This article discusses the implementation of electrocardiogram tip location (ECG TLS) for the confirmation of central venous catheter tip position.
The author works within a nurse led vascular access service in NHS Scotland and has found that this method of catheter tip confirmation allows greater accuracy when compared to radiography.
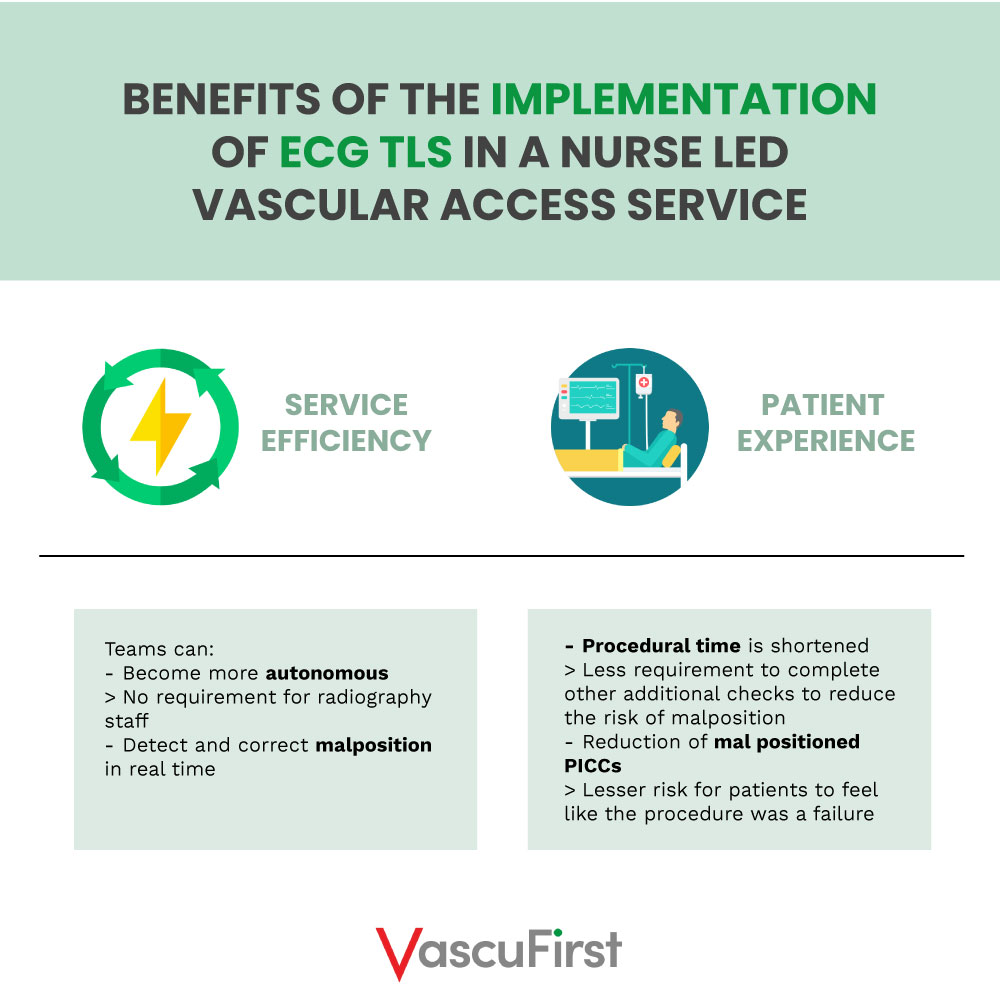
Furthermore, the implementation of ECG TLS has improved the efficiency of the service, has had a positive impact on patient experience, and is a safe alternative to radiography.
1. Background: catheter tip location methods
To reduce post procedure complications, it is essential that the tip of a CVC is positioned accurately. In fact, the distal end, or tip of the device should terminate within the lower third of the superior vena cava (SVC), at cavo-atrial junction, or within the upper right atrium1, 2.
A tip that is positioned too high can increase the risk of complications such as persistent withdrawal occlusion or thrombus. If it is too low, it can increase the risk of arrhythmia or cardiac tamponade3.
In this part, we will focus on two methods that can be used to determine catheter tip position: radiography, either plain film chest radiography (CXR) or fluoroscopy, and electrocardiogram (ECG) guidance4.
-
Radiography
Radiography has been the most frequently used method for tip confirmation but can present many challenges. Specific challenges are delays in obtaining, interpreting, and reporting radiography5,6.
For patients who require CVC insertion in a non-clinical environment, there can be delays in accessing a radiography appointment. This can have a real time impact on the patient’s treatment as the CVC cannot be accessed until the catheter tip has been determined, which can result in delays to treatment.
While chest landmarks can vary between patients, body habitus and patient rotation can distort the image and external equipment can obscure anatomy, resulting in misinterpretation7,8. Despite troubleshooting, the use of post procedure CXR can confirm catheter tip mal position.
When it is confirmed, manipulation of the catheter may be required. This will delay the use of the CVC, impacting service efficiency, patient treatment and experience.
Furthermore, exposure to radiography emits harmful ionising radiation which can increase the long-term risk of cancer9,10. Guidelines inform us that the use of radiography should be justified, and the potential benefits of the exposure should outweigh the risks10.
Although there is no limit to the number of radiography exams a person can have, it is recognised that repeated exposure can result in cumulative doses and an increase in associated risk to health11. Therefore, if there is an alternative method, that does not involve exposure to ionising radiation, this should be considered12. Despite this, radiographic CVC confirmation is still the mainstay, likely due to these procedures still falling within the remit of Interventional Radiology4.
-
Electrocardiogram tip location systems
ECG TLS allows the inserter to observe changes in the electrical activity of the heart, focusing on the patient’s P wave as the catheter tip is advanced through the superior vena cava, cavoatrial junction and into right atrium. This allows the inserter to accurately position the catheter tip within the optimal range13.
Often referred to as ECG tracking, the inserter can detect and correct any error in CVC placement and confirm correct tip positioning in real time, removing the need for CXR in most patients14.
2. Organisation of our vascular access service (VAS)
As the Senior Charge Nurse of a busy nurse led vascular access service (VAS), I have experienced first-hand the challenges faced by health care workers to establish reliable vascular access that meets their patient’s treatment requirements.
Our VAS accepts referrals from all specialities within our health board and as part of regional services, receiving approximately 7000 referrals per year. Decision making around which vascular access device (VAD) a patient receives is multifactorial and includes the patient’s vascular access requirements, their vessel health, and previous vascular access history.
Patient safety, experience and service efficiency is paramount, and to achieve this, it is essential that we keep informed of the ever-evolving literature base and new technologies which can enhance the service that we provide.
Our VAS has dedicated sessions within clinical areas at three acute hospital sites and we also provide a mobile service inserting VADs at the patient’s bedside. The mobile service benefits those patients whose condition could be compromised by transferring between hospitals, departments, and wards, such as patients with complex or unstable clinical situations15. This service is provided within ambulatory care hospitals, mental health facilities and hospices.
Prior to implementing ECG TLS, decision making for patients requiring our mobile service was challenging and often, there was a requirement to insert suboptimal VADs due to the lack of availability of radiography. This was our main indication for trialling ECG TLS.
3. Introduction of ECG TLS in our hospital
Our VAS is part of the wider Interventional Radiology team and therefore, the use of radiography was well established. However, we are a progressive team and were keen to change the status quo if it would benefit our patients and service.
In order to enhance our practices, we chose to try then implement ECG. This transformative shift was accomplished through a series of steps:
-
Team training
A date was arranged for one of the manufacturers of ECG TLS to have a representative attend one of our clinical lists to demonstrate the device.
Following the demonstration, we allocated a morning PICC insertion list to use the ECG for the insertion of PICCs in conjunction with post procedure CXR. Unfortunately, this was an unsuccessful day, and resulted in a lack of confidence in the system. We only had 50% success with the system. One patient’s PICC tip was found to be mal positioned into their internal jugular vein on post procedure CXR.
Following this, we requested that further training be facilitated by a clinician who had hands on experience and knowledge of the device. Two further training sessions were organised when an appropriate trainer was available, and this proved invaluable. These sessions concentrating solely on the functionality of the system and provided with useful troubleshooting techniques and real-life insights.
The team’s confidence in the use of the ECG TLS improved and I was keen to introduce the system into our clinical practice.
-
Implementation of ECG
The implementation of ECG would be a change in our practice. I was required to apply for permission to trial the equipment in the first instance. Once approved, a four-week period at one of our clinical sites was allocated for the trial, during which the manufacturer provided us with one system. We continued to use post procedure CXR along with the ECG during the trial to ensure that we were interpreting the device correctly.
In the trial period, we inserted a total of 72 PICCs using ECG in conjunction with CXR for the catheter tip confirmation of 59 insertions. 10 of the 72 patients requiring PICC insertion attended our clinical area whilst the ECG TLS was being utilised for bedside PICC placements. A further three patients had cardiac pacemakers which precluded the use of ECG TLS. For all 59 PICCs that ECG was used for, insertion was straightforward, and the inserter was confident that catheter tip was within the optimal range. This was confirmed on post procedure CXR.
On completion of the trial period, this data was presented and discussed with our diagnostic management team.
Post trial, it was agreed that the VAS would procure an ECG TLS for our three main sites.
-
Encountered challenges in the implementation of ECG
Radiography was an ingrained part of the standard operating procedure for PICC tip insertion and confirmation. Despite completing procedural documentation and issuing a post procedure electronic report stating that satisfactory tip position had been confirmed using the ECG tip location system, many referrers continued to look for a post procedure CXR. In some instances, they even requested a CXR, exposing the patient to unnecessary radiation.
Reconditioning and educating our service users was a significant challenge. Some specialities were quick to adapt, whilst others, particularly those specialities who had historically made a high volume of referrals for VADs, required more time and education.
One challenge we encounter when utilising ECG involves patients lacking a P wave or those with a cardiac pacemaker exhibiting a paced rhythm. In such instances, the device fails to detect P wave changes, rendering it unusable. However, increasingly, ECG has additional functionalities that in some cases, can be suitable for patients who do not have a P wave. These allow the inserted to focus on changes in the F wave16.
Our ECG tip location systems are portable allowing us to use them at multiple locations across various care settings. Although this is an advantage of the system, movement between care settings along with extremely busy patient lists can result in wear and tear. We do require technical advice and support from the manufacturer.
We have also been required to return the device for maintenance when troubleshooting has been unsuccessful. This can result in the requirement to revert to post procedure CXR.
-
The benefits of the implementation of ECG:
> Service efficiency
The ECG tip location system has improved the efficiency of our service. In most cases, it allows us to be autonomous practitioners, with no additional requirement for radiography staff.
We can detect and correct mal position in real time. Previously, mal position would have only been detected on post procedure chest CXR, resulting in the patient having to undergo another procedure to correct the catheter tip position.
Negating the requirement for CXR for these patients allows appointment to be accessed for other referrals which has a positive impact on the efficiency of x-ray lists.
> Patient experience
Procedural time is shortened with less requirement to complete other additional checks to reduce the risk of malposition. This has had a positive impact on patient experience and reduces potential anxiety whilst waiting for CXR confirmation.
In fact, due to the ECG TLS allowing the inserter to detect and correct malposition in real time, we have seen a reduction in mal positioned PICCs. Previously, we would not have known that there was a catheter tip malposition until following post procedure CXR. There was then the requirement to bring the patient back into the clinical area for manipulation of their PICC. Even though malposition is a recognised risk of PICC insertion and is discussed during the consent conversation, patients can feel like the procedure has been a failure if it happens. This can reduce confidence in the device and result in the patient being reluctant to consent to VAD insertion in the future.
Conclusion
ECG TLS is gaining popularity, particularly with the increase in specialist vascular access services. Our VAS have used the device for over two years and the implementation has proven beneficial to our service and our service users.
In summary, ECG TLS is now well established within our service and has proven an accurate, safe, and efficient method of catheter tip confirmation.