The PERSEUS guidelines, recently released by the European Society of Anaesthesiology and Intensive Care (ESAIC), recommend a global use of ultrasound to assist all steps of central venous catheterization in order to minimize all immediate, early, and late complications. However, some barriers for such a global use of ultrasound still exist1.
The new wireless ultrasound technology applied to the field of vascular access may allow to overcome barriers to the global use of ultrasound by increasing easiness in performing the maneuver due to the absence of a cable. Furthermore, since wireless transducers can easily be wrapped up into a sterile cover, adoption of wireless systems may avoid accidental contaminations, improving maximal barrier precautions and increasing safety as well.
Point-of-care Ultrasonography
Point-of-care ultrasonography (POCUS) consists in the ultrasonographic image acquisition and its immediate interpretation, performed by the same, properly trained, healthcare professional, whether at patient’s bedside, in the field or during transport2,3.
With the development of smaller ultrasound devices first, and handheld wireless probes recently, POCUS has been spread and implemented in different clinical settings for all steps of patient’s care.
As a guide for invasive procedures, POCUS has been associated to reduced complications and improved safety4,5.
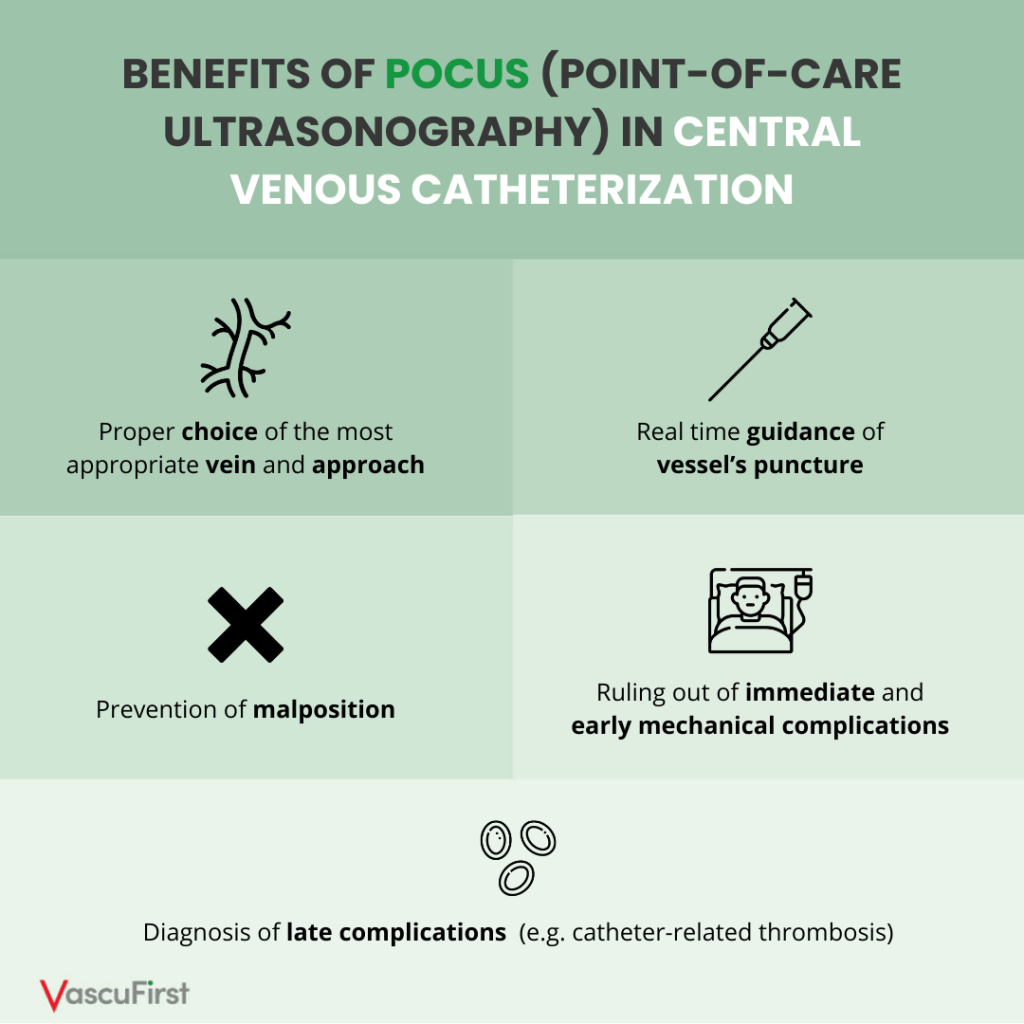
With regard to the field of central venous catheterization, POCUS is recommended to assist all steps of the procedure, either for placement or management:
Ultrasound in the field of vascular access: history, evidence, guidelines
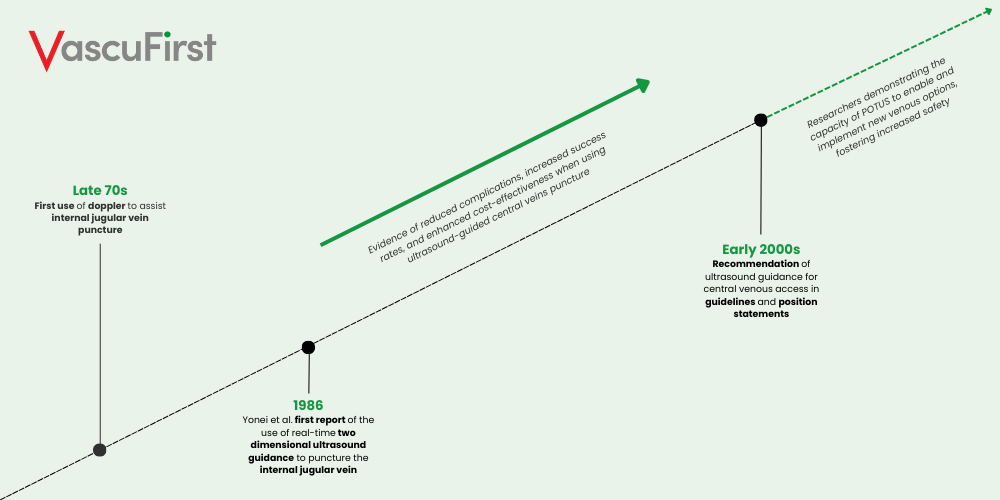 Image: Timeline of the history of Ultrasound in Vascular Access
Image: Timeline of the history of Ultrasound in Vascular Access
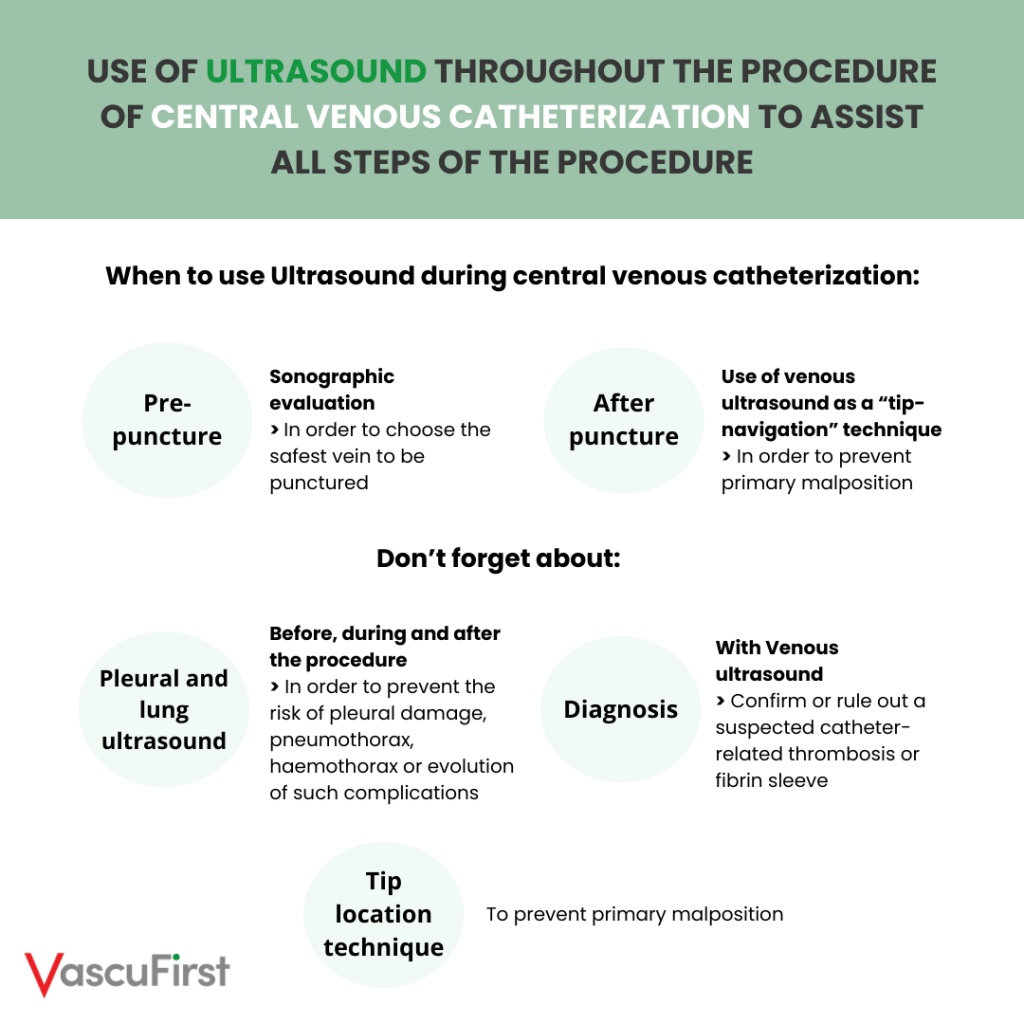
ERSEUS guidelines, recently released from the European Society of Anaesthesiology and Intensive Care (ESAIC), recommend a global use of ultrasound throughout the procedure of central venous catheterization, to assist all steps of the procedure1. The preliminary sonographic evaluation is recommended to choose the side and the safest vein to be punctured, weighing the risks and benefits of infectious and noninfectious complications. Pre-puncture sonographic examination should include evaluation of vein’s depth and diameters1. To enhance the compatibility between the catheter’s outer diameter and the vein’s inner diameter and reduce the risk of catheter-related thrombosis, a 1:30 ratio is recommended. The ultrasound-guided puncture is considered safe only if the needle tip is visualized in real-time while entering the vein1.
After puncture, venous ultrasound may play a significant role in the prevention of primary malposition1. Being utilized as a sort of ‘tip navigation’ technique, sonographic imaging allows to visualize wires and catheters travelling towards the cavo-atrial junction by its visualization throughout the ipsilateral brachiocephalic vein also ruling out a possible misdirection to other veins. Transthoracic echocardiography is utilized, today, as an ultrasound-based ‘tip location’ technique, allowing direct or indirect visualization of the catheter’s tip, being effective in preventing primary malposition and confirming or ruling out a suspected late malposition of the catheter. Pleural and lung ultrasound should be performed before, during and after the procedure of central venous catheterization1. Before the procedure, the pleura should be visualized so to choose the safest vein to be punctured considering the possible risk of pleural damage. After all difficult punctures potentially associated with pleural injury, lung ultrasound should be performed to exclude pneumothorax or haemothorax and, if detected, to monitor the evolution of such complications. Venous ultrasound is recommended as the first-level diagnostic technique to confirm or rule out a suspected catheter-related thrombosis, also allowing differential diagnosis with fibrin sleeve, thus playing a significant role in the management of late complications1.
As ultrasound has become, today, the standard of care in the field of vascular access, portable devices, such as handheld ultrasound machines and wireless probes, are gaining increasing popularity due to their small size and easy functionality allowing to quickly acquire imaging at the point of care.
Handheld wireless ultrasound at the point of care
A handheld wireless ultrasound machine is a portable ultrasound device consisting of a probe that can connect to a mobile device, with no need of a cord, to provide clinicians with real-time images at the point of care18.
Image: Wireless linear transducer. On the device depicted in this figure there are controls built-in allowing the main ultrasonographic functions (e.g., gain, depth, freeze, etc.) to be operated directly on it.
The probe is connected to a smart device by Bluetooth or by a Wi-Fi field created by the probe itself. The images are sent to smartphones, or tablets equipped with a specific app. Wireless ultrasound probes tend to be compact and small enough to fit in a pocket so to be used anywhere, whether at patient’s bedside, in the field or during emergency transports.
In the last decade, the quality of wireless ultrasound devices has gradually begun to improve. They are now a very good option for rapid assessment of acute conditions requiring immediate intervention at the point of care or for guidance of simple interventional procedures18,19.
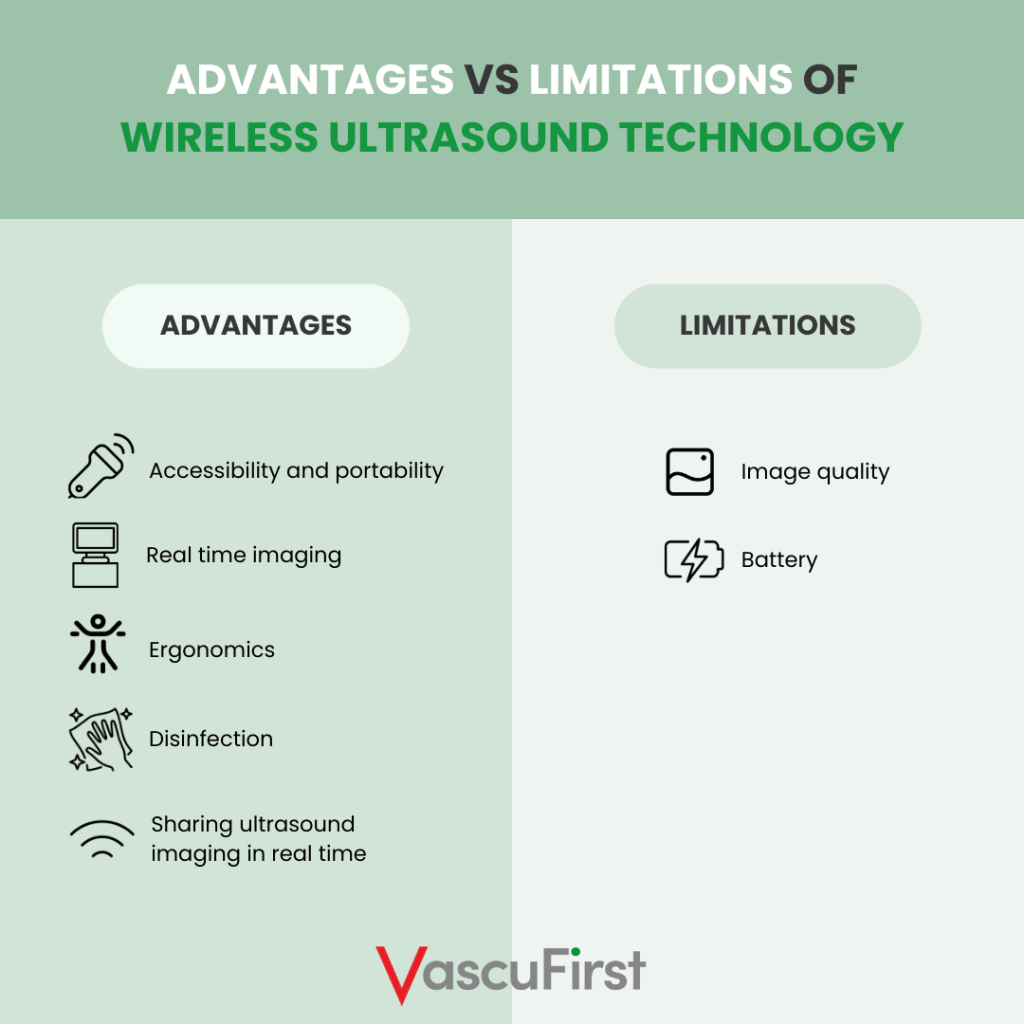
General advantages of wireless ultrasound technology
- Accessibility and Portability. Wireless ultrasound devices can be used with patients anywhere, whether at bedside, in the field or during emergency transports, even on a helicopter. Images are saved directly onto provider’s smartphone or tablet, easy to be uploaded and reviewed.
- Real-time imaging. Wireless ultrasound devices allow a rapid assessment by providing clinicians with real-time, quality images that may be crucial for diagnosis. This is especially beneficial in emergency conditions and critical care settings, where clinicians need to image patients quickly, allowing to perform E-FAST exam (Extended Focused Assessment with Sonography for Trauma), lungs evaluation, RUSH exam (Rapid Ultrasound for Shock and Hypotension) and also, enabling to assess many other acute conditions requiring immediate intervention, as well as to guide interventional procedures such as central venous catheterization.
- Ergonomics. Using wireless ultrasound systems, clinicians can easily scan with one hand and no need to deal with a wire or to move in a tight space between the patient and the ultrasound machine, providing more comfort in any environment, such as the emergency room, the field, or the intensive care unit.
- Disinfection. Wireless ultrasound devices are easy to disinfect since they’re small and without wires. Furthermore, a key advantage of wireless systems over larger ultrasound devices is that wireless ones can more easily be wrapped up into a sterile cover during their use, significantly reducing risks of cross-contamination and spread of infectious diseases18.
- Sharing Ultrasound Imaging in Real-Time. A few wireless ultrasound devices using Wi-Fi technology allow to share imaging across multiple smart devices in real-time. This function may be advantageous both for teaching purposes and infection control situations.
General limitations of wireless ultrasound technology
- Image Quality. Wireless ultrasound devices currently available do not provide the same image quality as traditional ultrasound systems with wires. Even if a qualitative focused cardiac assessment can be performed with wireless ultrasound devices as well, advanced quantitative applications are still lacking. In fact, only few current devices provide doppler trace or comprehensive measurement options, thus making wireless systems still not well suitable for quantitative applications18.
- Batteries. Wireless ultrasound devices typically run on rechargeable batteries which may not last as needed, depending on usage. Devices with rechargeable and removeable batteries are ideal, allowing to use additional batteries for back-up power, eliminating or reducing the down time. However, only few devices have rechargeable, removeable batteries which may take up to 90 minutes to recharge.
However, even if still affected by some limitations, wireless ultrasound is a promising technology with many already concrete advantages and continuous ongoing advancements, especially in the field of vascular access.
Handheld wireless ultrasound for placement of vascular access device
Researchers have found that wireless ultrasound technology applied to the field of vascular access devices placement may further increase safety as well as allow to overcome barriers to the use of ultrasound guidance. In fact, the increased easiness in performing ultrasound-guided manoeuvres due to the absence of the cable may facilitate a more widespread daily use of ultrasound guidance itself20-22.
In the field of vascular access, the key advantage of wireless systems over larger ultrasound devices is that wireless ones can more easily be wrapped up into a sterile cover so to perform the procedure with maximal barrier precautions.
Image: Wireless ultrasound devices can be easily wrapped-up in a sterile cover and placed on the sterile tray without dealing with a cord which may disrupt maximal barrier precautions.
Few devices, allow the main functions such as gain, depth, freeze, etc, to be operated either by controls built-in on the transducer or directly on the screen of the smart device, which, in turn, can be wrapped up into a sterile sheath in order to operate the above listed main functions by maintaining maximal barrier precautions.
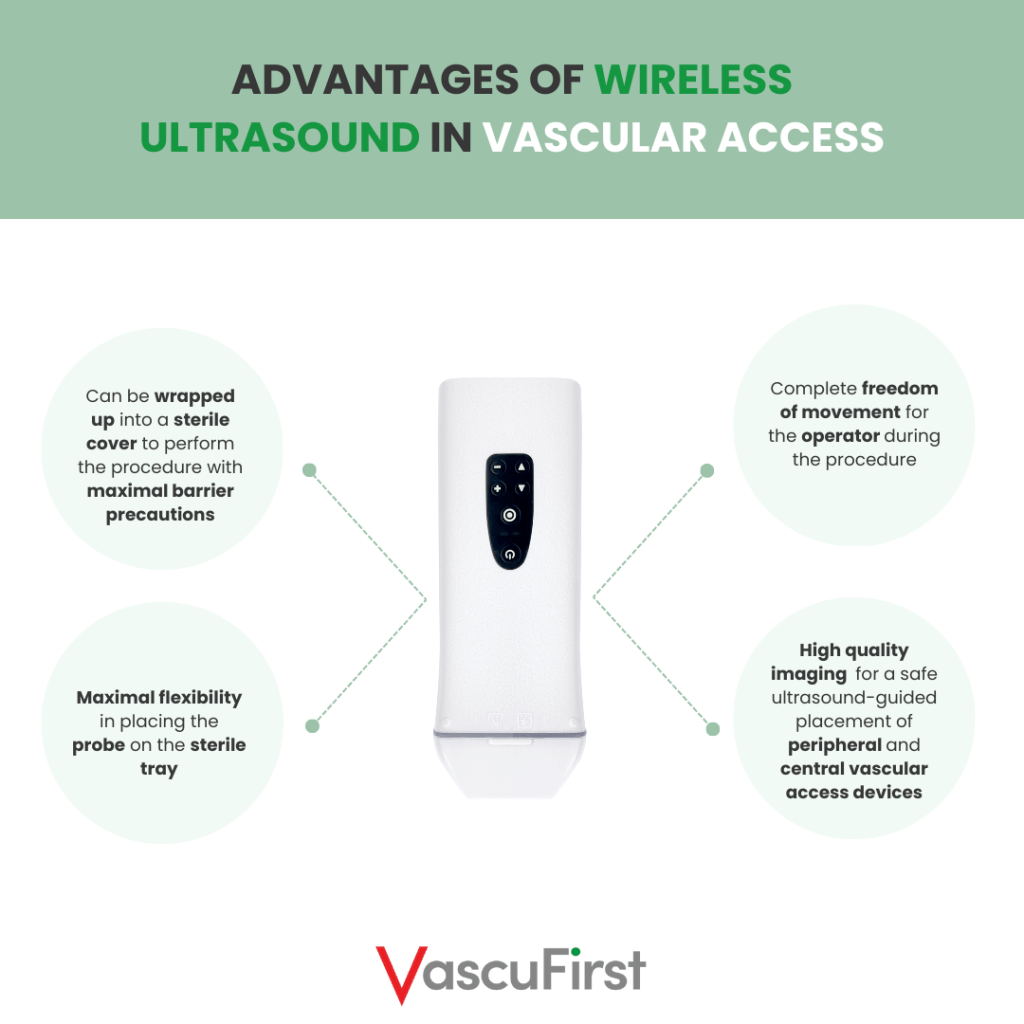
Further advantages include: (a) maximal flexibility in placing the probe on the sterile tray, as the connection is wireless; (b) complete freedom of movement for the operator during the procedure, as most wireless probes are easy to handle. Furthermore, most currently available wireless ultrasound devices allow to obtain a high-quality vascular imaging in order to perform a safe ultrasound-guided placement of peripheral and central vascular access devices. Also, visualizations of needle tip, guidewires, introducers, and catheters are very nice in quality.
The same wireless linear transducer can be used for sonographic detection of potential misplacement of guidewires and/or catheters, as well as for ruling out pneumothorax or haemothorax. Wireless convex or microconvex transducers can be used, instead, for direct or indirect visualization of the catheter’s tip. For all these purposes, wireless ultrasound devices have been developed consisting in a two-headed probe: on one head, a linear transducer for ultrasound-guided puncture and for confirming the right direction of wires and catheters; on the other head, a convex transducer for ruling-out complications and for enabling sonographic-based catheter’s tip location.
In the field of ultrasound-guidance for vascular access placement, the advantages of wireless ultrasound technology overcome its limitations when compared to diagnostic applications. Wireless probes and the mobile apps supporting them are constantly improving, continuing to progress in terms of image quality, versatility, and ergonomics. Many advancements are yet to come, including artificial intelligence which might help to enhance this technology allowing to further improve patients’ outcomes reducing, immediate, early, and late complications.
References
- Lamperti M, Biasucci DG, Disma N, Pittiruti M, Breschan C, Vailati D et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur J Anaesthesiol. 2020 May;37(5):344-376. doi: 10.1097/EJA.0000000000001180. Erratum in: Eur J Anaesthesiol. 2020 Jul;37(7):623
- Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-Care Ultrasonography. N Engl J Med. 2021 Oct 21;385(17):1593-1602. doi: 10.1056/NEJMra1916062
- Heldeweg MLA, Lopez Matta JE, Pisani L, Slot S, Haaksma ME, Smit JM et al. The Impact of Thoracic Ultrasound on Clinical Management of Critically Ill Patients (UltraMan): An International Prospective Observational Study. Crit Care Med. 2023 Mar 1;51(3):357-364. doi: 10.1097/CCM.0000000000005760
- Biasucci DG. Ultrasound based innovations for interventional procedures: the paradigmatic case of central venous access. Minerva Anestesiol. 2020 Feb;86(2):121-123. doi: 10.23736/S0375-9393.19.14070-9
- Mcgahan JP. The history of interventional ultrasound. J Ultrasound Med 2004;23:727-4. doi: 10.7863/jum.2004.23.6.727
- Biasucci DG, La Greca A, Scoppettuolo G, Pittiruti M. What’s new in the field of vascular access? Towards a global use of ultrasound. Intensive Care Med. 2015 Apr;41(4):731-3. doi: 10.1007/s00134-015-3728-y
- Ullman JI, Stoelting RK. Internal jugular vein location with the ultrasound Doppler blood flow detector. Anesth Analg. 1978 Jan-Feb;57(1):118. doi: 10.1213/00000539-197801000-00024
- Yonei A, Nonoue T, Sari A. Real-time ultrasonic guidance for percutaneous puncture of the internal jugular vein. Anesthesiology. 1986 Jun;64(6):830-1. doi: 10.1097/00000542-198606000-00033
- Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996 Dec;24(12):2053-8. doi: 10.1097/00003246-199612000-00020
- Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A. The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technol Assess. 2003;7(12):1-84. doi: 10.3310/hta7120
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015 Jan 9;1(1):CD006962. doi: 10.1002/14651858.CD006962
- Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015 Jan 9;1(1):CD011447. doi: 10.1002/14651858.CD011447
- National institute for clinical excellence. NICE Technology appraisal guidance No 49: Guidance on the use of ultrasound locating devices for placing central venous catheters. London: Nice; 2002.
- Breschan C, Platzer M, Jost R, Stettner H, Beyer AS, Feigl G, Likar R. Consecutive, prospective case series of a new method for ultrasound-guided supraclavicular approach to the brachiocephalic vein in children. Br J Anaesth. 2011 May;106(5):732-7. doi: 10.1093/bja/aer031
- Brescia F, Biasucci DG, Fabiani F, Favarato M, Costa F, Longo F et al. A novel ultrasound-guided approach to the axillary vein: Oblique-axis view combined with in-plane puncture. J Vasc Access. 2019 Nov;20(6):763-768. doi: 10.1177/1129729819826034
- O’Grady NP. Prevention of Central Line-Associated Bloodstream Infections. N Engl J Med. 2023 Sep 21;389(12):1121-1131. doi: 10.1056/NEJMra2213296
- Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A et al; 3SITES Study Group. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015 Sep 24;373(13):1220-9. doi: 10.1056/NEJMoa1500964
- Malik AN, Rowland J, Haber BD, Thom S, Jackson B, Volk B, Ehrman RR. The Use of Handheld Ultrasound Devices in Emergency Medicine. Curr Emerg Hosp Med Rep. 2021;9(3):73-81. doi: 10.1007/s40138-021-00229-6
- Ossola C, Piacentino F, Fontana F, Curti M, Zorzetto G, Coppola A et al. Pocket-sized, wireless-Bluetooth ultrasound system to perform diagnostic and low-complexity interventional procedures in bedridden patients during the COVID-19 pandemic: from intensive care unit to domiciliary service? Eur Radiol Exp. 2022 May 10;6(1):20. doi: 10.1186/s41747-022-00273-1
- Franco E, Rodriguez Muñoz D, Matía R, Hernandez-Madrid A, Carbonell San Román A, Sánchez I, et al. Wireless Ultrasound-Guided Axillary Vein Cannulation for the Implantation of Cardiovascular Implantable Electric Devices. J Cardiovasc Electrophysiol. 2016 Apr;27(4):482-7. doi: 10.1111/jce.12917
- Rodríguez Muñoz D, Franco Díez E, Moreno J, Lumia G, Carbonell San Román A, Segura De La Cal T, Matía Francés R, Hernández Madrid A, Zamorano Gómez JL. Wireless Ultrasound Guidance for Femoral Venous Cannulation in Electrophysiology: Impact on Safety, Efficacy, and Procedural Delay. Pacing Clin Electrophysiol. 2015 Sep;38(9):1058-65. doi: 10.1111/pace.12670
- Rodríguez Muñoz D, del Val Martin D, Fernández Santos S, Segura de la Cal T, Carbonell San Román A, Moreno Planas J, Zamorano Gómez JL. Use of a new wireless transducer for femoral venous vascular cannulation. J Clin Ultrasound. 2015 Feb;43(2):118-9. doi: 10.1002/jcu.22255






