Intravenous (IV) therapy is a cornerstone of modern medicine, enabling the delivery of fluids, medications, and nutrition directly into the bloodstream.
Peripherally Inserted Central Catheters (PICCs) have been the preferred choice for patients requiring medium- to long-term IV access. Their ability to provide central venous access with a relatively straightforward insertion has made them a staple in hospitals and outpatient settings alike.
For all the benefits of PICCs, they are not without their weaknesses. Their Central placement carries a higher risk of serious complications such as bloodstream infections, thrombosis, and mechanical issues as they terminate in a central vein, usually the superior vena cava, compared with other devices such as midlines. Additionally, insertion often requires specialist teams and imaging guidance, all adding to the cost and complexity of care.
In recent years, there has been an increasing interest in midline catheters, particularly those with midclavicular tip placement. These devices offer a compelling alternative for patients who need IV therapy for up to four weeks, with a potential reduction of the risks associated with central venous access. As clinical evidence mounts and guidelines evolve, midclavicular midlines are emerging as a safer, more cost-effective option[1], potentially reshaping vascular access practices across the UK and beyond.
PICCs VS Midlines: Understanding the Devices
When selecting a vascular access device, clinicians must weigh multiple factors, for example, therapy duration, medication type, patient anatomy, and risk profile.
Two commonly used devices for intermediate to long-term intravenous therapy are Peripherally Inserted Central Catheters (PICCs) and Midclavicular Midline Catheters. Though similar in appearance and insertion site, they differ significantly in function, risk, and suitability.
PICC
PICCs are central venous access devices inserted via peripheral veins (typically basilic or cephalic) and advanced until the tip resides in the superior vena cava.
They are suitable for:
- Long-term therapy (weeks to months)
- Irritant or vesicant medications (e.g., chemotherapy, parenteral nutrition)
- Frequent blood sampling
However, PICCs carry higher risks:
- Central line-associated bloodstream infections (CLABSI)
- Deep vein thrombosis (DVT)
- Insertion complexity, often requiring radiological confirmation and specialist teams.
Midclavicular Midline
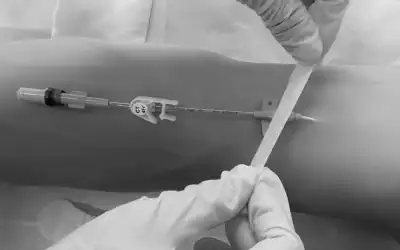
Midclavicular midlines are peripheral access devices, inserted into upper arm veins with the tip terminating near the midclavicular region, short of central circulation.
They are ideal for:
- Intermediate therapy (1 to 4 weeks)
- Non-vesicant, non-irritant medications e.g. therapies with pH 5–9 and osmolarity <900 mOsm/L
- Patients with difficult venous access or frequent hospital admissions
Advantages include:
- Lower infection risk
- Bedside insertion with ultrasound guidance
- Reduced complications such as phlebitis and thrombosis
Disadvantages include:
- Limited duration of use – not suitable for long-term therapy
- Not suitable for infusing irritant or vesicant drugs which require central access
- Risk of mechanical complications – although lower than peripheral cannulas, midlines still carry potential risks, such as occlusion, dislodgement and infiltration1.
Clinical Evidence & Guidelines: Why Choose Midclavicular Midlines over PICCs
Evidence shows that PICCs carry higher risks of bloodstream infection and thrombosis. A large multicentre study published in JAMA Internal Medicine analysed 10,863 patients and found midlines were associated with fewer complications such as bloodstream infections and catheter occlusions compared to PICCs, with similar thrombosis rates for short-term therapy (≤30 days)[2]
Further research supports this trend. A systematic review and meta-analysis of 20 studies reported that midlines reduce catheter-related bloodstream infections by up to 76% compared with PICCs (OR 0.24; 95% CI, 0.15–0.38)[3]. However, midlines were linked to a slightly higher risk of superficial vein thrombosis, which is generally less severe than the deep vein thrombosis associated with PICCs. Another study focusing on outpatient antimicrobial therapy found major complications occurred in only 0.8% of midline cases compared to 3.4% for PICCs, reinforcing their safety for intermediate-duration treatments[4].
Cost and practicality are also important for the NHS. PICCs require imaging and specialist insertion, increasing resource use and potential delays. Midlines can be placed at the bedside using ultrasound, reducing complexity and cost while improving efficiency for patients.[5]
Guidelines support this approach. NICE and NHS best practice recommend selecting devices based on therapy duration and risk, with midlines suitable for up to 28 days when infusates are compatible. The Infusion Nurses Society (INS) 2024 Standards also endorse midlines for intermediate therapies, citing lower infection risk, easier insertion and cost-effectiveness[6].
For UK hospitals, this evidence positions midclavicular midlines as a practical alternative to PICCs for most non-vesicant treatments. They offer a balance of safety, simplicity and value that aligns with NHS priorities for reducing complications and improving efficiency.
Midclavicular Midlines – Challenges & Considerations
While midclavicular midlines offer clear benefits, there are important limitations to consider. These devices are not suitable for vesicant drugs, irritant solutions or infusates with extreme pH or high osmolarity. NICE guidance and Infusion Nurses Society standards recommend midlines only for compatible therapies such as IV antibiotics, hydration and certain medications6.
Tip location remains a point of debate. The midclavicular position is peripheral, but some clinicians question whether it increases thrombosis risk or creates confusion with central lines. Consistent training and adherence to standards are essential to avoid misclassification and ensure safe practice3.
Another challenge is premature removal. Studies report early removal rates of up to 62% for midlines, often due to infiltration, leakage or patient discomfort. This can lead to multiple device placements during a single course of therapy, increasing workload and cost.4
Finally, training and awareness are critical. Successful adoption depends on clinicians understanding device selection, insertion technique and maintenance. Hospitals must invest in education and competency programmes to ensure midlines are used appropriately and safely.6
Implications for UK Practice
Adopting midclavicular midlines therefore could help the NHS meet key priorities for patient safety and cost control. Lower infection rates and fewer complications mean fewer hospital-acquired infections, which supports NHS targets for reducing avoidable harm and improving quality of care.
Financial impact is significant. PICCs require radiology support and specialist teams for insertion, which adds cost and delays. Midlines can be placed at the bedside using ultrasound, reducing procedure time and freeing up imaging capacity. This supports NHS efficiency goals and helps trusts manage workforce pressures.
Implementation will require planning. NHS trusts should review vascular access policies to ensure device selection aligns with therapy duration and risk. Training is essential so clinicians can confidently insert and maintain midlines. Manufacturers such as Vygon can support this transition by providing education, competency programmes and clinical resources.
For the NHS, midclavicular midlines represent a practical alternative to PICCs for most intermediate therapies such as IV antibiotics and hydration. They offer a safer, simpler and more cost-effective solution that aligns with NHS objectives for reducing complications, improving patient flow and delivering value-based care.
Conclusion
PICCs have served as the default for extended IV therapy, but growing evidence and updated standards highlight their risks and resource demands. Midclavicular midlines offer a safer, simpler and more cost-effective alternative for intermediate therapies, reducing infection rates and supporting NHS goals for efficiency and patient safety.
It may be time for NHS Trusts to re-evaluate current vascular access practices and consider adopting midlines where appropriate and investing in staff training, hospitals can improve outcomes, reduce costs and align with best practice. Midclavicular midlines are an option; they could represent the future of IV therapy in UK healthcare.
References
[1] Meto E, Cabout E, Rosay H, Espinasse F, Lot A-S, El Hajjam M, et al. Cost comparison of four venous catheters: short peripheral catheter, long peripheral line, midline, and PICC for peripheral infusion. J Vasc Access. 2024;25(3):1-9. doi:10.1177/11297298241258257.
[2] Chopra V, et al. “Comparative Outcomes of Midline Catheters and Peripherally Inserted Central Catheters: A Multicenter Study.” JAMA Internal Medicine. 2019;179(3):357–365.
[3] Xu T, et al. “Midline Catheters vs PICCs: A Systematic Review and Meta-Analysis.” Journal of Vascular Access. 2021;22(4):456–464.
[4] Keller SC, et al. “Complication Rates of Midline Catheters Compared to PICCs in Outpatient Parenteral Antimicrobial Therapy.” Clinical Infectious Diseases. 2018;66(3):439–445.
[5] NICE Guidance: “Intravenous Therapy Device Selection.” National Institute for Health and Care Excellence.
[6] Infusion Nurses Society (INS). Infusion Therapy Standards of Practice. 2024 Edition.