With the introduction of venous mapping methods prior to the placement of a central venous catheter (RaPeVA, RaCeVA, and RaFeVA), the evolution of ultrasound techniques has given a fundamental role to the choice of vein. In fact, the measurement of this vein (obtained in mm) allows vital information to be obtained to prevent complications related to the place taken by the catheter.
In this regard, two key questions arise:
- If the vein measurement is in mm and the diameter of catheters is expressed in Fr or Gauge, is it possible to have an equivalence?
- What is the appropriate Catheter to Vein Ratio (CVR) knowing that nowadays, reference groups in vascular access do not agree in their recommendations?
MEASUREMENT UNITS: EQUIVALENCE BETWEEN CATHETER AND VEIN
MEASUREMENT UNITS USED FOR VASCULAR ACCESS DEVICES
Within the range of available vascular accesses, different measurement units are used for the external and internal diameter of the catheter.
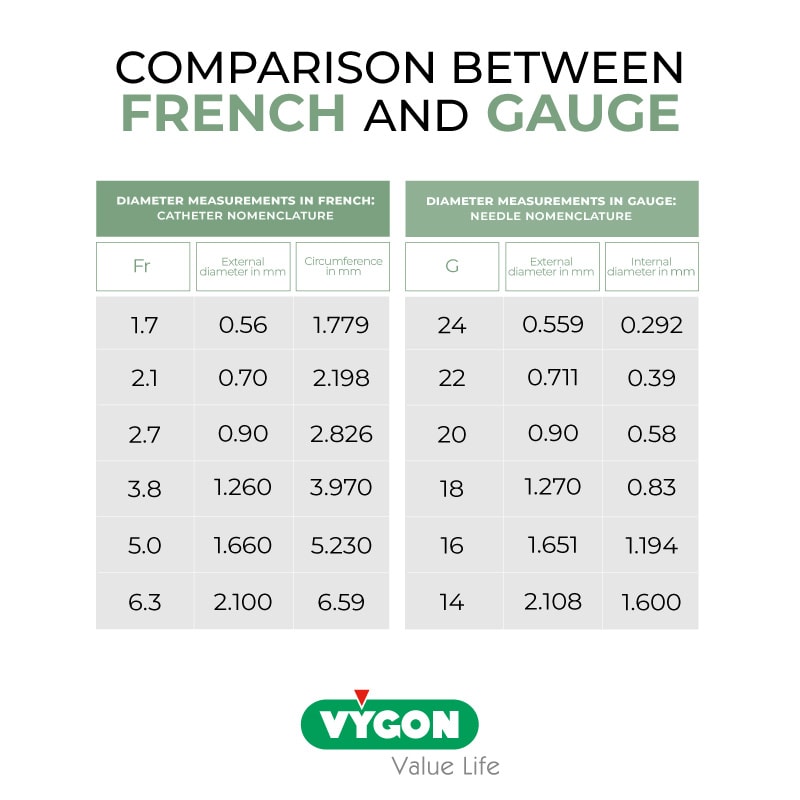
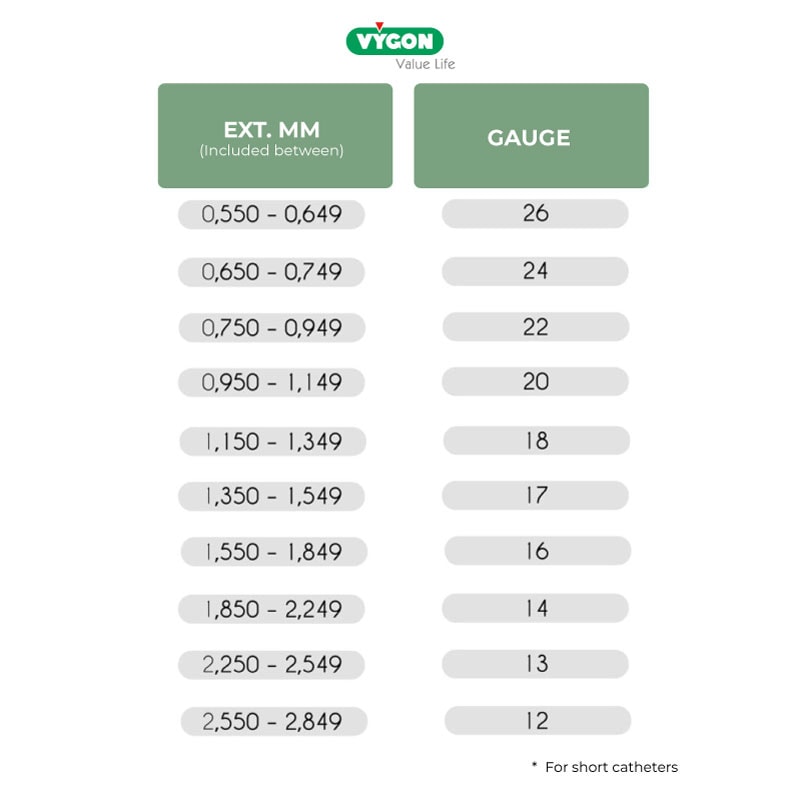
The short catheter is characterized by a diameter measured in Gauge (G). It measures the internal diameter of the catheter. The particularity of Gauge is as follows: the wider the diameter, the smaller the measurement in G, and vice versa.
Midlines, PICC, reservoirs, and Hickman catheters have a diameter whose measurement is expressed in French (Fr). In this case, the measurement in Fr varies in the same way as the device: a small catheter will have a small French, and vice versa. Fr measures the external diameter of the catheter. In central catheters, it is possible to observe both units of measure: the external diameter of the catheter expressed in French and the diameter of the lumens expressed in Gauge:

EQUIVALENCE BETWEEN THE MEASUREMENT OF THE VEIN AND THE CATHETER
The vast majority of ultrasound machines give the measurement in mm and conversion tables can be used to correctly choose the catheter. The unit of measure for catheters that we most commonly encounter when placing catheters with guides is the French, which corresponds to 1/3 of a mm:
1Fr = 0.33mm
As we mentioned, Fr is used to measure the external calibre of devices. The G (Gauge) is used to measure the internal diameter. Therefore, when determining how much space the catheter can occupy, it is necessary to refer to the Fr.
There is no exact equivalence between all units of measure, but literature that can help determine the equivalence between Gauge, French, and mm exists:
INTERNATIONAL RECOMMENDATIONS ON CATHETER TO VEIN RATIO (CVR)
CVR USED IN EUROPE
The size of the catheter we are going to place inside the vein plays an important role.
In 2011, Nifong demonstrated with an in vitro study how blood flow was reduced with a smaller venous calibre and a larger external diameter of the catheter. Thanks to this study, international organizations such as GAVeCeLT urge us to carefully observe both the venous calibre -which can only be observed and calculated with ultrasound- and the external diameter of the catheter.
The purpose of this observation is to prevent complications, particularly thrombosis, whose risk of occurrence increases proportionally with the thickness of the catheter.
To achieve this, the standard recommended by GAVeCeLT is to leave at least two-thirds of the vein diameter free for the flow surrounding the catheter:
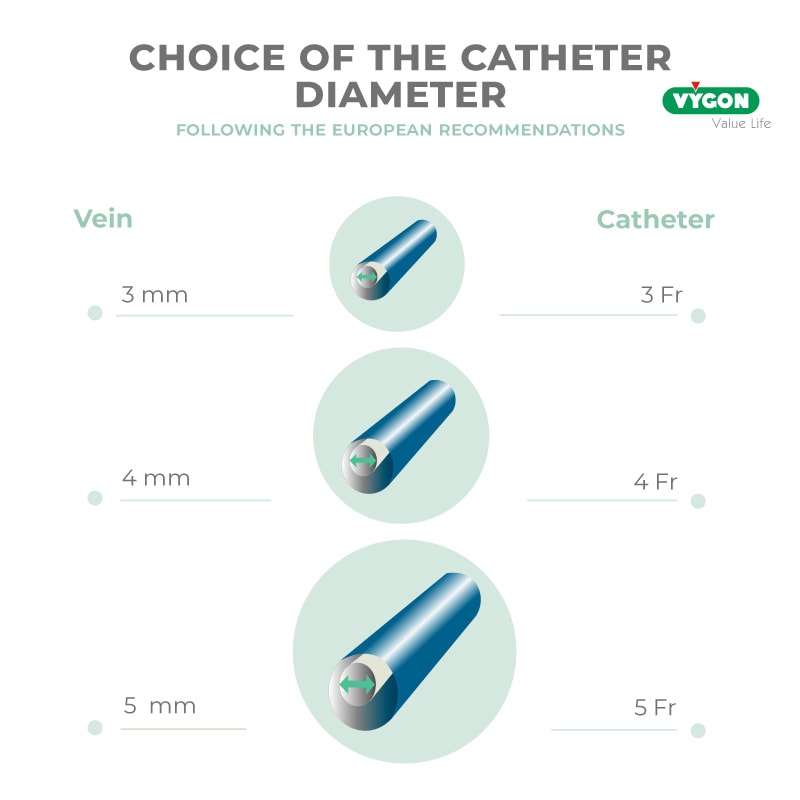
This means that if we follow this recommendation, 33% of the vein should be occupied by the catheter and not more.
This easy-to-remember rule ensures flow around the catheter, although we cannot forget that, even when these criteria are met, thrombosis sometimes occurs. However, it is true that with ultrasound-guided micro puncture and respecting the catheter to vein ratio, the chances of it occurring are greatly reduced.
CVR USED IN ANGLO-SAXON COUNTRIES
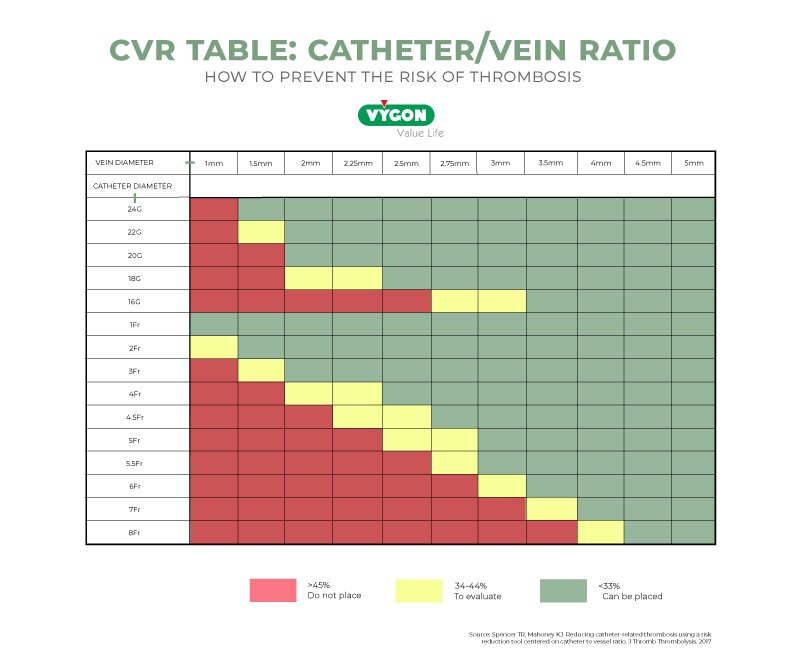
Recently, research teams have questioned the 33% CVR and have been interested in finding out what level of catheter occupancy would be an exact cut-off to prevent thrombosis.
The Sharp et al. 2021 study, conducted on over 2400 patients, aimed to determine the effect of the catheter/vein ratio (CVR) on symptomatic thrombosis rates in people with a PICC catheter and to identify the optimal cut-off point. They came to the following conclusions:
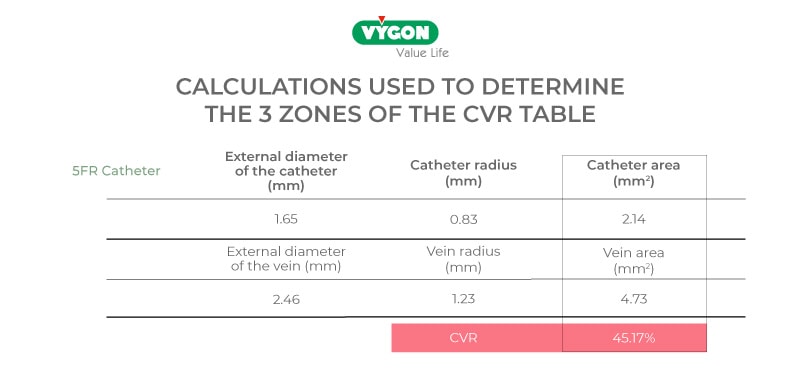
A cut-off point of 45% was predictive of thrombosis. Those with a higher proportion had more than double the risk, while a CVR of 33% was not associated with statistically significant outcomes overall or in those with malignancy. Further research is needed on this topic.
Similarly, less conservative societies such as the INS consider that vessel occupancy by 45% of the catheter is acceptable if the objective is to reduce thrombosis.
In 2017, Spencer and Mahoney presented a study in which they developed a tool to help calculate the catheter’s Fr with respect to the vein and indicate the CVR involved in each case.
This model is more commonly used in the United States:
As a general rule, we will always choose the smallest calibre necessary for the treatment to be followed. For example, if the patient needs continuous parenteral nutrition and gastric protection, we will need at least 2 catheter lumens since each drug has to pass through an exclusive lumen. This implies that a 2-lumen catheter will have a larger Fr than a single-lumen catheter, and therefore we will have to look for the vein that allows the greatest space for flow around the catheter.
If, on the other hand, the patient needs hydration for 8 hours and analgesia every 4 hours, we can consider a single-lumen catheter, and in this case, we will opt for the smaller Fr.
As specialists in venous access, it is our duty to make decisions and choose the most appropriate material possible to avoid complications such as thrombosis. Here are some possible symptoms of thrombosis:
- Pain
- Swelling of the limb
- Oedema, difficulty moving the joint
- Engorgement of veins or appearance of collateral veins.
To achieve this, the use of ultrasound is fundamental, and it is always necessary to carry out a complete prior assessment of the patient’s vascular map. We can do this systematically thanks to the different assessment protocols promoted by GAVeCeLT, such as RaPeVA, RaCeVA, and RaFeVA.
If the required venous calibre is not achieved in the green zone of Dawson, it is always possible to puncture in the yellow zone in a larger calibre vein and tunnel the catheter to the green zone.
BIBLIOGRAPHY
- Massimo Lamperti et.al, International evidence-based recommendations on ultrasound-guided vascular access, Intensive Care Medicine volume 38, pages 1105–1117 – 2012
- Spencer TR, Mahoney KJ. Reducing catheter-related thrombosis using a risk reduction tool centered on catheter to vessel ratio. J Thromb Thrombolysis. Nov;44(4):427-434. – 2017
- Sharp et al., Catheter to vein ratio and risk of peripherally inserted central catheter (PICC)-associated thrombosis according to diagnostic group: a retrospective cohort study
- Infusion Nursing Society, 2021
- Spencer TR, Pittiruti M. Rapid Central Vein Assessment (RaCeVA): A systematic, standardized approach for ultrasound assessment before central venous catheterization. J Vasc Access. 2019 May;20(3):239-249. doi: 10.1177/1129729818804718. Epub 2018 Oct 4. PMID: 30286688.
- Brescia F, Pittiruti M, Ostroff M, Biasucci DG. Rapid Femoral Vein Assessment (RaFeVA): A systematic protocol for ultrasound evaluation of the veins of the lower limb, so to optimize the insertion of femorally inserted central catheters. J Vasc Access. 2021 Nov;22(6):863-872. doi: 10.1177/1129729820965063. Epub 2020 Oct 16. PMID: 33063616.
- Dawson R, PICC Zone Insertion Method™ (ZIM™): A systematic approach to determine the ideal insertion site for PICCs in the upper arm. JAVA. 2011 Sept; 16:156-65. doi = {10.2309/java.16-3-5}
- Bertoglio S, Annetta MG, Brescia F, Emoli A, Fabiani F, Fino M, Merlicco D, Musaro A, Orlandi M, Parisella L, Pinelli F, Reina S, Selmi V, Solari N, Tricarico F, Pittiruti M. A multicenter retrospective study on 4480 implanted PICC-ports: A GAVeCeLT project. J Vasc Access. 2022 Jan 17:11297298211067683. doi: 10.1177/11297298211067683. Epub ahead of print. PMID: 35034480.
- Pittiruti M, Bertollo D, Briglia E, Buononato M, Capozzoli G, De Simone L, La Greca A, Pelagatti C, Sette P. The intracavitary ECG method for positioning the tip of central venous catheters: results of an Italian multicenter study. J Vasc Access. 2012 Jul-Sep;13(3):357-65. doi: 10.5301/JVA.2012.9020. PMID: 22328361.
- Ostroff MD, Moureau N, Pittiruti M. Rapid Assessment of Vascular Exit Site and Tunneling Options (RAVESTO): A new decision tool in the management of the complex vascular access patients. J Vasc Access. 2021 Jul 21:11297298211034306. doi: 10.1177/11297298211034306. Epub ahead of print. PMID: 34289721.






