Catheter occlusion is one of the most common complications associated with central venous access devices (CVADs). Its reported incidence rates range from 3% to as high as 79%1.
This complication can significantly impact patient care and can, in some cases, even contribute to more severe clinical consequences, including increased morbidity and mortality.
Preventing catheter occlusion is therefore a critical priority in clinical settings. One effective strategy involves the use of some type of needle-free connectors, which have been shown to reduce the risk of intraluminal thrombus formation.
In this article, we will explore the nature and consequences of catheter occlusions, then examine how needle-free connectors could be a potential solution.
Read on to find out how a small and simple device could make a difference in patient safety.
Types of catheter occlusion
Catheter occlusion can be defined as partial or complete blockage of the catheter lumen, which hinders or prevents the flow of fluids or medications2.
Catheter occlusion types are classified into three main categories3:
- Mechanical occlusions: These are caused by physical issues either inside or outside the catheter. Common causes include catheter kinking, displacement of the catheter tip, partial dislodgement of the catheter, or incorrect placement of a Huber needle in an implantable port.
- Chemical occlusions: These can result from the mixing of incompatible medications, or residue from lipids or drugs accumulating inside the catheter.
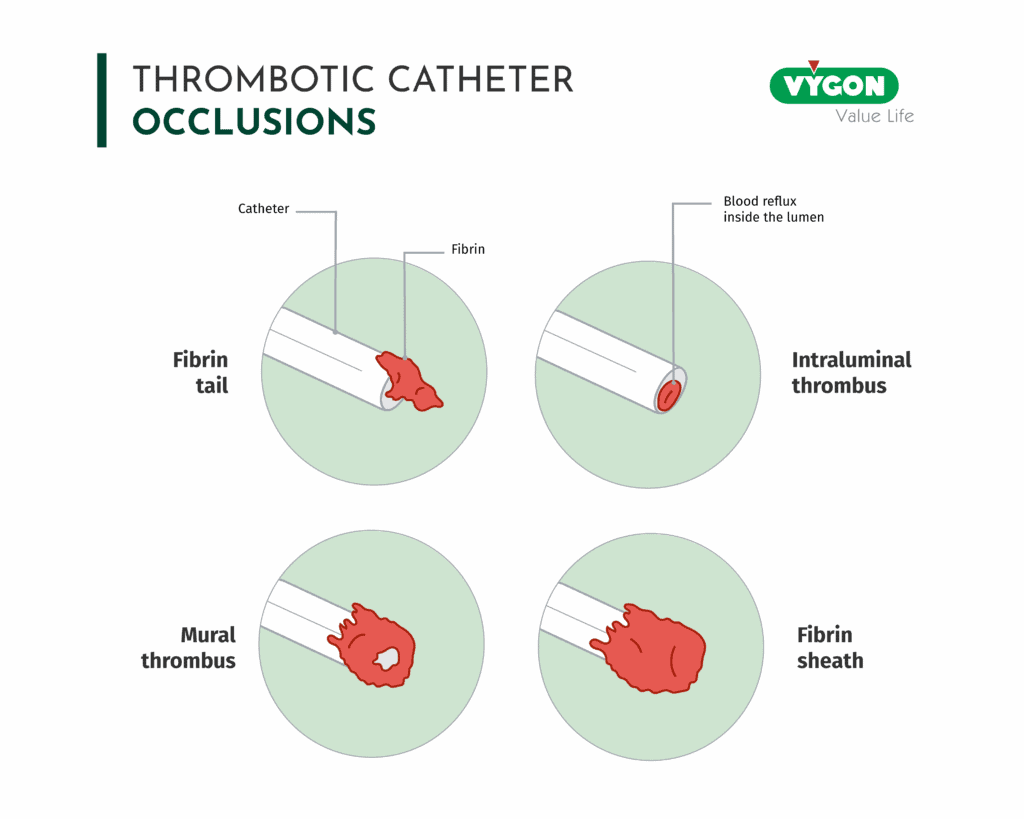
- Thrombotic occlusions: These involve the formation of a blood clot (thrombus) inside the catheter, around it, or in the surrounding vein. Thrombotic occlusions may present as an intraluminal thrombus, a fibrin tail or flap, a fibrin sheath or sleeve, or a mural thrombus.
In cases of thrombotic occlusion, catheter-related thrombosis may be classified as follows:
- Partial occlusion: Characterized by slow or sluggish flow through the catheter.
- Persistent withdrawal occlusion: The catheter can be flushed, but aspiration (withdrawal of blood) is not possible.
- Total occlusion: Neither flushing nor aspiration through the catheter is possible.
Consequences of catheter occlusion
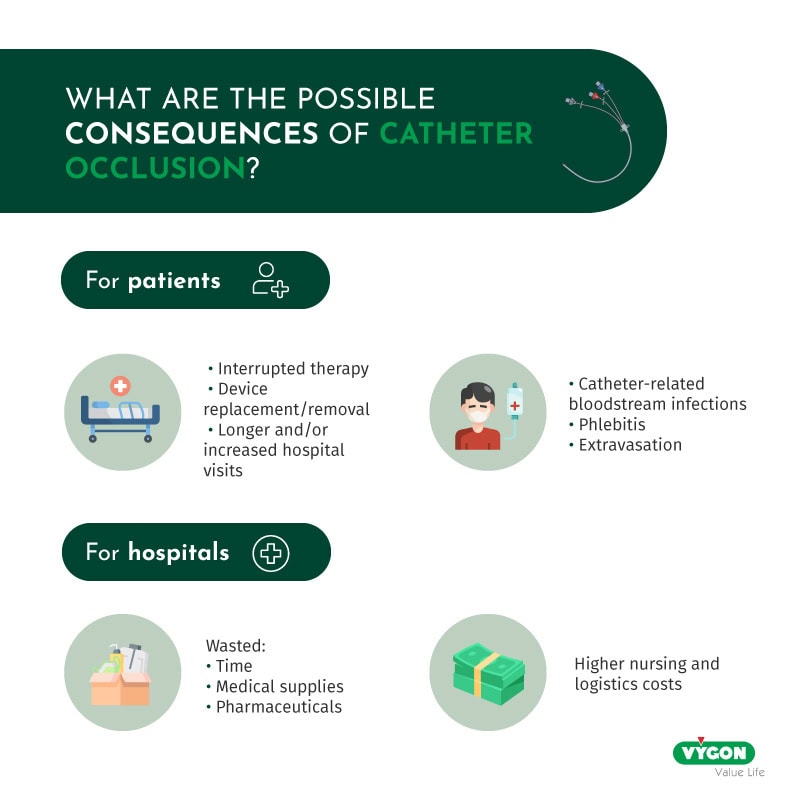
Catheter occlusion can significantly impact both patients and healthcare facilities.
For patients, it is most commonly associated with therapy interruption due to loss of patency (43%). It may also lead to device replacement (29%) or removal (14%), and in some cases, increased hospital visits (15%). These complications can delay treatment and prolong hospital stays. They are often painful and distressing, with a negative impact on the patient’s overall well-being. Moreover, it does not only hinder the patient’s therapeutic progress but also increases the risk of complications acquired in hospitals.
For instance, occlusions raise the risk of catheter-related bloodstream infections (CRBSI), phlebitis and extravasation, posing serious safety concerns. In severe cases, they can increase the risk of mortality. Moreover, managing occlusions often involves the use of thrombolytic agents like tissue plasminogen activator (tPA), which has been associated with an increased risk of CRBSI1.
For hospitals, catheter occlusion represents a substantial economic burden. It results in wasted time, medical supplies, pharmaceuticals, and increased nursing and logistical costs.1
These consequences highlight the importance of prevention, early detection, and proper management of catheter occlusions to protect both patient health and healthcare resources. Following international guidelines and recommendations, such as those of the INS4, is indeed essential to ensure best practices and reduce the risk of catheter occlusions.
In addition to these guidelines, other preventive measures can also be considered. One option is the use of needle-free connectors.
The role of anti-reflux needle-free connectors in preventing catheter occlusion
Needle-free connectors (NFCs) are medical devices designed to provide safe and quick access to intravenous (IV) lines for the administration of fluids and medications.
Initially developed to prevent needlestick injuries5, early NFC designs (specifically those using positive and negative flush), required complex clamping protocols. This led to user confusion and increased risk of complications such as CLABSI5.
In response to safety concerns, including those raised by the FDA, device designs were later improved. As a result, neutral anti-reflux NFCs were developed, and proved to be effective in preventing occlusion3,5.
Anti-reflux NFCs are engineered with pressure-sensitive valves in order to prevent blood reflux in all phases of use5. In fact, according to Buzas6, these devices exhibit minimal reflux.
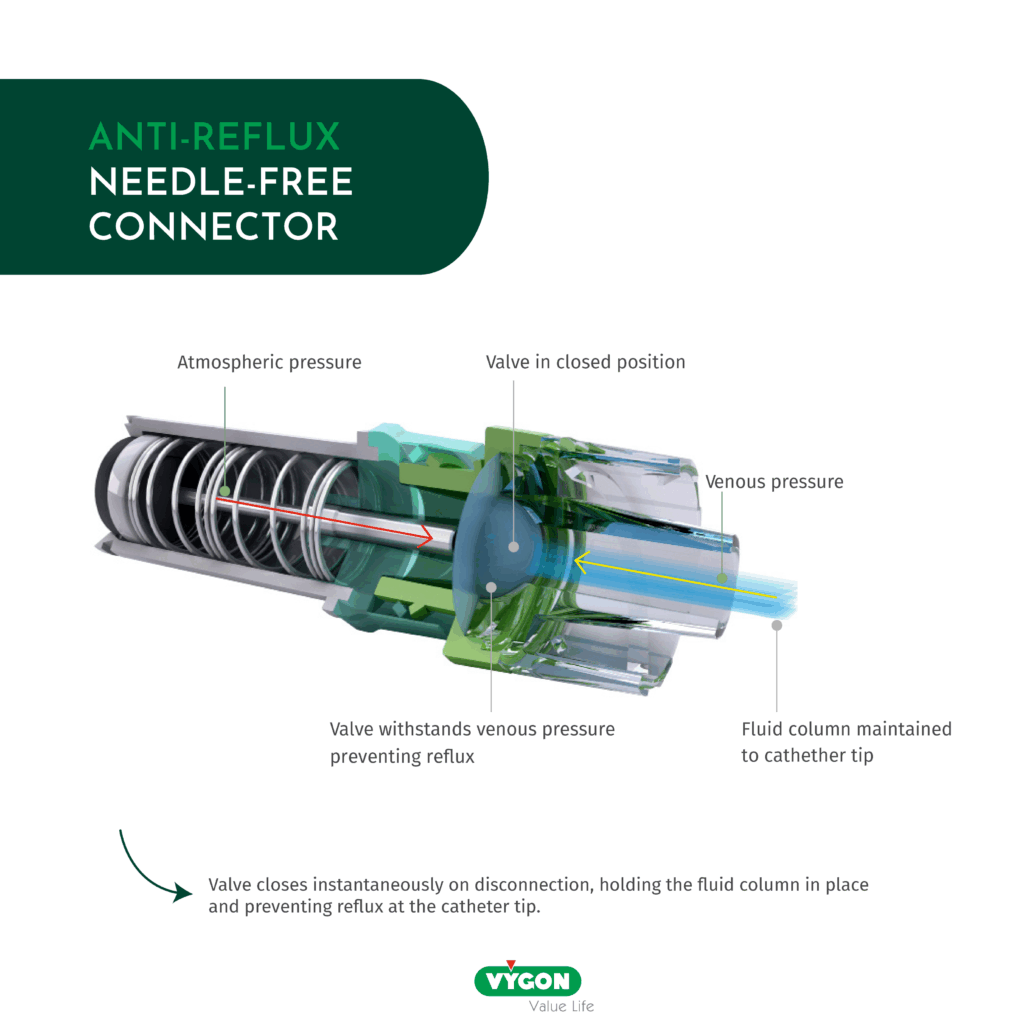
This is particularly important because blood reflux is a leading cause of catheter occlusion, accounting for up to 58% of all occlusion cases 2. Since it is largely influenced by flushing and locking practices, incorporating anti-reflux technology plays a critical role in reducing occlusions and therefore, improving patient safety and clinical efficiency.
According to Jasinsky and Wurster7, the use of an anti-reflux NFC significantly reduced occlusion rates in PICCs and CVCs, decreasing from 30% in the first month to 7.6% in the second month, and finally to 12.5% in the third month. Maurer9 reported similar positive results, with line blockage going from 59% in 2011 to 4.2% in a period going from 2012 to 2016. Hitchcock8 also observed a reduction in occlusions, with a total occlusion rate of 0.4/1000 catheter days.
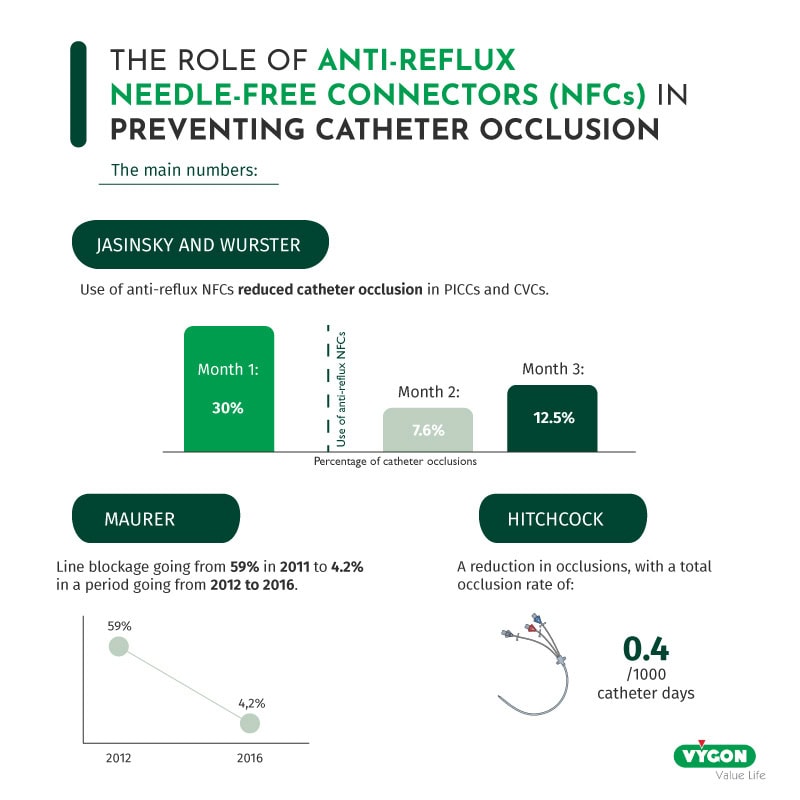
This decrease in occlusion has significant financial benefits for hospitals as it implies reduced drug use (alteplase or heparin), fewer catheter replacements and saved nursing time. Due to the reduction of the heparinized saline, Hitchcock8 reported £14,553 plus VAT saved based on 9702 catheter days. Buzas8 has also documented fixed cost savings of $124,370 over the study period, accounting to 28% savings in supply costs, 27% in nursing costs and 27% in pharmacy costs.
Beyond occlusion prevention, NFCs also contribute to infection control. As Moureau et al.2 explain, they automatically seal upon disconnection, minimizing the risk of microorganism entry into the catheter.
Needle-free connectors (NFCs) offer several clinical and economic benefits, notably by reducing needle-stick injuries, catheter occlusions, and catheter-related bloodstream infections (CRBSI).
Additionally, their effectiveness in preventing catheter occlusions is particularly well-documented in the literature, reinforcing their relevance in clinical practice. Given the growing body of evidence, NFCs appear to be a proven and valuable solution in the ongoing effort to improve patient safety and reduce healthcare costs.
Bibliography
- Steere, Lee, et al. « Lean Six Sigma for Intravenous Therapy Optimization: A Hospital Use of Lean Thinking to Improve Occlusion Management ». Journal of the Association for Vascular Access, vol. 23, no 1, march 2018, p. 42‑50. https://doi.org/10.1016/j.java.2018.01.002.
- Moureau, Nancy, et al. « A Systematic Review of Needleless Connector Function and Occlusion Outcomes: Evidence Leading the Way ». Journal of Infusion Nursing, vol. 48, no 2, march 2025, p. 84‑105. https://doi.org/10.1097/NAN.0000000000000578.
- Canadian Vascular Access & Infusion Therapy Guidelines, CVAA Occlusion Management Guideline for Central Venous Access Devices (CVADs), 2019 Second Edition.
- Infusion Nurses Society (INS), Infusion Therapy Standards of Practice, 9th edition, Revised 2024.
- Rosenthal, Victor Daniel. « Clinical Impact of Needle-Free Connector Design: A Systematic Review of Literature ». The Journal of Vascular Access, vol. 21, no 6, november 2020, p. 847 53. https://doi.org/10.1177/1129729820904904
- Buzas. « Keeping You Connected: Anti-Reflux Connectors Reduce Catheter Occlusions and Use of Alteplase ». National Home Infusion Association 2021 Annual Conference.
- Jasinsky, Lisa M., et Julie Wurster. « Occlusion Reduction and Heparin Elimination Trial Using an Antireflux Device on Peripheral and Central Venous Catheters ». Journal of Infusion Nursing, vol. 32, no 1, january 2009, p. 33 39. https://doi.org/10.1097/NAN.0b013e3181921c56.
- Hitchcock, Jan. « Preventing Intraluminal Occlusion in Peripherally Inserted Central Catheters ». British Journal of Nursing, vol. 25, no 19, october 2016, p. S12 18. https://doi.org/10.12968/bjon.2016.25.19.S12.
- Maurer and CDFFT IV Team. « Reducing the occlusion rates of peripheral midlines, our 5 years experience using Bionector TKO needle free connectors » Presentation[HC1] [PT2]. County Durham and Darlington, NHS Foundation Trust.







