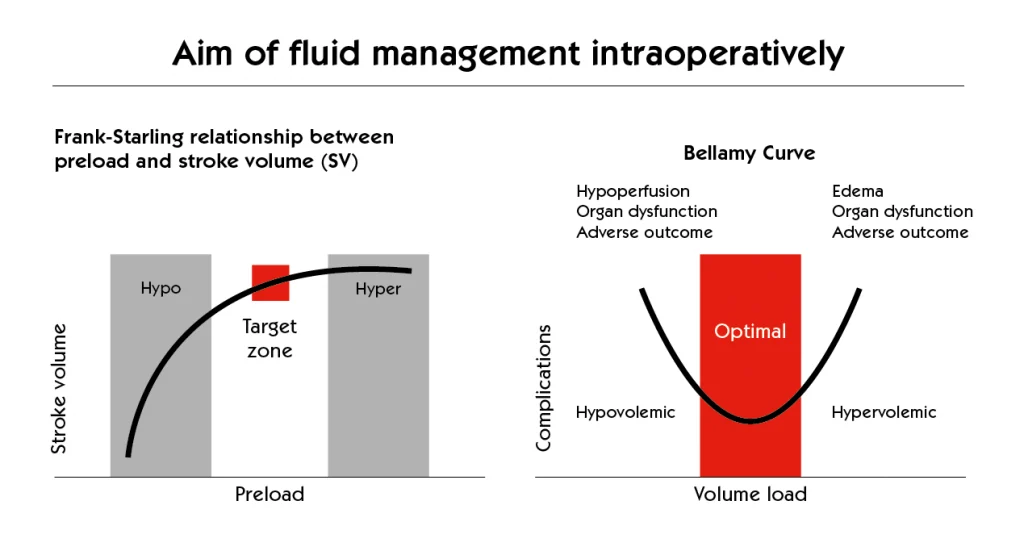
Fluid management is a cornerstone of patient care, particularly in critical conditions like septic shock. However, the line between adequate resuscitation and harmful fluid overload is often thin. Recognising the risks and implementing strategies to prevent fluid overload is essential for optimising patient outcomes.
The Risks of Fluid Overload:
Treating fluids as drugs is crucial, as their administration carries inherent risks.Just as with any medication, the benefits must be carefully weighed against potential harms. Excessive fluid administration can lead to a cascade of complications:
Organ Dysfunction:
- Increased stress on the heart, lungs, and kidneys.
- Impaired tissue oxygenation due to increased interstitial pressure and reduced blood flow.
Respiratory Complications:
- Pulmonary oedema, resulting in compromised gas exchange.
- Respiratory distress and hypoxia.
Cardiovascular Strain:
- Increased cardiac workload, potentially leading to cardiac dysfunction and heart failure.
Delayed Recovery:
- Prolonged hospital stays and poorer overall outcomes.
Preventing Fluid Overload: A Multifaceted Approach
Experts’ opinion:
We propose to routinely use a personalized approach of intraoperative fluid infusion/volume expansion based on the individual hemodynamic response to volume titration to reduce the deleterious side effects of fluids and improve patients’ outcome (agreement 100%)1
Preventing fluid overload requires a proactive and personalised approach.
- Individualised assessment of fluid needs.
- Continuous monitoring of patient response to fluid administration.
- Adjustment of infusion rates based on real-time data.
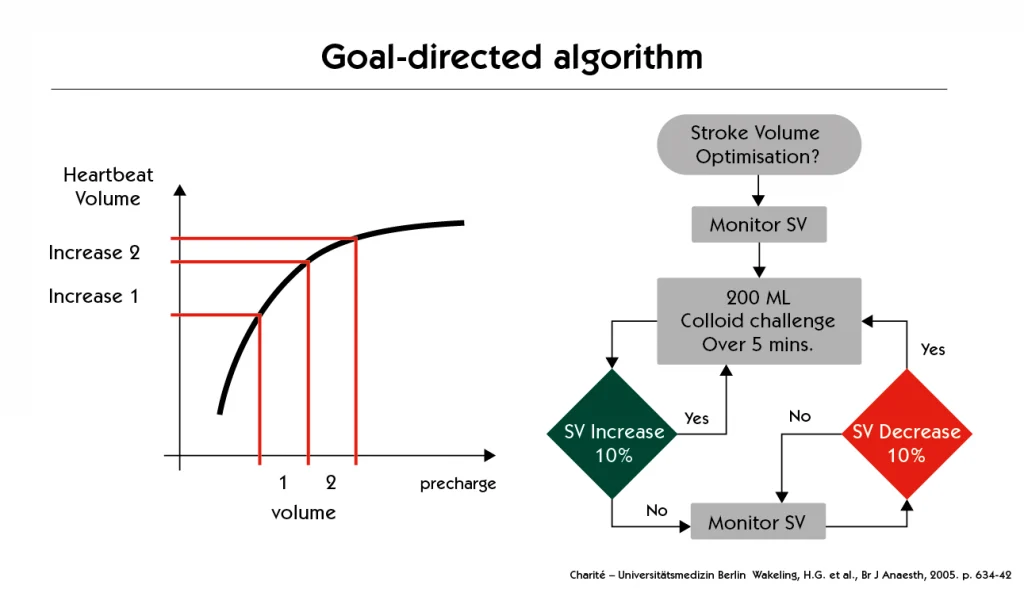
Early Goal-Directed Therapy (EGDT):
- Utilising specific haemodynamic goals to guide fluid administration.
- Optimising cardiac preload, afterload, and contractility.
- Matching oxygen delivery with oxygen demand.
- This can help avoid both under-resuscitation and fluid overload.
Dynamic Monitoring:
- Employing dynamic parameters like stroke volume variation (SVV) or pulse pressure variation (PPV).
- Assessing real-time fluid responsiveness.
- Helps make informed decisions about further fluid administration.
Strict Monitoring:
- Frequent monitoring of vital signs, fluid input/output, and clinical status for early detection of fluid overload signs.
- Allows for timely interventions to prevent progression.
Beyond the Numbers: Harnessing SVV, PPV, and Dynamic Elastance for Precision Fluid Therapy
In the dynamic environment of anaesthesia, accurately assessing a patient’s fluid responsiveness is paramount. Stroke Volume Variation (SVV) and Pulse Pressure Variation (PPV) have become essential tools in this assessment for mechanically ventilated patients.
Dynamic Elastance (PPV/SVV): Unveiling a Deeper Relationship
The ratio of PPV to SVV, or dynamic elastance, introduces an intriguing layer to our understanding of fluid responsiveness. It essentially describes the change in arterial pressure for a given change in ventricular volume during mechanical ventilation.
Clinical Significance and Potential Advantages:
- Refining Fluid Responsiveness Prediction: Some evidence suggests that dynamic elastance might be a more specific indicator of preload responsiveness in certain situations, potentially reducing false positives seen with PPV or SVV alone.
- Assessing Ventricular Compliance and Arterial Tone: The relationship between changes in volume (SVV) and pressure (PPV) can provide indirect information about the interplay between ventricular compliance and arterial tone. A high dynamic elastance might indicate a stiffer ventricle or increased arterial tone making the pulse pressure more sensitive to volume changes.
- Guiding Personalised Therapy: By considering dynamic elastance alongside absolute SVV and PPV values, we can potentially tailor fluid administration more precisely, avoiding both inadequate resuscitation and the detrimental effects of fluid overload.
The Importance of Haemodynamic Monitoring:
Minimally invasive haemodynamic monitoring systems are invaluable tools in preventing fluid overload. Utilising systems that provide real-time data on cardiac output, stroke volume, systemic vascular resistance, and other haemodynamic parameters, allow clinicians to:
- Assess the patient’s haemodynamic status with precision.
- Make informed decisions regarding fluid management and tailor fluid administration and vasopressor therapy.
- Optimise cardiovascular performance.
- Avoid both under-resuscitation and excessive fluid administration.
Moving forwards
Effective fluid therapy hinges on striking a balance between adequate resuscitation and avoiding fluid overload. This requires a multidisciplinary approach, close patient monitoring, and the ability to adjust fluid administration based on the patient’s evolving condition.
While further research is warranted, incorporating the concept of dynamic elastance into our haemodynamic assessment could represent a step towards more individualised and effective fluid management strategies in anaesthesia. Continuous monitoring systems capable of displaying these dynamic parameters are becoming increasingly valuable in our daily practice, ensuring we have the best tool to assess and titrate accurately.
By understanding the risks and implementing appropriate monitoring and management strategies, clinicians can minimise the risk of fluid overload and improve patient outcomes.
References
1. Perioperative hemodynamic optimization: from guidelines to implementation-an experts’ opinion paper. Fellahi JL, Futier E, Vaisse C, Collange O, Huet O, Loriau J, Gayat E, Tavernier B, Biais M, Asehnoune K, Cholley B, Longrois D.Ann Intensive Care. 2021 Apr 14;11(1):58. doi: 10.1186/s13613-021-00845-1. PMID: 33852124; PMCID: PMC8046882.
Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock Emanuel Rivers, M.D., M.P.H., Bryant Nguyen, M.D., Suzanne Havstad, M.A., Julie Ressler, B.S., Alexandria Muzzin, B.S., Bernhard Knoblich, M.D., Edward Peterson, Ph.D., and Michael Tomlanovich, M.D. for the Early Goal-Directed Therapy Collaborative Group*
Goal directed fluid therapy decreases postoperative morbidity but not mortality in major non-cardiac surgery: a meta-analysis and trial sequential analysis of randomized controlled trials. Som A, Maitra S, Bhattacharjee S, Baidya DK. J Anesth. 2017;31:66–81.
Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Malbrain, M.L.N.G., Van Regenmortel, N., Saugel, B. et al. Ann. Intensive Care 8, 66 (2018). https://doi.org/10.1186/s13613-018-0402-x
García MI, Romero MG, Cano AG, Aya HD, Rhodes A, Grounds RM, Cecconi M. Dynamic arterial elastance as a predictor of arterial pressure response to fluid administration: a validation study. Crit Care. 2014 Nov
Zhou X, Pan W, Chen B, Xu Z, Pan J. Predictive performance of dynamic arterial elastance for arterial pressure response to fluid expansion in mechanically ventilated hypotensive adults: a systematic review and meta-analysis of observational studies. Ann Intensive Care. 2021 Jul 31;



