Every day in neonatology, just a few seconds can make the difference between the stability of a preterm infant and the onset of a critical event. Among these silent threats, necrotizing enterocolitis (NEC) remains one of the most feared. This article provides you with practical, evidence-based tools to strengthen your daily practice.
Necrotizing enterocolitis (NEC) is a severe gastrointestinal disease that affects preterm infants. Its rapid progression, high mortality rate, and risk of long-term digestive complications make it a major neonatal concern. Management and prevention require a multidisciplinary strategy combining strict hygiene, rigorous feeding protocols, early diagnosis, and continuous vigilance.
The recommendations presented in this article are based on an analysis of recent literature, meta-analysis, and systematic reviews involving several thousand premature infants. The data come from more than 50 randomized clinical trials, guidelines published in Pediatric Neonatology (2024), and key studies on feeding, probiotics, hygiene, and enteral feeding devices. This takes part in building up the essentials to know about the NEC management.
Hand Hygiene1
Hand hygiene plays a fundamental role in preventing infections in Neonatal Intensive Care Units (NICUs). Strict adherence to established protocols is essential to limit the transmission of pathogens that may contribute to the development of NEC.
- Thorough handwashing with soap and water, or the use of an alcohol-based hand sanitizer, must be performed before and after handling newborns or enteral feeding equipment.
- The use of strict aseptic techniques when preparing and administering enteral nutrition is crucial to minimize the risk of microbial contamination.
Several studies have confirmed that improving hand hygiene compliance in NICUs significantly reduces the incidence of NEC and other neonatal infections.
Enteral Feeding practices
Feeding strategies play a critical role in NEC prevention. Proper feeding protocols can help promote gut maturation and reduce the risk of intestinal inflammation.
Standardized Feeding protocol
- Start with minimal enteral nutrition (MEN), also known as trophic feeding, helps stimulate the development of the immature gut.
- Gradually increase feeding volumes according to standardized protocols to prevent gut ischemia and inflammation of the intestine.
- Avoid hyperosmolar formulas, which may contribute to mucosal injury2
- Avoid acid-suppression medications that may alter the microbiome3
Human Milk as the Preferred Nutrition Source4
Human milk provides essential bioactive components that support gut integrity and immune function. Compared to formula feeding, exclusive human milk feeding has been associated with a lower incidence of NEC.
- Breast milk contains immunoglobulins, lactoferrin, and anti-inflammatory factors that protect the neonatal gut.
- Fortification with human milk-based fortifiers is recommended for preterm infants requiring additional nutrients while minimizing NEC risk.
- Donor human milk is a viable alternative when maternal milk is unavailable, as it retains many protective properties.
Administration of probiotics5
Probiotic supplementation has been shown to reduce the risk of NEC by nearly 50% in preclinical studies. Systematic reviews and meta-analysis of over 50 randomized controlled trials (RCTs) involving more than 10,000 preterm infants have found that probiotics reduce the incidence of NEC. Probiotics may help strengthen the intestinal barrier, reduce inflammation, and inhibit pathogen growth. However, there is heterogeneity in the RCTs regarding the type of probiotics used and the gestational age or birth weight of the infants included, which can complicate the interpretation of results.

Antibiotic management6
Recent research has shown that the long use of oral prophylactic antibiotic ( > 5 days) for NEC prevention may be counterproductive and could increase the risk of NEC. Although some older studies suggesting potential benefits of using antibiotics to prevent NEC, concerns about antibiotic resistance and gut microbial imbalance have been raised and the recommendations tend to limit the use of antibiotics in preterm infants, especially when there is no confirmed infection.
Enteral Feeding tube’s cleaning
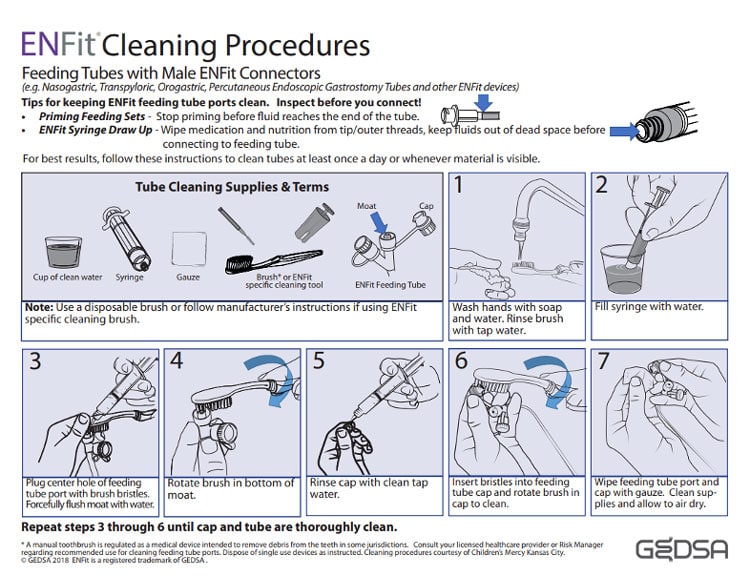
The ENFitTM enteral feeding system, while designed to enhance safety by preventing misconnections, presents a specific challenge in neonatal intensive care units (NICUs) concerning the risk of microbial contamination. This contamination may significantly increase the risk of necrotizing enterocolitis (NEC) in preterm infants. Indeed, the intricate design of ENFitTM connectors traps liquid in its moat and requires meticulous cleaning to prevent bacterial colonization. That’s why a cleaning protocol for ENFitTM feeding tubes must be implemented and repeated at least once a day or whenever residues are visible. This below GEDSA guideline aims to provide NICU staff with the required cleaning protocol:
GEDSA cleaning procedure7
- Preparation: Begin by washing your hands thoroughly with soap and water to prevent contamination. Fill a syringe with clean water, which will be used to flush the feeding tube.
- Cleaning the Feeding Tube Port: Rinse the brush with tap water. Use the brush to plug the center hole of the feeding tube port and forcefully flush the moat with water to remove any debris. This step is crucial for dislodging any particles that may have accumulated in the port.
- Cleaning the Cap: Rinse the cap with clean tap water. Insert the bristles of the brush into the feeding tube cap and rotate the brush to clean the inside thoroughly. This ensures that any residue within the cap is effectively removed.
- Final Steps: Wipe the feeding tube port and cap with gauze to remove any remaining moisture or particles. Allow all cleaned supplies to air dry completely before reusing them. This step helps prevent the growth of bacteria and ensures the equipment is ready for the next use.
Unfortunately, studies showed that the ENFitTM cleaning protocols fail, and bacterial residues remain trapped into the ENFitTM feeding tubes’ connector. Therefore, using medical devices specifically designed for premature infants, devices that reduce the risk of misconnections while minimizing the need to focus on complex cleaning protocols, is essential to lower contamination risks and optimize caregivers’ workload⁸.
Bibliography
- Best, C. (2008). Enteral tube feeding and infection control: how safe is our practice?. British Journal of Nursing, 17(16), 1036-1041.
- Entérocolite nécrosante – Pédiatrie – Édition professionnelle du Manuel MSD
- Colarelli A. & Al., Prevention Strategies and Management of Necrotizing Enterocolitis, Pediatric Neonatology, Volume 10, pages 126–146, (2024)
- Abrams, S.A., et al. (2014). Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeeding Medicine, 9(6), 281-285.
- Colarelli, A. M., Barbian, M. E., & Denning, P. W. (2024). Prevention Strategies and Management of Necrotizing Enterocolitis. Current treatment options in pediatrics, 10(3), 126-146.
- Colarelli A. & Al., Prevention Strategies and Management of Necrotizing Enterocolitis, Pediatric Neonatology, Volume 10, pages 126–146, (2024)
- https://stayconnected.org/enfit-cleaning-procedures-all-tubes/
- Girgenti, C., & Hyde, J. (2024.). Understanding feeding tube risks associated with necrotizing enterocolitis.






