Have you ever wondered how nursing works outside of your country? What protocols are used, how is the coordination between professionals, and how is patient follow-up conducted?
Christian Dupont is a nurse at one of the major hospital centers in the French capital, Cochin Hospital, and has extensive experience. As the president of GIFAV (Francophone Interdisciplinary Group for Vascular Access) and a member of the WoCoVA committee, Christian has been dedicated to vascular access for many years and is heavily involved in training in this field.
During the WoCoVA congress, Christian Dupont answered our questions and told us about his current work and his perspective on vascular access from both a national and international standpoint.
Could you please explain what your job entails?
I am a patient journey nurse, which is a special position that involves coordinating all the care that a patient in my department may need. I work in pulmonology, and the type of patients I follow are those with cystic fibrosis or respiratory infectious diseases. To be more precise, my duties include:
- Organizing home care as prescribed by the doctors.
- To do this, I liaise with home care nurses, pharmacies, healthcare suppliers, and laboratories (for monitoring treatment through blood tests).
One of my responsibilities is to suggest the best possible vascular access for each patient. The catheters used in the unit are:
- Short peripheral catheters
- Ports
- PICCs (Peripherally Inserted Central Catheters)
- Midlines (although they are not widely used due to lack of reimbursement from social security).
We also have to support the patient through phone calls to check if the antibiotic treatment is effective.
Management of complications in vascular access
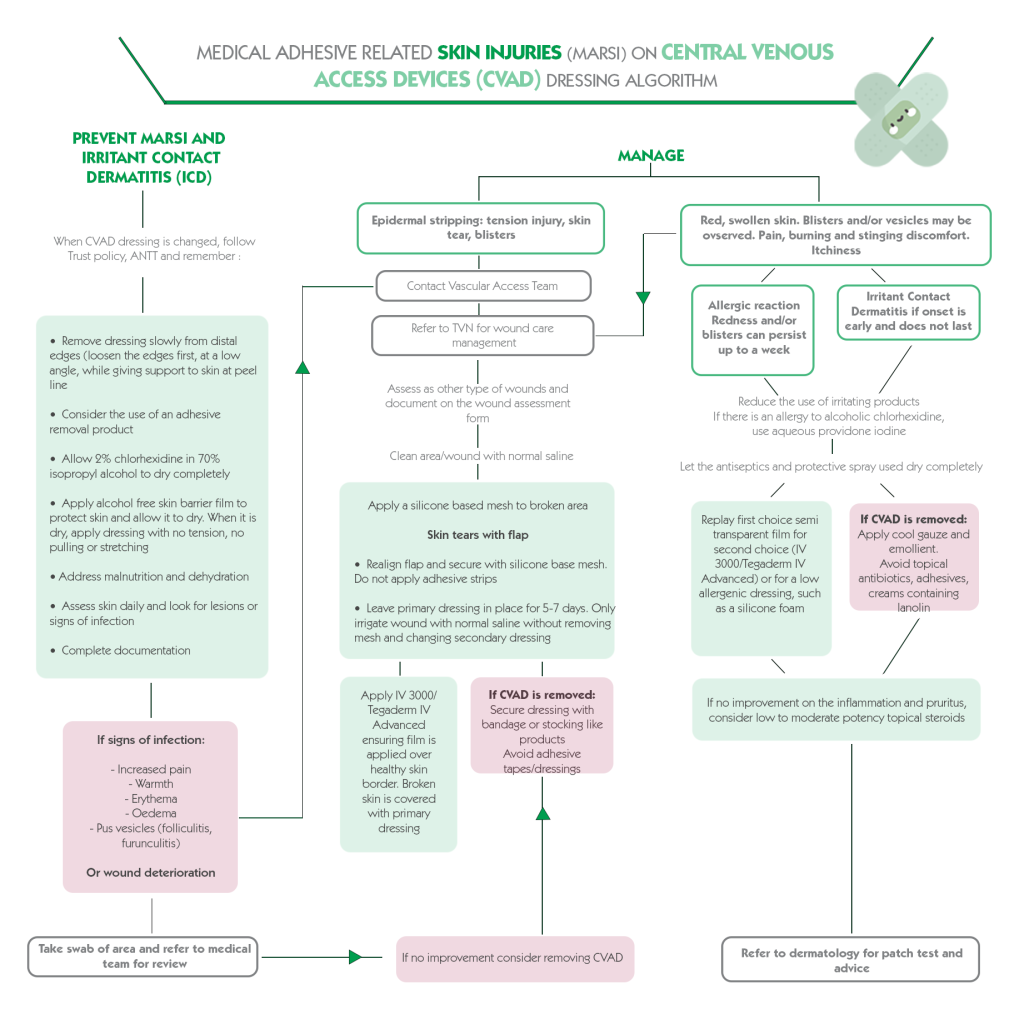
The most common complication is occlusion. For central lines, a fibrinolytic injection is usually prescribed. We check for the absence of infection, thrombosis, and MARSI (catheter-related skin injuries).
In France, PICCs cannot be removed at home, so we schedule patients for removal at the hospital’s outpatient clinic. The removal is performed by nurses.
Vascular access training
We cover both home care and in-hospital aspects of vascular access handling.
To do this, we first conduct an audit to assess the level and the number of professionals to be trained based on the size of the department. For example, training an entire 3-floor operating room department may take up to 12 hours to ensure everyone is adequately trained, whereas a replacement team at a centre may only take a morning, depending on the size.
Training is conducted annually and serves as more of a knowledge update for professionals already in practice. Additionally, we provide training at universities 1 to 2 times a year.
Research
In our hospital, we conduct prospective studies. During a period when we were not very familiar with PICCs, we tracked 182 PICCs from insertion to removal. We will likely do the same for midlines.
We have also conducted knowledge audits on ports and antiseptics. Antiseptics, in general, are a less-studied topic, perhaps because they are often influenced by habits, and the world of vascular access is generally more focused on device insertion.
You dedicate a lot of your time to training nurses. What is the main reason for training healthcare professionals?
As I age, one day, they will be the ones taking care of me, so I have to train them! The biggest interest in teaching in both initial and ongoing education is that it forces us to:
- Gain perspective on our practice.
- Conduct literature searches.
- Learn to break away from our habits, particularly during interactions with students.
Sometimes, we don’t ask the right questions about our practices; we stop questioning things, and it’s essential to remember that training is of no interest to both the audience and the trainer if the needs of the students are not considered beforehand.
For example, during a training on removing Huber needles that I gave in Uganda, I realized that we are so focused on technicalities that we forget what truly matters in care. And what truly matters is not as complicated as it may seem. It’s important not to make something more complex than it is in its basic form just to showcase expertise as an instructor.
How do you handle confrontation with professionals when you question their expertise in teaching good practices?
I like to evaluate the service’s practices first through an audit. Sometimes, I go to the service when they have a good number of patients, and I go from room to room taking photos of vascular access. Afterwards, we discuss the practices with the nurses.
We do the same when we have to test new devices: photos of the current device and photos after. I believe involving them in this process to try to improve their daily routine and asking for their opinion is important.
You work in France and have a broad international perspective on care, as you preside over the GIFAV and participate in the WoCoVA: what do you think of the vascular access culture among nurses in general? And among doctors?
In France, there is a great awareness of implantable ports. This is due to 100% reimbursement by social security for this type of devices. So, we haven’t asked ourselves the same questions as in the US, where most of the time, you have to pay for the implantation of vascular access devices. This is why PICCs are often used there.
However, there is a tendency to think that they do it better outside of France. But if we look at the latest studies on infections in intensive care, the results are very good. So, nursing in France works well. They are usually interested in practices carried out abroad.
Doctors are not very involved in the decision regarding the patient’s vascular access.
Is this context difficult for patients?
Imagine that you’ve just been diagnosed with cancer. The first doctor you see is the oncologist who delivers the diagnosis. Then, you have to visit the “announcing nurse” (as they are called in France), who explains the journey you will go through (which likely includes numerous examinations, tests, and lab work). Finally, you’re admitted to the hospital. In this context, it’s crucial to be well-coordinated because if it’s not the case, it can be an extremely anxiety-inducing situation for the patient.
However, one thing to consider is that in the past, nurses provided comprehensive patient care. But with the introduction of the 35-hour workweek several years ago, they can’t follow the patient all the way through. They have to work on multiple units, which can be challenging for them.
That’s why the position of the patient journey nurse was created to maintain this follow-up from the beginning to the end of treatment. There are also advanced practice nurses and coordination nurses. Gradually, nursing is moving in a direction similar to medicine, segmenting patient care, somewhat like in the United States.
If we continue in this direction, there will be a basic nurse and then several nurses with different roles. This approach can lead to a loss of holistic patient management, which is what patients really need.
The PICC-Port is gaining more prominence. What do you think about this device compared to a chest port?
It is a vascular access device that can provide an excellent alternative for certain types of patients. To understand the context, let’s take the example of lung cancer patients. In such cases, life expectancy is often compromised to a significant extent, so aesthetics are generally not a top concern for the patient. They readily accept a chest port.
However, for patients with conditions like cystic fibrosis, particularly young patients, the visibility of the device is a problem. Body image is important, and having a visible device:
- Can hinder their social interactions because it means they have to explain their illness when others see it.
- Constantly reminds them of their disease.
In this regard, a PICC-Port is more discreet and can even be mistaken for a closed-loop glucose control system.