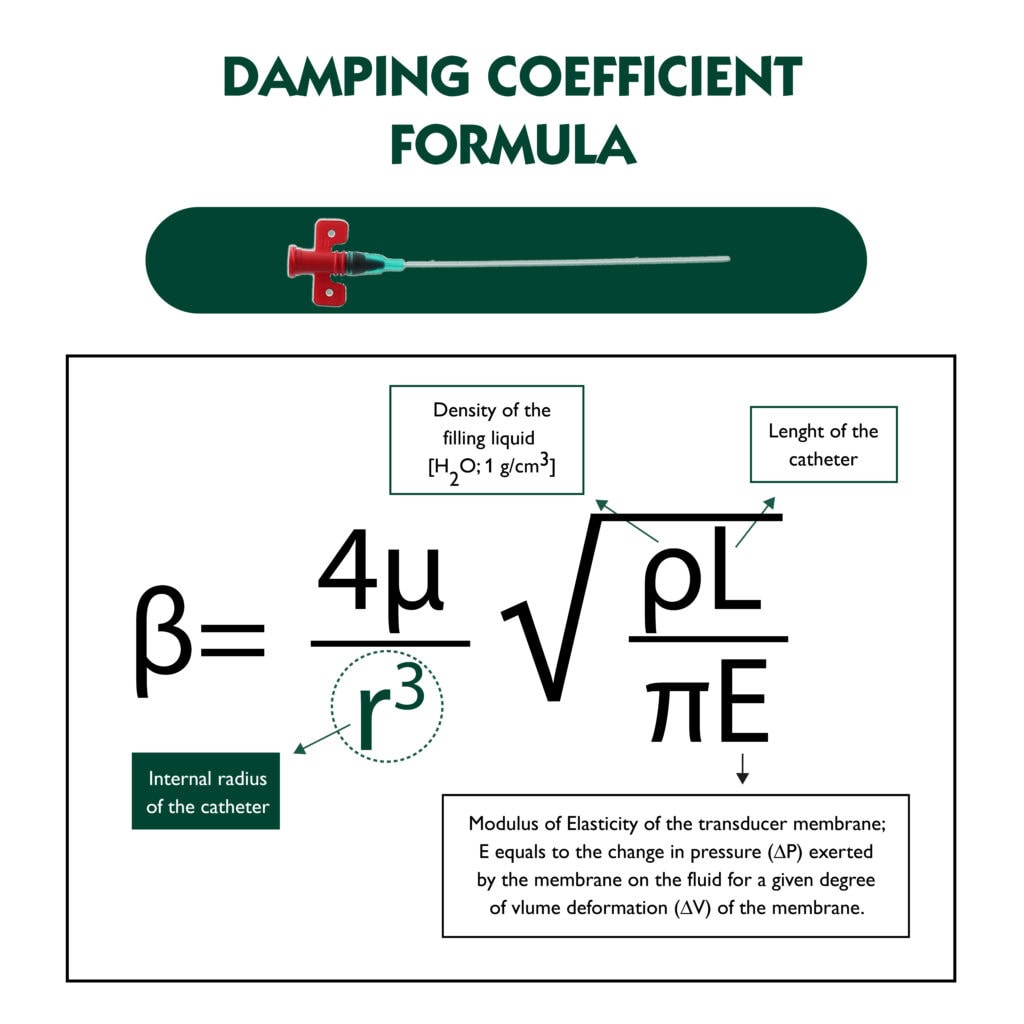
Therefore, the quality of the blood pressure waveform transmission is crucial. The dynamic response of the system depends on multiple factors, including the length and inner radius of the catheter. We already know that larger diameter catheters (e.g., 18 G) are much more likely to generate resonance than smaller ones (e.g., 20 G).
This characteristic comes from the damping coefficient formula where the radius of the catheter is located at the denominator and elevated at the third power.
Having the right signal is the first step to avoid major mistakes in our diagnostic and therapeutic decisions.
HOW CAN WE AVOID ARTIFACTS?
Selecting the right catheter and verifying the dynamic response of the transducer system are two key factors in obtaining a correct waveform. Getting a good signal is the first step; we must ensure that there are no problems with the pressure transducer before looking at what the monitor is telling us (i.e. blood pressure values).
In addition, there are mechanical filters that can be added inside the arterial pressure line or cardiac output monitors that have electronic filters that allow the waveform to be corrected automatically, eliminating resonance distortion and providing more reliable blood pressure and cardiac output estimates.
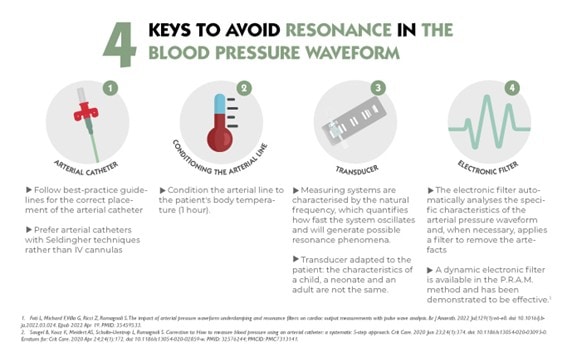
Summarized in a practical way, we must remember these 4 factors:
- Properly verify the dynamic response of the catheter-tubing-transducer system. (fast-flush test)
- Use smaller caliber catheters if possible (20G better than 18 G)
- Use an adjustable damping device when necessary.
- Use an electronic filter. Activating the filter allows artifacts to be corrected and has proven to be very effective, contributing to better decision-making.
Being aware of the problem is the first step towards correcting it
Although scientific literature on pressure wave devices dates to 1949, with key publications in the 1980s and a renew in the last decade, awareness of the problem remains insufficient among healthcare professionals.4
In summary, if a patient requires continuous invasive blood pressure monitoring, it is essential that this information is accurate. Cardiac output monitors are important tools, but therapeutic interventions are those that save lives, and these are based on the data we read. We cannot properly work with waveforms affected by artifacts.
The key lies in the reliability of the number provided by the monitor. This reliability can only be achieved if the device analyses a correct waveform.
Although not all monitors have automatic filters, it is vital that clinicians know how to identify the problem and correct it, to ensure that therapeutic decisions are based on accurate data, thus avoiding therapeutic errors.
“We cannot continue working with incorrect blood pressure readings. We can identify the problem and must correct it.”
Prof. Stefano Romagnoli
REFERENCES
- Foti L, Michard F, Villa G, Ricci Z, Romagnoli S. The impact of arterial pressure waveform underdamping and resonance filters on cardiac output measurements with pulse wave analysis. Br J Anaesth. 2022 Jul;129(1):e6-e8. doi: 10.1016/j.bja.2022.03.024. Epub 2022 Apr 19. PMID: 35459533.
- Michard F. Towards the automatic detection and correction of abnormal arterial pressure waveforms. J Clin Monit Comput 38, 749–752 (2024). https://doi.org/10.1007/s10877-024-01152-3
- Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, Romano SM, De Gaudio AR. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Crit Care. 2014 Nov 30;18(6):644. doi: 10.1186/s13054-014-0644-4. PMID: 25433536; PMCID: PMC4279904.
- Gardner RM. Direct blood pressure measurement–dynamic response requirements. Anesthesiology. 1981 Mar;54(3):227-36. doi: 10.1097/00000542-198103000-00010. PMID: 7469106.
If you want to learn how to improve your artery monitoring technique, get the most out of your monitor’s information, or learn more about the electronic filter, don’t miss these resources:






