We are currently witnessing an increase in the use of therapeutic apheresis (TA) with indications not only in oncohaematology, but also in nephrology, cardiology, dermatology, gastroenterology, rheumatology, neurology, metabolic diseases… The list of diseases with treatments that include TA goes on and on.
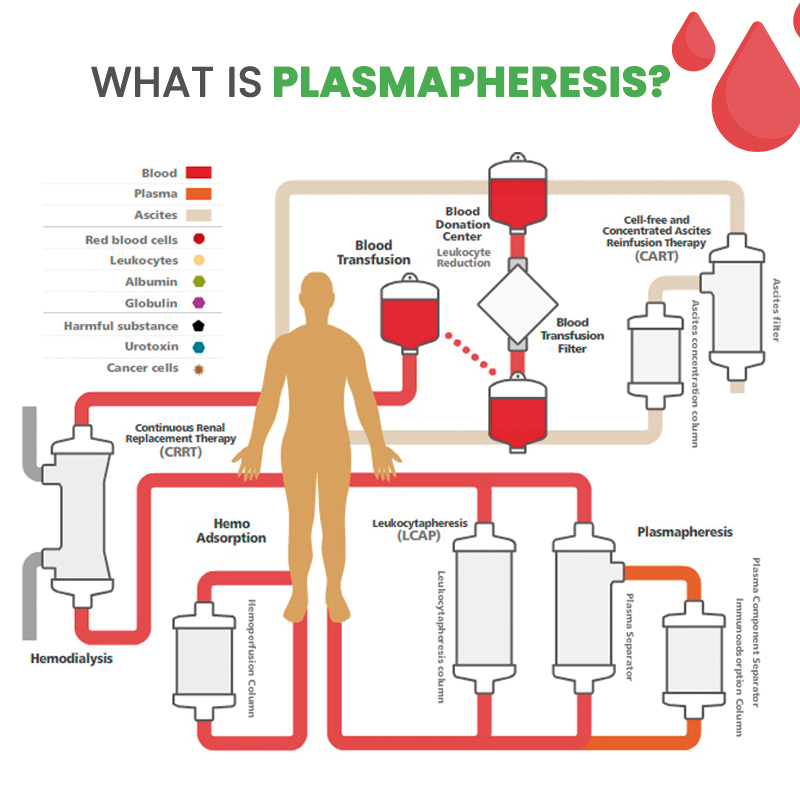
TA can be defined as a technique based on passing the patient’s blood through an extracorporeal device in order to eliminate pathogenic components that affect or perpetuate a disease and thus contribute to its treatment.
The purpose of TA is to eliminate molecules or immune complexes that affect a disease. It is a therapeutic alternative aimed at the treatment of certain diseases for which conventional treatment has not obtained the desired response or has failed.
TA applications today and in the future
Interest in TA has grown significantly over the past few years thanks to the positive results published, improved control of its indications and the availability of new apheresis procedures.
Publications in recent years describe the use of TA for the treatment of Alzheimer. In such cases, plasmapheresis is carried out to remove albumin. This involves extracting all the plasma to remove the amyloid proteins that build up in the brain.
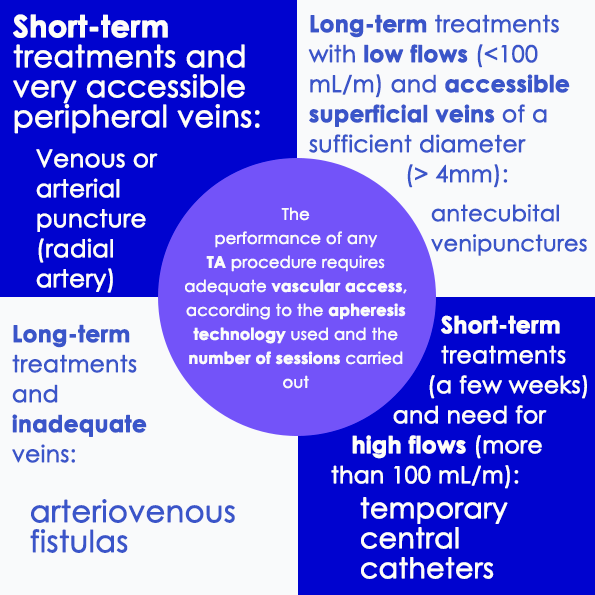
A number of procedures are carried out using TA (cytapheresis, photopheresis, haemoadsorption, plasma adsorption, LDL apheresis, double filtration, rheopheresis, immunoadsorption, MARS, Prometheus, haemoadsorption using polymyxin, red blood cell exchange), although the two main techniques used for plasma separation during apheresis are centrifugation and membrane filtration. These techniques differ in terms of plasma extraction efficiency, the vascular access that will be needed and the blood flow required to carry them out.
Centrifugation allows us to effectively separate the plasma, as well as different blood cell components. The time it takes to perform this technique will depend on the efficiency of the plasma extraction. Low blood flows (60 – 120 ml/min) are required and the procedure can be carried out through both central and peripheral lines. Some monitors allow for unipuncture mode, although bipuncture mode or dual-lumen catheters are most commonly used.
For the filtration, high permeability membranes are used which allow both the plasma and its molecules to be filtered as they pass through, retaining only the cellular component required according to the technique used. In this case, central venous cannulation is required.

However, TA involves certain risks such as the need to use large-gauge venous catheters for apheresis, which can cause complications such as bleeding, infection or pneumothorax. This particular feature means that the procedure cannot be carried out in children due to the smaller calibre of the veins.
The aim is to use less invasive vascular access that allow for high flows in both the extraction and ejection of blood.
What vascular access can improve accessibility and simplify the application of these emerging therapies?
Traditional vascular access for TA: problems and limitations
In the case of the centrifugation technique, two peripheral venous accesses are used, usually inserted in the forearms.
One of the problems we face is that the end of the peripheral catheters collapses without obtaining optimal flows: 16 G butterfly needles (used for dialysis treatment, equivalent to 5 Fr) or 17 G (4.5 Fr) short multi-perforated catheters are therefore used to ensure blood flow on entry to the machine and a short catheter of at least 20 G is also used on the return to the patient to avoid generating resistance.
Naturally, not all patients have an adequate vein diameter or an adequate vascular network for the cannulation of these calibres, not to mention the number of punctures that must be performed each time the technique is carried out. In such cases we can consider the use of reinforced tip venous catheters (midline) placed in the veins of the arm, with a minimum diameter of 4 Fr. However, the length of these catheters (preferably 15 cm) means that the tip must reach the axillary vein to achieve optimum blood flow for entry into the machine, in order to avoid repeated puncture in successive treatments.
The problems associated with central venous cannulation (CICCs, FICCs) are:
• The problems typically associated with the cannulation technique, such as pneumothorax
• Infection
• Operating Room, Interventional Radiology Room or ICU time is used for central catheter cannulation, with all the associated implications (delays in the start of TA until there is a gap in the ward/surgery schedule or the appropriate specialist is available to perform cannulation)
• Patients who need these therapies on an ad hoc basis or for a limited time and whose body image or activities of daily living are affected by CICC or FICC placement for TA.
Vascular access of the future (midline): advantages and benefits
Some of the advantages to bear in mind when using a midline to carry out some of the TA techniques are:
• Avoiding the use of central access catheters (CICC, FICC) excludes the risks mentioned above, although it is impossible to achieve the flow offered by a catheter such as a Hickman line.
• In those cases where several sessions must be carried out in a short space of time, there is no need to cannulate two peripheral venous access each time, since, with proper care, the midline catheter can be maintained by following the recommendations for use and duration of these catheters (4 weeks).
• Ultrasound-guided midline catheter placement ensures that the diameter of the vein is adequate.
Bibliography:
-
Evidence-based Therapeutic Apheresis Manual – Fernando Anaya Fdez Lomana
-
Vascular Access in Therapeutic Apheresis: Update 2013 – Ladan Golestaneh and Michele H. Mokrzycki
-
http://transfusion.granada-almeria.org/donar/aferesis
-
Therapeutic apheresis, a hopeful alternative for Alzheimer’s and 80 other diseases
-
Therapeutic Apheresis in Renal Pathology – Eva Rodríguez, Dolores Redondo-Pachon, Marta Crespo, María Dolores del Pino, Julio Pascual
-
Guidelines on the Use of Therapeutic Apheresis in Clinical Practice-Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Seventh Special Issue Joseph Schwartz, Anand Padmanabhan, Nicole Aqui, Rasheed A. Balogun, Laura Connelly-Smith, Meghan Delaney, Nancy M. Dunbar, Volker Witt, Yanyun Wu, and Beth H. Shaz



