Infusion is a common practice across various hospital departments that carries risks for both patients and healthcare practitioners.
Since infusion is typically carried out progressively over the duration of a patient’s hospitalization, it often becomes increasingly complex due to the use of a large number of medical devices and administered drugs (including several with a Narrow Therapeutic Range or NTR).
Chemical reactions or mechanical behaviors (e.g., bolus effects) can occur between these drugs when multiple solutions with different flow rates are delivered simultaneously. This complexity can lead to errors in the management of infusion setups—errors that can frequently have fatal consequences for the patient (e.g., risk of air embolism or microbial contamination) and expose the practitioner to hazards (e.g., blood exposure).
In this article, we will discuss all the common errors, misuses, risks, and complications associated with infusions in intensive care.
Read on to learn how to better mitigate these risks and enhance the safety of your infusion practices.
Identifying Errors, Risks and Complications in Infusion in Intensive Care (ICU)
In intensive care (ICU), complex infusion setups pose numerous risks that can lead to clinical complications for the patient.
To prevent these issues, we have identified the common errors and misuses, their risks and complications, along with recommendations to avoid them:
Infusion lines not closed or protected at the proximal end:
This practice can lead to opening the system to air and micro-organisms, increasing the risk of air embolism and microbial contamination.
To avoid these high-risk situations, it’s essential to use bi-directional valves (needle-free connectors, needleless connectors) on the proximal ends of the devices available on the infusion line, such as stopcocks, ramps and extension lines. Not only does this protect healthcare personnel from needle-stick injuries, but it also safeguards patients from gas embolism and microbial infections. Thanks to the bi-directional valve, the infusion line is duly secured.
New device implementation:
Sometimes, we are requested to re-organize the infusion line set up to be agile. When adding devices such as stopcocks or ramps to the line, the circuit is opened to air and micro-organisms, which can result again in air embolism or microbial contamination.
Depending on how the patient’s clinical condition evolves, he or she may require an additional infusion, which is why a stopcock or ramp of stopcocks needs to be added to support this need. By doing this, the circuit is once again opened to air and micro-organisms, giving rise to a dual risk situation: risk of gas embolism and risk of microbial contamination.
To avoid opening the system during patient care, it is essential to assess in advance the devices that may be required before the line set-up. This is all the more important when the line is not fitted with closed-system bi-directional valves that allow the line to be handled in complete safety.
Succession of stopcocks:
The use of series of stopcocks can result in unforeseen disconnections, leading to the opening of the system and therefore to air embolism or microbial contamination.
To prevent this, avoid systematically assembling several three-way stopcocks in sequence and favour a ramp of stopcocks or a multi-lumen extension line with the necessary number of accesses.
Placement of several devices near the catheter:
Placing multiple stopcocks near the catheter can apply pressure, and pulling effect on the catheter, causing it to bend and potentially leading to treatment interruption or catheter dislodgement.
Adding an extension line at the proximal end of the catheter can move the derivation devices (stopcock, ramp) away from the insertion site, which can help get round this issue.
Infusion of incompatible drugs:
This can cause precipitates to form, obstructing the infusion line and decreasing or even stopping the infusion, which can have severe consequences on the clinical condition of the patient.
To avoid this problem, it is important to increase the number of infusion lines to prevent mixing incompatible medications, or at least to reduce the contact time between incompatible drugs. Refer to databases like Stabilis to better identify common physicochemical incompatibilities.
Pinching/Bending the PE extension line while opening the line:
Polyethylene is a material valued for its chemical inertness, which means that it can be in contact with the drug solution without any risk of interaction. It is also appreciated for its rigidity, which means that the extension tube can be kept intact even if it is subjected to pressure.
However, the rigidity of PE also presents a disadvantage, as the slightest pinch or kink can leave a mark. The line may even break if the kink is significant, such as when it is pinched to close the line (during device change or with an exhausted syringe), leading to complications such as gas embolism, microbial contamination, or medication underdosing.
To avoid these risky consequences, prefer the use of bidirectional valves to ensure the closure of the line at the moment of opening it instead of bending the extension line.
Catecholamines infusion on the same line as other therapeutics:
This can result in administering a vasoactive drug bolus to the patient due to the infusion of drugs with different flow rates, which causes a severe hemodynamic instability to the patient.
The best way to prevent bolus effect on the line is to dedicate a line for the infusion of catecholamines in order to isolate this class of high alert medication. If lines are limited, we recommend prioritizing medications like catecholamines and drugs with a Narrow Therapeutic Range (NTR).
Improper line flushing after drug, lipid or blood administration:
This can lead to line contamination. In the event of crystallization of perfusate residues, occlusion of the line may occur, causing acute complications such as CRBSI and Sepsis.
In this case, it is highly recommended to perform a 10 mL pulsed flush (3 to 10 pulses) after each drug, lipid or blood administration to clean the line properly.
Blood reflux:
There are many causes for catheter occlusion. This is often due to a difference between the administration pressure and the central venous pressure.
If the central venous pressure is higher than the pressure at which the solution is infused, a blood reflux can occur, causing occlusion of the distal end of the catheter by accumulation. This may be due to exhaustion of the infusion bag, a low flow rate from the KVO (Keep Vein Open) or the generation of a strong pressure by the patient (episodes of coughing, sneezing, vomiting, etc.).
There are other reasons for catheter occlusion, such as inadequate flushing, movement of the distal end of the catheter, and the patient’s clinical and physiological condition (e.g., Diabetes)
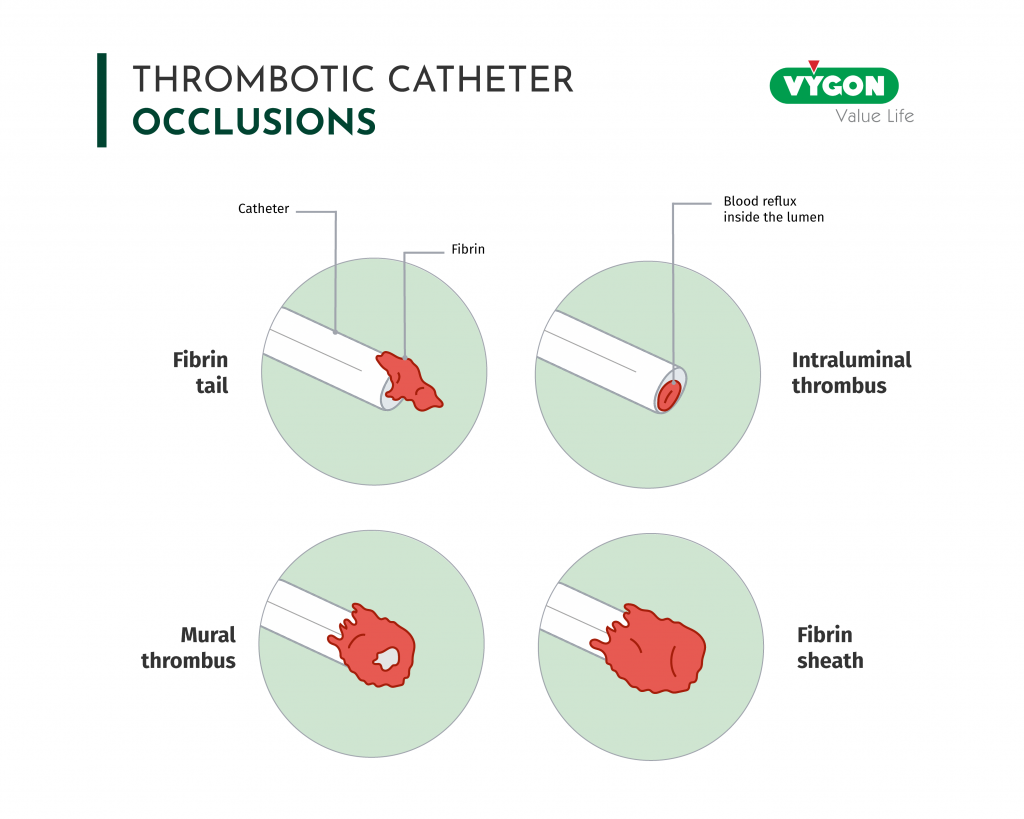
The catheter occlusion (intraluminal thrombus, mural thrombus, or fibrin sheath) leads to line obstruction, treatment interruption, or even to catheter removal.
To prevent occlusion, it is highly recommended to use neutral bidirectional valves with flow control function (anti-reflux).
Incorrect identification of the line:
The lack of identification of lines makes it difficult to identify administered solutions, especially during alert situations. This can increase the risk of error and therefore increase the probability of administering the therapeutic on the wrong way, giving birth to clinical instability of the patient.
It is recommended to properly identify administrated drugs essentially through labeling on bags, syringe pumps, and extension lines (next to the patient) with appropriate color codes to recognize the type of medication.
>> ACCESS THE ERRORS-RISKS-COMPLICATIONS-RECOMMENDATIONS POSTERS HERE <<
Golden Rules for Optimal Infusion in Intensive Care:
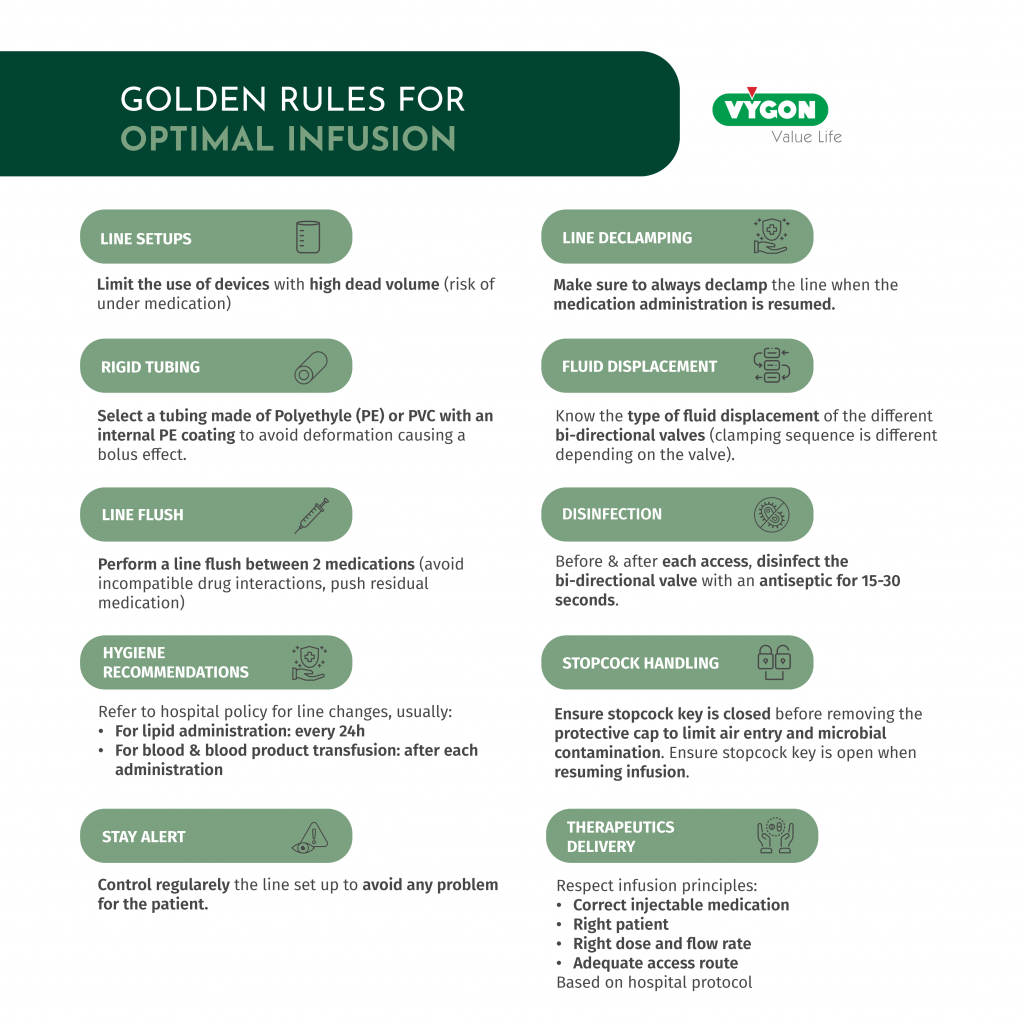
Infusion is therefore a complex practice during which the user must make the right choices to ensure the delivery of therapeutics to the patient in accordance with the medical prescription.
The ideal setup does indeed not exist, but it can be optimized by following basic rules for successful infusion management.
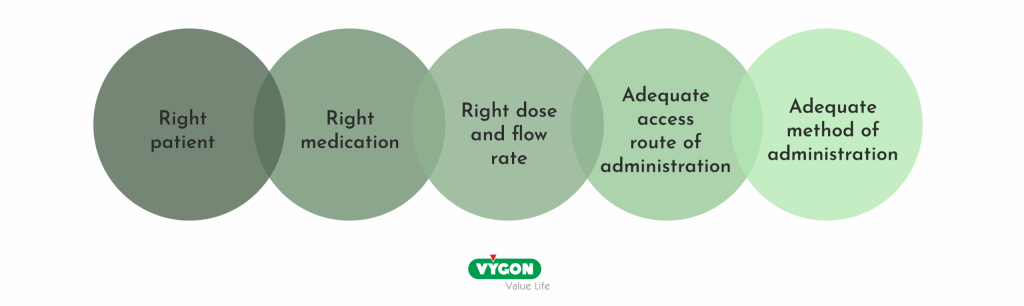
The selection of the appropriate access route, infusion of the correct medication with proper administration methods, and the choice of devices must be done in accordance with the recommendations of relevant medical societies. Additionally, it is essential to understand the advantages and limitations of these devices and to regularly check the setups.
This will contribute to the proper execution of the infusion procedure with the ultimate goal of ensuring patient’s therapeutic safety.
For the latest insights, updates, and expert tips in Vascular Access, follow our Instagram!
Bibliography
- Gorski, Lisa A., et al. “Infusion Therapy Standards of Practice, 8th Edition”. Journal of Infusion Nursing, vol. 44, no. 1S, January 2021, p. S1224. DOI.org (Crossref), https://doi.org/10.1097/NAN.0000000000000396.
- Bonnes pratiques de Perfusion en Anesthésie-Réanimation : des abords vasculaires aux montages de perfusion – Lucie Germon, Aurélie Bros, Perrine Drancourt, Stéphanie Genay, Delphine Cabelguenne.
- https://www.cathflo.com/catheter-management/types-catheter-occlusions.html







