This article provides a comprehensive, data-driven comparison between local-regional anaesthesia and general anaesthesia, demonstrating why local-regional anaesthesia is a superior option for the modern, environmentally conscious clinician. Its goal is to highlight the clear benefits of switching to more sustainable techniques without compromising the quality of care. In this article, you will find:
- A direct comparison of the carbon footprint (CO2e) of each technique, revealing an overwhelming difference.
- Clear evidence of improved patient outcomes, including faster recovery and fewer post-operative complications.
- An analysis of how local-regional anaesthesia reduces the consumption of drugs and other medical resources.
The Hidden Challenge: Addressing the Environmental Footprint of the Operating Room
In the modern healthcare landscape, hospitals are under increasing pressure to reduce their environmental footprint. While many sustainability initiatives focus on energy or physical waste, one of the most significant contributors to a hospital’s carbon emissions often remains hidden: the choice of anaesthesia.
General anaesthesia, long the cornerstone of surgery, is associated with high carbon emissions, excessive drug use, and more postoperative complications.
Many dedicated clinicians, committed to providing the highest quality of care, are simply unaware that a powerful and sustainable alternative is already within their reach.
This article aims to close the knowledge gap by demonstrating, with clear, evidence-based data, that loco-regional anaesthesia is an effective, safe and environmentally friendly alternative in certain situations. Moving towards sustainability in the operating room is an improvement, not a sacrifice.
The Data Speaks: A stark Comparison of Anaesthesia Carbon Footprints
When evaluating the environmental impact of general anaesthesia, the numbers speak for themselves. The debate about sustainability must be based on data, and the evidence reveals a stark disparity between general anaesthesia and local-regional anaesthesia.
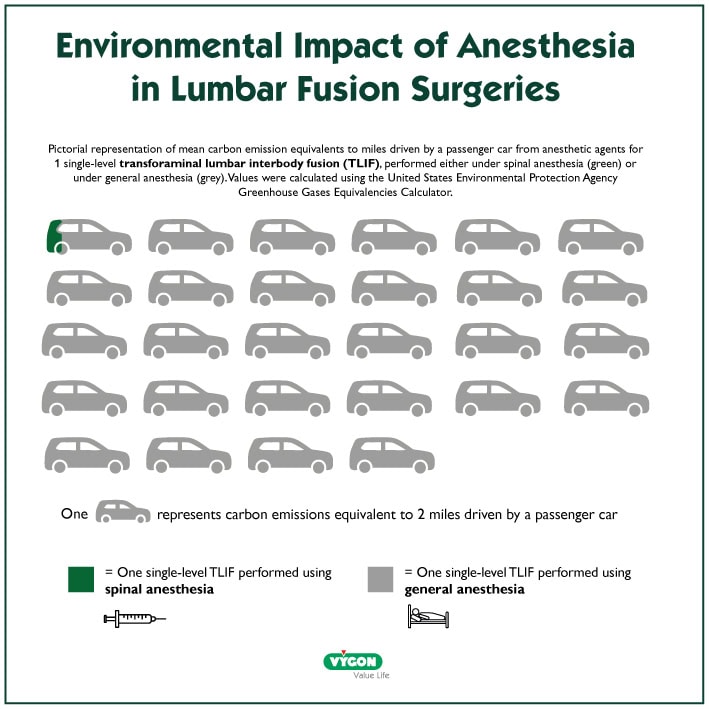
A life cycle analysis conducted in spine surgery, which considers all greenhouse gas emissions and translates them into a single comparable unit (CO2 equivalent or CO2e), offers a striking contrast.
- A single procedure with spinal anaesthesia (LRA) generates an average carbon footprint of just 63 g of CO2e.
- The same procedure under general anaesthesia (GA) produces a whopping 22,707 g of CO2e.
(Based on a life cycle analysis in spine surgery à includes all greenhouse gas emissions translated into CO₂ equivalent) This is not an abstract figure. Choosing local-regional anaesthesia for a single procedure avoids pollution equivalent to driving a car for 91.5 kilometers (56.9 miles).
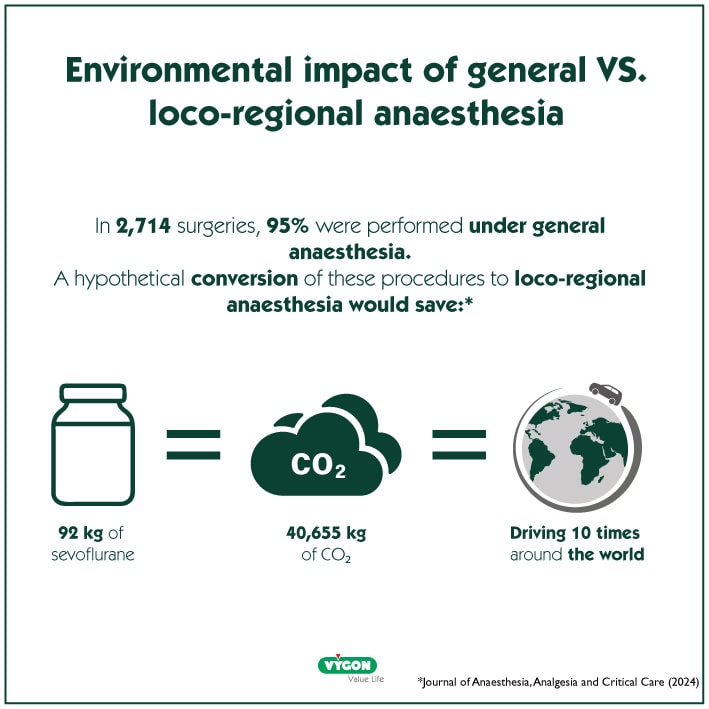
This drastic reduction becomes incredibly powerful at scale. A study referenced by Wang et al. analyzed 2,714 surgeries (hand, wrist, hip, and ankle), of which 95% were performed under general anaesthesia. A hypothetical conversion of these procedures to loco-regional anaesthesia would save 92 kg of sevoflurane, equivalent to 40,566 kg of CO2 , enough pollution to drive around the world 10 times.
Beyond Emissions: The Domino Effect of Clinical and Resource Benefits
The environmental advantages of local-regional anaesthesia extend far beyond the direct reduction of greenhouse gas emissions. The choice of technique creates a positive domino effect, significantly reducing the consumption of pharmaceuticals and medical devices, which in turn have a manufacturing and disposal footprint.
- Less need for postoperative opioids, such as morphine, which helps mitigate the risk of dependence and side effects.
- Avoids the use of muscle relaxants (curare), eliminating the complexities and risks associated with their administration and reversal.
- Avoids the use of difficult intubation procedures and controlled ventilation, eliminating the need for associated drugs and equipment.
- Using ultrasound during the procedure enables healthcare professionals to visualize target nerves and the spread of anaesthetic in real time. Using ultrasound guidance reduces the total volume of anaesthetic administered while maintaining efficacy.
Perioperative hemodynamic management made easy, affordable, and green – By Frédéric Michard
Efficacy and Patient Recovery: The Undeniable Double Victory
A crucial question for any clinician is whether a sustainable option compromises efficacy. With regional anaesthesia, the answer is a resounding no.
Multiple studies and clinical experiences affirm that regional anaesthesia is equally, and in some cases, even more effective than general anaesthesia for a wide range of procedures, all while boasting a much lower carbon footprint.
This conclusion holds even when considering the plastic waste associated with regional anaesthesia kits, a point confirmed by S.M. White and C.L. Shelton in Anaesthesia (2019). It is not a choice between “green” and “effective,” but rather a matter of achieving both.
The benefits for the patient are equally compelling, creating a clear “double win.”
- Regional anaesthesia is associated with better postoperative pain relief and fewer side effects such as nausea, vomiting, and itching.
- It facilitates better postoperative rehabilitation and mobilization, which can lead to shorter hospital stays and faster discharge.
- In outpatient hip and knee arthroplasty, patients under spinal anaesthesia have a higher same-day discharge rate compared to those under general anaesthesia (77% vs. 67%).
- Patients also experience less respiratory depression or other side effects.
This synergy of ecological responsibility and patient-centered care is what makes local-regional anaesthesia a truly revolutionary approach in modern medicine.
Adopting a New Standard of Responsible Anesthesiology
The evidence is clear and compelling. The choice between local-regional anaesthesia and general anaesthesia is a strategic decision with profound implications for sustainability, resource management, and patient well-being.
By adopting regional anaesthesia, the anesthesiology community can lead an important ecological transformation in the healthcare sector. It is a tangible, immediate, and evidence-based step toward a more sustainable and responsible practice, where clinical excellence and environmental stewardship go hand in hand.
Bibliography:
- Assessing the Environmental Carbon Footprint of Spinal versus General Anaesthesia in Single-Level Transforaminal Lumbar Interbody Fusions Wang et al., 2022. World Neurosurgery.
- Carbon footprint in trauma surgery, is there a way to reduce it? Journal of Anaesthesia , Analgesia and Critical Care (2024)
- Anesthésie locorégionale en orthopédie – s. Saadallah, z. Dahoumane – Algerian medical journal, December 2022
- Abandoning inhalational anaesthesia White & Shelton, Anaesthesia, 2019).






