Sepsis remains a critical threat to children, with septic shock frequently requiring admission to Paediatric Intensive Care Units (PICUs).1
Early and appropriate fluid resuscitation is paramount for improving outcomes and reducing mortality in these vulnerable patients.2
While the “golden hour” concept emphasises rapid intervention, modern practice is shifting towards a personalised approach, guided by real-time haemodynamic monitoring to assess fluid responsiveness. The 2020 Surviving Sepsis Campaign guidelines advocate for the use of advanced haemodynamic variables alongside clinical assessment to guide resuscitation in children with septic shock or sepsis-associated organ dysfunction. This article aims to provide an educational overview of cardiac output monitoring, particularly pulse contour analysis, to support informed clinical decision-making in PICUs.
The Importance of Haemodynamic Monitoring:
Accurate assessment of cardiac output and fluid responsiveness is crucial in managing critically ill children. While clinical signs are valuable, they can be subjective and not always indicative of actual haemodynamic changes.
- Echocardiography: Echocardiography is a cornerstone of bedside assessment in PICUs, providing valuable insights into cardiac function.3 However, it offers a snapshot in time, requires specialised training, and may not be feasible for continuous monitoring.
- The Need for Continuous Monitoring: Continuous haemodynamic monitoring allows clinicians to track trends, detect subtle changes, and make timely interventions, leading to improved patient outcomes.
Pulse Contour Analysis: A Complementary Approach:
Pulse contour analysis offers a valuable tool for continuous haemodynamic monitoring, complementing echocardiography.4
Monitors that use software such as PRAM, are non-calibrated and estimate cardiac output by analysing the arterial blood pressure waveform, which reflects the interplay of stroke volume, systemic vascular resistance, and vascular compliance in real time.
- Pulse Pressure (PP): The difference between systolic and diastolic blood pressure (PP = Systolic BP – Diastolic BP).
eg. In a child with blood pressure of 110/50, Pulse pressure = 110-50 = 60mmHg
- Mean Arterial Pressure (MAP): Diastolic BP + 1/3 Pulse Pressure.
Mean BP for above child = 50 + 20 = 70mmHg
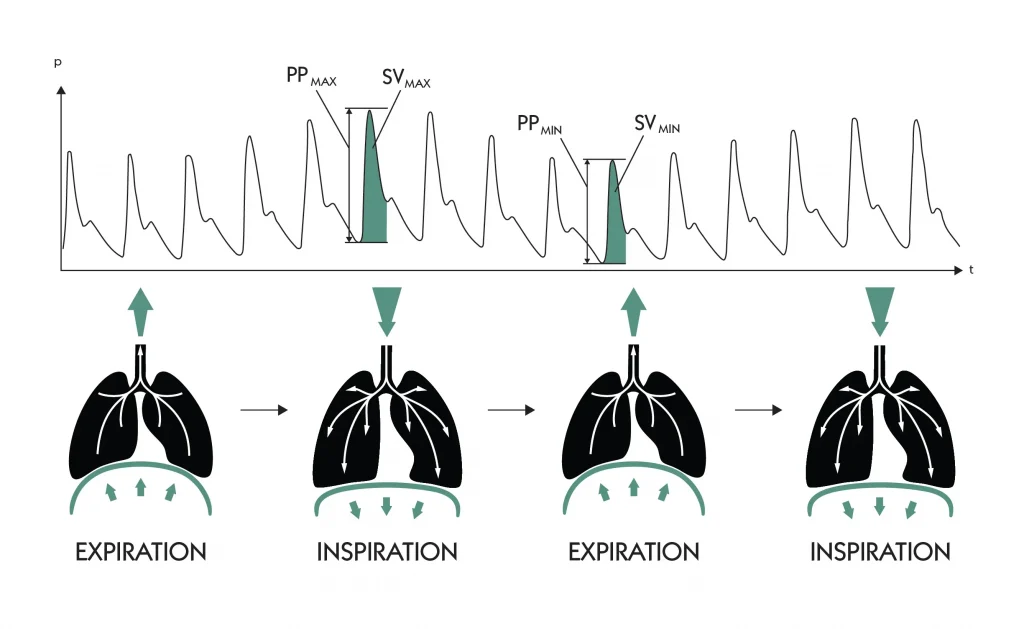
- Pulse Pressure Variation (PPV): The percentage variation in pulse pressure during the respiratory cycle. In mechanically ventilated patients, PPV can predict fluid responsiveness.
Understanding Pulse Pressure Variation (PPV):
- During positive pressure ventilation, inspiration causes an increase in left ventricular preload, leading to a rise in systolic arterial pressure.
- During spontaneous breathing, inspiration causes a decrease in left ventricular preload.
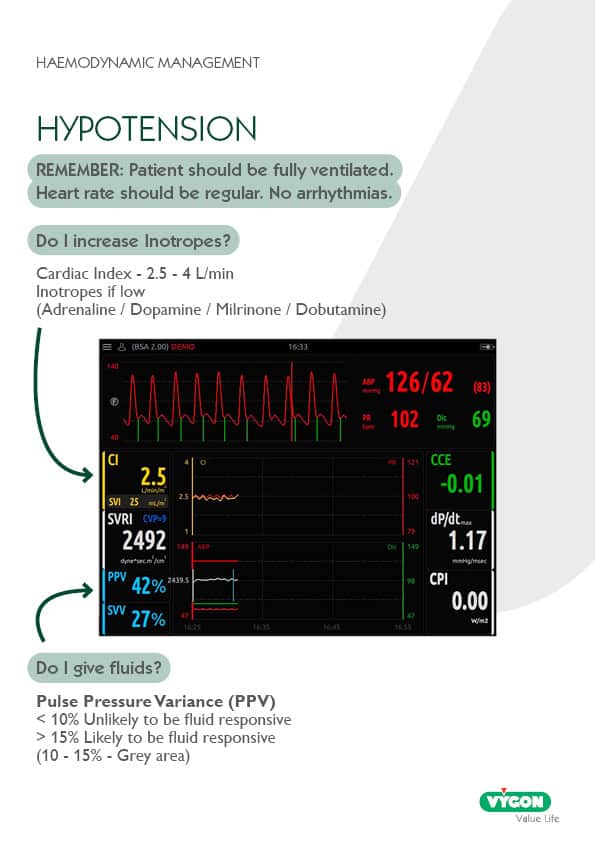
PPV to guide fluid therapy in children
- When PPV is less than 10%, your patient is UNLIKELY to respond to fluid therapy.
- When PPV is greater than 15% your patient is LIKELY to respond to fluids.
Give a 10ml/kg bolus.
- 10-15% is a GREY AREA. This needs a bit more thought and examination.
This group MAY respond to fluids.
- PRAM: Pressure Recording Analytical Method (PRAM) is a validated pulse contour method for paediatric use, providing beat-by-beat analysis and continuous monitoring of various haemodynamic parameters.
Clinical Application of PPV:
PPV can guide fluid therapy in mechanically ventilated children.
- When PPV indicates fluid responsiveness, a 10 mL/kg fluid bolus can be administered.
- Careful clinical assessment is essential in the “grey area” to determine the need for further fluid administration.
Limitations of PPV:
Accurate PPV measurement requires specific conditions:
- Mechanical Ventilation: Patients must be fully mechanically ventilated with appropriate tidal volumes (6-8 mL/kg) and without spontaneous breathing or asynchrony.
- Regular Heart Rhythm: Arrhythmias can significantly affect PPV accuracy.
PPV vs. Stroke Volume Variation (SVV):
- Both PPV and SVV assess fluid responsiveness.
- Studies suggest PPV may be superior as it more accurately reflects changes in transmural pressures and is less affected by extramural pressure changes.5
- Both variables can be affected by changes in vasomotor tone.
Conclusion:
Cardiac output monitoring, particularly pulse contour analysis using PPV, offers a valuable tool for guiding fluid resuscitation in critically ill children. By providing continuous, real-time haemodynamic data, clinicians can make informed decisions, optimise fluid therapy, and improve patient outcomes. However, it is essential to understand the limitations of PPV and integrate it with clinical assessment and other monitoring modalities. Ongoing research and education are crucial to further refine the use of haemodynamic monitoring in paediatric intensive care.
- Rodriguez-Portilla R, et al. Septic shock upon admission to pediatric intensive care units: prognostic analysis of mortality in a retrospective cohort. Bol Med Hosp Infant Mex. 2025
- Farrell D, Nadel S. What’s New in Paediatric Sepsis. Curr Pediatr Rep. 2016
- Huygh J, Peeters Y, Bernards J, Malbrain ML. Hemodynamic monitoring in the critically ill: an overview of current cardiac output monitoring methods. F1000Res. 2016
- Grensemann J. Cardiac Output Monitoring by Pulse Contour Analysis, the Technical Basics of Less-Invasive Techniques. Front Med (Lausanne). 2018
- Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002 Jun



