Approximately 94 million infants are born each year worldwide. All of these infants are vulnerable to cold stress and thus hypothermia, regardless of their gestational age or weight. It is important to provide them with an adequate and stable environment because of their poor and impaired ability to regulate their body temperature (1).
At the beginning of the 20th century, in 1907, Pierre Budin, at the Paris Maternity Hospital, was the first neonatologist to highlight the importance of the neonatal thermal environment. Budin reported a decrease in mortality from 66 to 38% in newborns weighing less than ≤ 2,000 g after the introduction of thermal control measures (4,5).
Since then, the relevance of heat loss prevention strategies in the initial stabilization of newborns has been supported by several institutions and included in official guidelines. However, some studies point out that temperature monitoring during resuscitation in the delivery room has been carried out, so far, “never or occasionally” in 81% of the cases.
Why does a newborn lose heat after birth?
Neonatal hypothermia is a recurrent problem among newborns, the World Health Organization (WHO) asserts that it is a common complication that contributes to a high rate of perinatal mortality and poor outcomes in the patient’s normal development (2,3). It is essential that healthcare professionals involved in neonatal care understand the importance of the physiological transition and adaptation that these infants must make after birth (4).
Data in low-resource countries and settings suggest that hypothermia occurs in up to 85% of newborns admitted to medical facilities and in up to 92% of home births (2).
Although the hypothalamic thermal regulation system is functional from birth, it can be altered by the development of an illness, perinatal asphyxia, or the administration of certain drugs to the mother, which make the newborn particularly sensitive to external temperature variations (1,6,7). When the infant is exposed to cold stress conditions, it loses the ability to maintain its normal body temperature and falls into hypothermia (6).
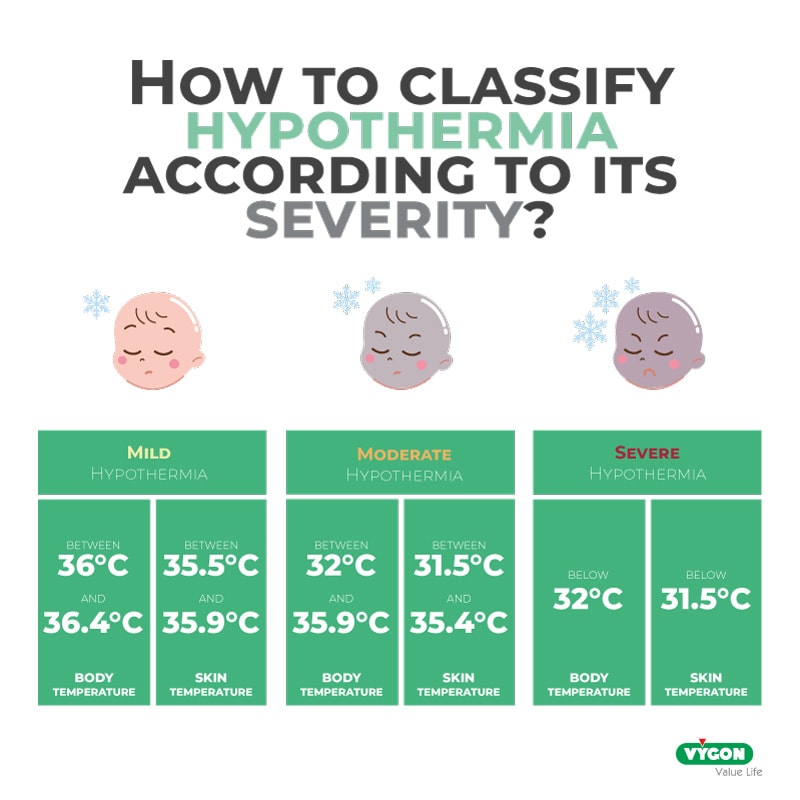
Neonatal hypothermia is defined as a temperature lower than 36.5°C. Newborns are vulnerable to hypothermia especially between 12 and 72 hours after birth (2). However, the greatest temperature drop in infants occurs in the first few minutes of life. Without adequate thermal protection, in the first 20 minutes, the infant’s temperature can drop by 2°C to 4°C (3); and for every 1°C drop in temperature, the risk of mortality increases by 28% (1).
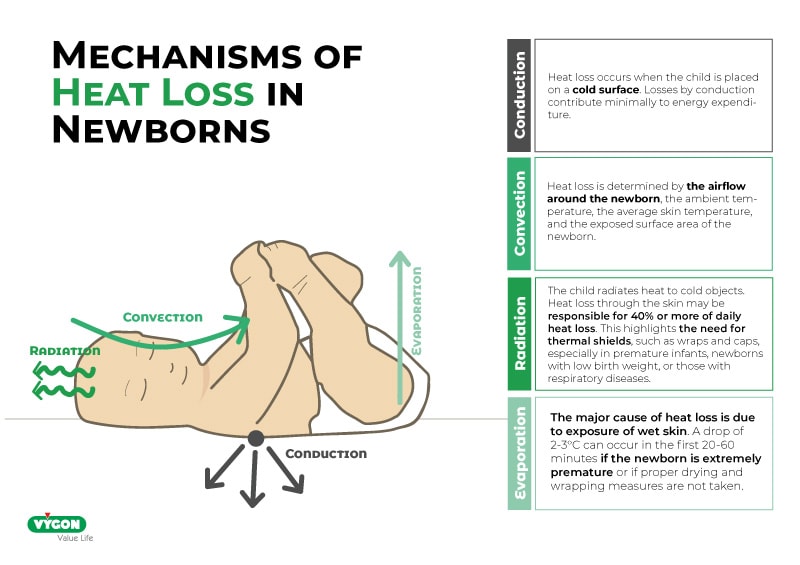
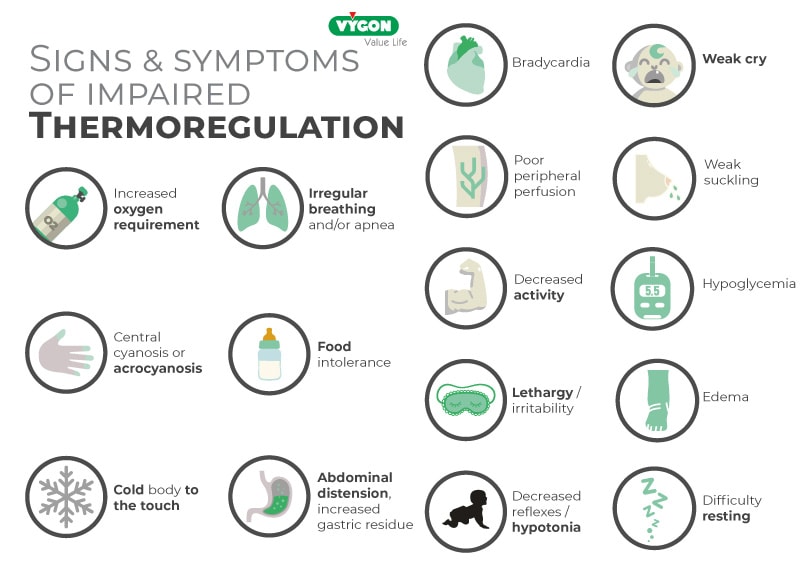
Since the newborn cannot reduce its heat loss or regulate its temperature by shivering or by increasing the activity of its voluntary muscles, the primary neonatal responses to cold stress are peripheral vasoconstriction and chemical thermogenesis. By this mechanism, acid oxidation occurs, especially of brown fat. The release of cytoplasmic triglyceride and fatty acid reserves increases metabolism leading to glucose and oxygen consumption and heat production.
This increase in oxygen consumption and metabolic expenditure contributes to increased morbidity and mortality, especially in extremely low birth weight infants. Prolonged exposure to cold stress leaves the newborn at risk as it has been linked to the development of hypoxia, hypoglycemia, metabolic acidosis or necrotizing enterocolitis (1,7).
Why is the risk of hypothermia increased in a preterm compared to a term newborn?
The aforementioned complications are in addition to many others such as hypotension, late onset sepsis, intraventricular hemorrhage and even death, the probability of which increases threefold in the first two months of life if hypothermia develops (2,5).
These are aggravated in very low birth weight or premature newborns, because gestational age, together with maternal hypertension, congenital anomalies involving skin opening, central nervous system damage or sedation are risk factors that contribute to the onset of hypothermia (8,9).
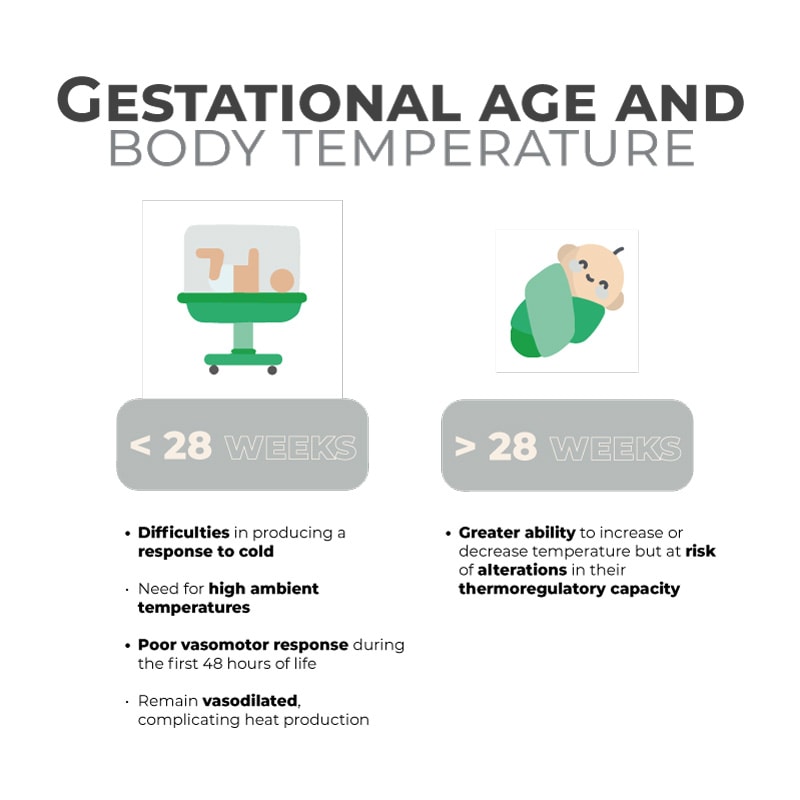
The neonate born before 28 weeks gestation presents a major challenge in the prevention of heat loss and is especially difficult to prevent in those less than 25 weeks gestation (1). Preterm and low birth weight infants also share several characteristics that make additional support for thermoregulation necessary (2,4):
- Inadequate heat production: The ability to increase metabolic rate in response to cold stress begins around 28-30 weeks gestation. Premature infants of greater maturity may increase heat production, but their response is weak due to inadequate brown fat supply, their inability to initiate mechanisms such as shivering, an underdeveloped cardiovascular and pulmonary system, and the immaturity of their skin, which increases evaporation
- Limited insulation: Poor muscle development and scanty fat layers
- Insufficient vasomotor response, due to incomplete involuntary muscle response (shivering)
- Insufficient sudomotor response: There is sweat production as early as 29 GA, but the response is slower and less efficient compared to term infants
- Decreased motor tone and activity to adopt a position with limb flexion and reduce body surface area, thus preventing heat loss
The amount of heat that can be lost by the evaporation mechanism is particularly important. This occurs in the form of insensible water losses and is known as TransEpidermal Water Loss (TEWL). TEWL has been considered to be the main factor contributing to weight loss and hypothermia in the preterm newborn. The inverse relationship between increased TEWL and lower gestational age has been demonstrated since 1979 with measurements of TEWL in preterm and term newborns. A maximum weight loss of 10-15% has been reported in preterm infants in the first days of life in relation to TEWL.
Prevention of hypothermia after birth
With the aim of minimizing the risk of hypothermia and avoiding the development of complications that can mark the growth of the newborn, especially those of a lower gestational age and lower weight, several clinical studies have been carried out with the aim of finding out which therapeutic strategies can reduce heat loss and hypothermia in the delivery room and operating rooms (4).
Some strategies, which have traditionally been used, such as skin-to-skin contact, the use of radiant heat, thorough and quick drying, and maintaining room temperature between 24°C and 28°C, are valid and allow for the regulation of newborns’ temperature. (1,4,6). However, the special characteristics of premature infants have made it necessary to supplement these actions for additional protection (6).
Recent studies have demonstrated the benefits of using polyethylene bags and polyethylene caps covering the patient’s body in premature neonates. Transparent and flexible plastic wrapping achieves better results than traditional drying in reducing the drop in body temperature, by at least 1°C, in low-birth-weight newborns (1,4,5).
In fact, more than 40 years ago Besch et al. showed the superiority of the combined use of plastic bags together with radiant heat spaces for the prevention of hypothermia due to the reduction of heat loss through the evaporation process (4,6).
It should be noted that the use of plastic covers is compatible with the resuscitation needs of premature infants. Several institutions, including the WHO, emphasize the importance of keeping infants warm during resuscitation, as an asphyxiated newborn cannot produce heat efficiently and is at greater risk of cooling down. Therefore, it is advisable to lay the newborn on a warm surface and wrap the baby in a plastic bag, leaving only the face exposed (3,4,6).
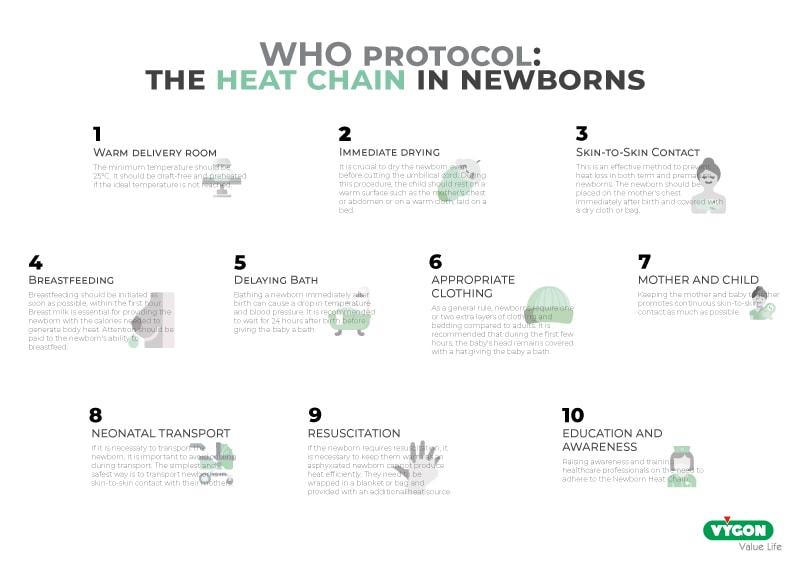
This easy-to-implement and low-cost practice can be a great tool for the care of all newborns, especially in countries with fewer resources. To improve its effectiveness, it should be accompanied by a set of strategies such as skin-to-skin contact, early initiation of breastfeeding and frequent monitoring of the baby’s temperature (3,5).
Bibliography
- Gleason, C., & Juul, S. (2020). Diseases of the Newborn. 10th ed. Barcelona: ELSEVIER, pp. 361-367. Retrieved from https://books.google.es/books?id=Ew-DDwAAQBAJ&pg=PA365&lpg=PA365&dq=por+each+ca%C3%ADda+in+1%C2%B0C+in+temperature,+increases+the+risk+of+mortality+by+28%25.&source=bl&ots=vTPTBRGEu3&sig=ACfU3U0bsOP0sZQTcHF3YajhoZ_24TWUfw&hl=en&sa=X&ved=2ahUKEwijxc21p6HpAhWlA2MBHbA1AwgQ6AEwAHoECAsQAQ#v=onepage&q&f=true
- Safe and Effective Thermal Protection for the Care of Hospitalized Newborns. Do No Harm Technical Paper, pp. 1-3. Retrieved from https://www.everypreemie.org/wp-content/uploads/sites/10/2019/09/ThermalProtection_spanish_10.22.18Revised.pdf
- World Health Organization. (1997). Maternal and Newborn Health/Safe Motherhood. Thermal protection of the newborn: a practical guide. Geneva: World Health Organization. Retrieved from https://apps.who.int/iris/handle/10665/63987
- Zamorano-Jiménez, C. A., Cordero-González, G., Flores-Ortega, J., Baptista-González, H. A., & Fernández-Carrocera, L. A. (2012). Thermal management in the preterm newborn. Perinatology and human reproduction, 26(1), 43-50. Retrieved May 11, 2020, from http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0187-53372012000100007&lng=es&tlng=es
- Julca, H., Perez Franco, B., & Jesus, S. (2016). Efectividad Del Uso De Bolsa De Polietileno Para La Prevención De La Hipotermia En Los Recién Nacidos Prematuros Y De Bajo Peso Al Nacer. Lima, pp. 11-17. Retrieved from http://repositorio.uwiener.edu.pe/bitstream/handle/123456789/472/T061_10032432_S.pdf?sequence=1&isAllowed=y
- Rodrigo, F., Rivero Rodríguez, S., & Quesada, C. (2014). Factores De Riesgo De Hipotermia Al Ingreso En El Recién Nacido De Muy Bajo Peso Y Morbimortalidad Asociada. Las Palmas de Gran Canaria: Vol. 80 No.3, pp. 144-150. Retrieved from https://www.analesdepediatria.org/es-factores-riesgo-hipotermia-al-ingreso-articulo-S1695403313003482
- Quiroga, A., Chattas, G., Gil, A., Ramírez, M., Montes, M., Iglesias, A., Plasencia, J., López, I., & Carrera, B. (2010). Clinical Practice Guideline On Thermoregulation In The Newborn. pp. 1-6. Retrieved from http://www.sld.cu/galerias/pdf/sitios/williamsoler/consenso_termoreg.pdf
- Réanimation Du Nouveau-Né En Salle De Naissance. p. 13. Available at: http://campus.cerimes.fr/maieutique/UE-puericulture/reanimation_nne/site/html/cours.pdf
- Stavis, R. (2017). Newborn Small For Gestational Age. Merck Manuals. Available at: https://www.merckmanuals.com/es-pr/professional/pediatría/problemas-perinatales/recién-nacido-pequeño-para-la-edad-gestacional-peg






