When withdrawing a Huber needle from an implantable port, complications such as occlusion can arise. It is one of the leading complications in CVADs, affecting up to 1 in 3 catheters1 and can potentially lead to serious or life-threatening consequences.
To mitigate these risks, several techniques are employed. Among them, the positive pressure technique plays a central role. This method is essential during Huber needle withdrawal to maintain catheter patency and prevent blood reflux, ensuring safe port access without causing damage.
This article offers an in-depth examination of the positive pressure technique, its clinical relevance, and the best practices for its effective application.
What is catheter occlusion?
According to Moureau1, catheter occlusion is defined as a partial or complete blockage of a vascular access device (VAD) that limits or prevents blood aspiration, withdrawal, flushing of the catheter, administration of blood, and infusion of solutions, medications, or drugs.
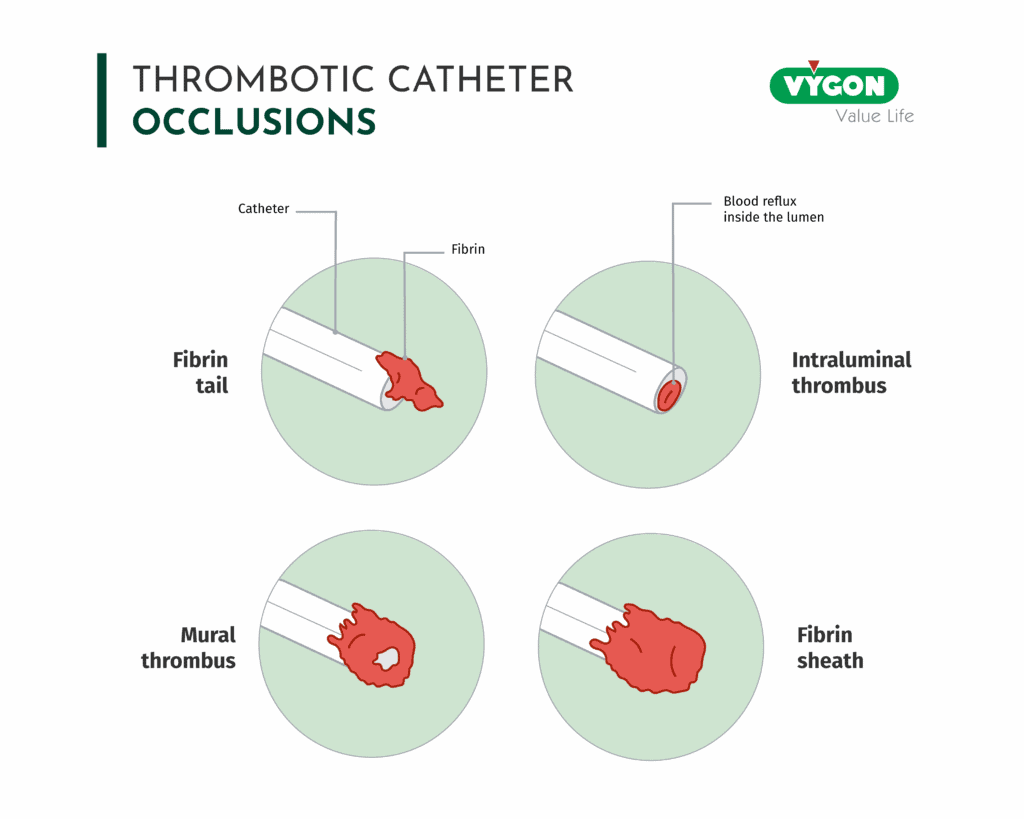
Occlusion can be classified as follows:5
- Fibrin tail: A strand of fibrine adheres to the catheter tip and extends into the bloodstream
- Intraluminal thrombus: A blood clot forms inside the catheter lumen, often leading to complete obstruction
- Mural thrombus: Fibrin from vessel wall injury binds to fibrin on the catheter, forming a clot attached to both
- Fibrin sheath: Fibrin coats the external surface of the catheter, forming a “sock” around it
Blood reflux, one of the main causes of catheter occlusion
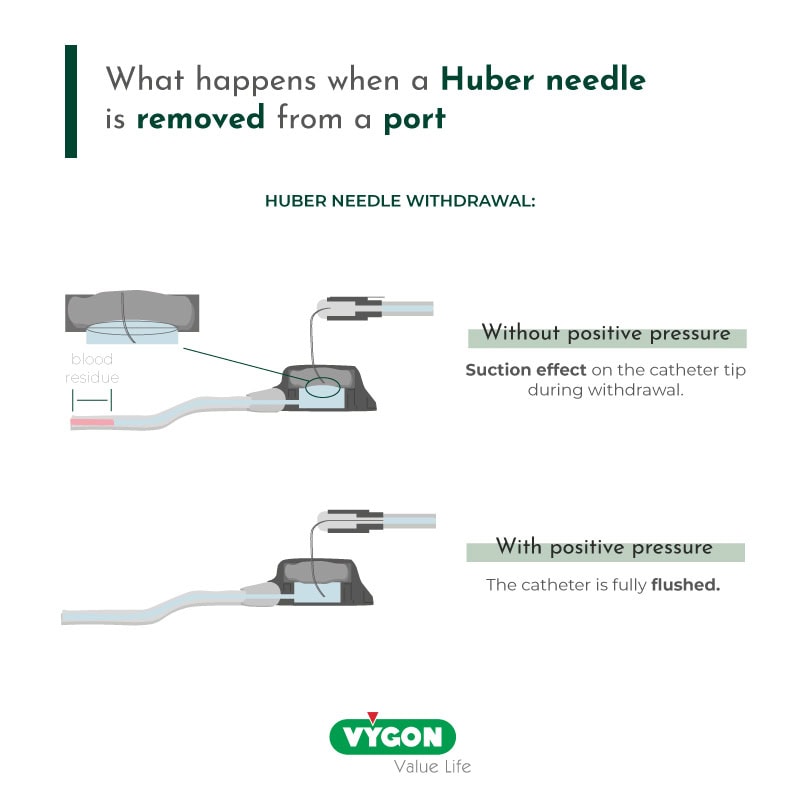
Occlusion during needle withdrawal is primarily caused by blood reflux.
In 99% of cases, a suction effect is created during the removal of the needle, due to the adhesion between the steel of the needle and the silicone of the septum2. This mechanism leads to blood reflux at the distal end of the catheter, which can result in obstruction.
The use of positive pressure to prevent catheter occlusion
When referring to catheter occlusion, the traditional “negative pressure” technique (flush – clamp – withdraw) has proven itself insufficient to prevent blood deposit.
Therefore, international guidelines recommend other techniques to prevent catheter occlusion during withdrawal, with positive pressure being the most effective one. This method involves injecting fluid into the implantable port while simultaneously withdrawing the Huber needle.
By maintaining forward flow during needle removal, positive pressure counteracts the negative pressure that would otherwise draw blood into the catheter. In a study by Kelly et al.4,it was confirmed that one-handed positive pressure needle withdrawal was more effective than positive pressure flushing alone in minimizing reflux.
Another study by Lapalu3 has proven that without the application of positive pressure, nearly all cases (99.1%) showed blood reflux into the catheter. In parallel, the application of positive pressure during Huber needle withdrawal reduced the incidence of reflux by nearly 80%, going from 99% to 22%.
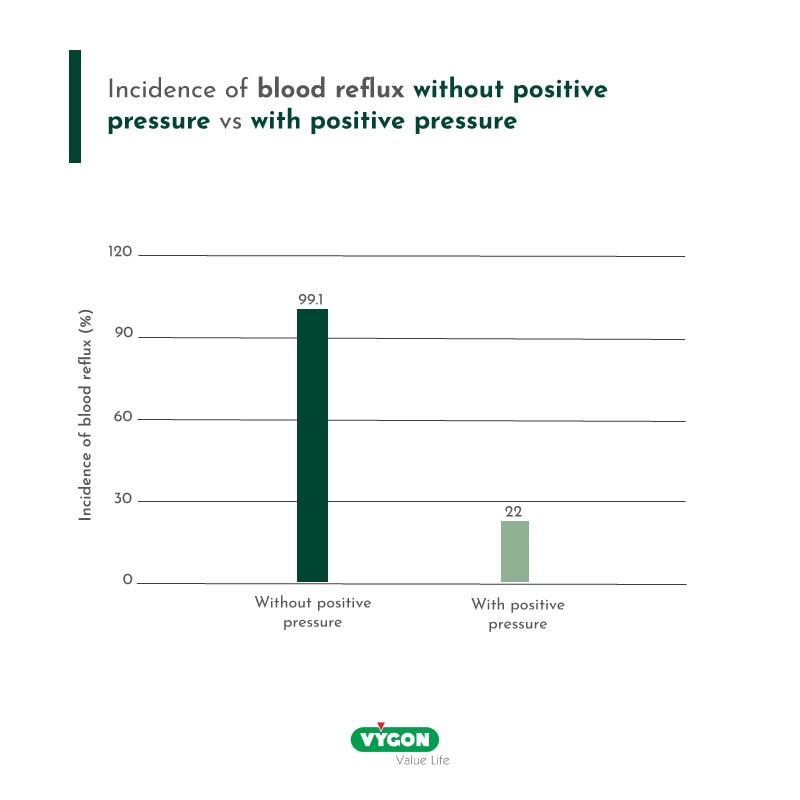
Compared to turbulent flushing and negative pressure, this positive pressure proved indeed significantly more effective in minimizing reflux. It is however important not to confuse it with the pulsatile flush, that involves a push – pause flush designed to clear the catheter and port of biofilm.
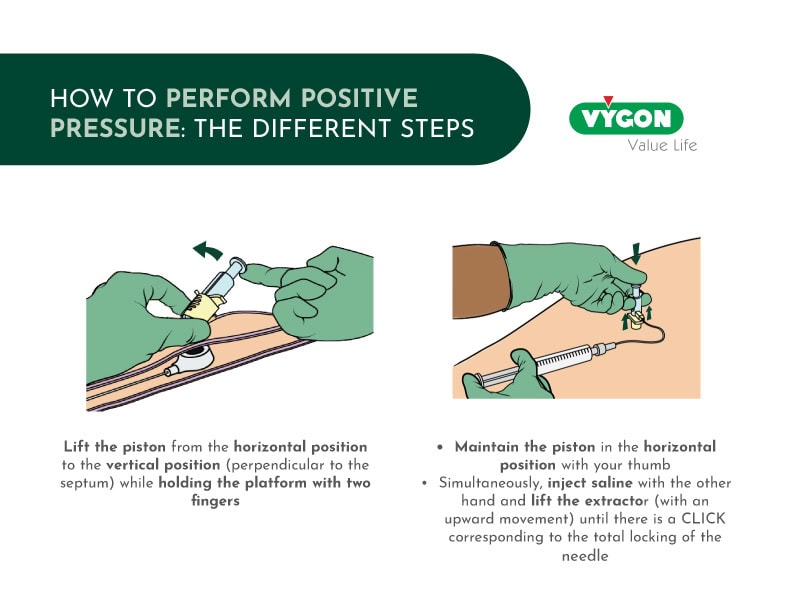
How to perform positive pressure: the different steps
Which type of Huber needle is the most adapted for positive pressure?
Several types of Huber needles are available today. Each has different mechanisms to reduce blood reflux and the risk of catheter occlusion during withdrawal. These devices can be grouped into two main categories6:
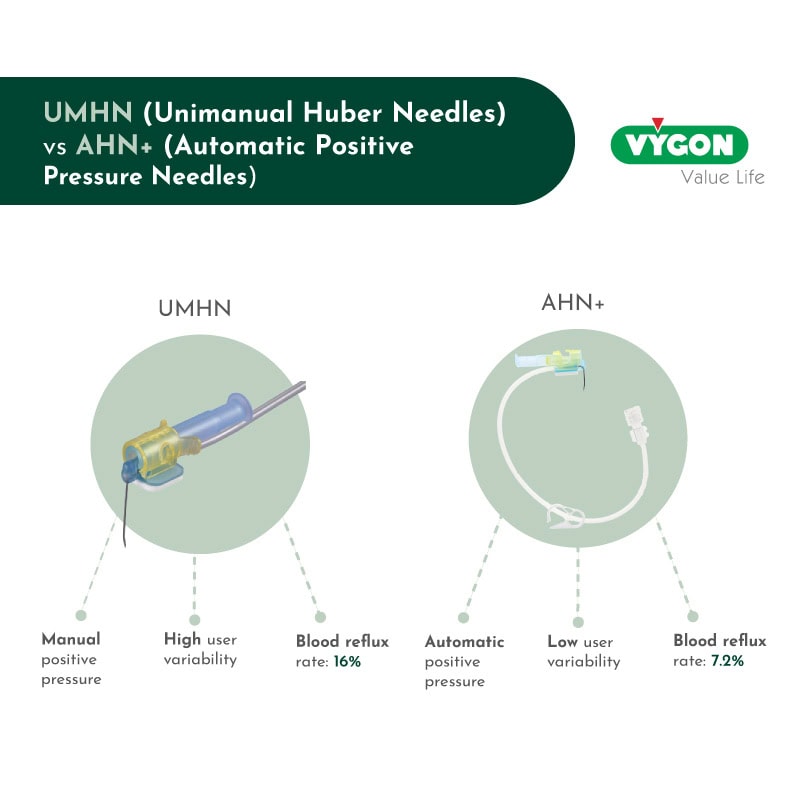
- Unimanual Huber Needles (UMHN):
UMHN requires manual positive pressure during withdrawal. It includes a safety mechanism which protects the nurse from accidental needlestick injuries. These safety needles offer improved ergonomics and smoother handling but still rely on the user’s technique.
Despite the improved design, the residual reflux rate remains high (16%) when pressure is applied manually.
- Automatic Positive Pressure Huber Needles (AHN+)
The latest generation of needles, such as AHN+, feature an integrated automatic positive pressure mechanism. During withdrawal, a connecting line is compressed against the plunger, automatically injecting saline into the port.
This system allows safe, one-handed withdrawal for the clinician and effective prevention of blood reflux for the patient. It eliminates user variability, ensuring consistent performance regardless of who uses it.
The results show a significantly lower residual reflux rate with this type of needles (7.2%).
Occlusion is a common complication during Huber needle withdrawal, but it can be effectively prevented with the right tools and techniques.
Positive pressure has proven to be an effective solution and is supported by international guidelines. When paired with an automatic positive pressure Huber needle, this method significantly reduces blood reflux and helps minimize the risk of catheter occlusion.
Bibliography:
- Moureau, N., Gorski, L., Flynn, J., & Johnson, K. (2025). A systematic review of needleless connector function and occlusion outcomes: Evidence leading the way. Journal of Infusion Nursing, 48(2), 84–105. https://doi.org/10.1097/NAN.0000000000000578
- Dupont, C. (Ed.). (2012). Guide pratique des chambres à cathéter implantables: Utilisation et gestion des complications (1st ed., pp. 202–203). Lamarre.
- Lapalu, J., Losser, M.-R., Albert, O., Levert, A., Villiers, S., Faure, P., & Douard, M.-C. (2010). Totally implantable port management: Impact of positive pressure during needle withdrawal on catheter tip occlusion (an experimental study). Journal of Vascular Access, 11(1), 46–51. https://doi.org/10.1177/112972981001100110 [europepmc.org]
- Linda J. Kelly, Constance Girgenti, Tracy Jones (2024). Observational Experiment of Catheter Reflux During Huber Needle Withdrawal. WoCoVA.
- 5. Canadian Vascular Access Association (CVAA). (2019). CVAA occlusion management guideline for central venous access devices (CVADs) (2nd ed., Vol. 13, Suppl. 1). CVAA.
- H.Levert, O.Albert, E.Barret, S.Villiers, & MC.Douard. (2014). A randomized experimental comparision of two safety Huber needles (HN) allowing manual or automatic positive pressure during needle removal: effect on the distal catheter reflux. WoCoVA







