Based on a presentation by Dr Keliana O’Mara, PharmD, NICU Pharmacy specialist WakeMed Health and Hospitals, United States
In neonatal intensive care units (NICUs), where the tiniest patients rely on technology for survival, precision isn’t a luxury, it’s a requirement. Among the many clinical tools used daily, enteral feeding and medication delivery systems play a vital role. But are current systems accurate and safe enough for neonates, especially for drug administration involving extremely small doses?
Dr. Keliana O’Mara tackled this question during VYNEODAYS 2024, offering a deep dive into the current limitations, risks, and potential alternatives to commonly used enteral syringe systems. Her session offered a wake-up call to clinicians and healthcare system designers alike: The syringe you’re using could be the difference between an effective dose and a dangerous misadministration.
The Challenge of Enteral Safety in Neonatology
Premature neonates, especially those born extremely preterm, rely on the enteral route for both nutrition and medication, often for weeks or months. The duration depends on gestational age, oral feeding abilities and any existing comorbidities. The enteral systems consist of feeding tubes and syringes, and while they’re essential, they aren’t without risks.
Complications may arise during tube insertion, from prolonged dwell times that increase the chance of bacterial contamination, or during administration of feeds and medications. Potential complications include infections, necrotising enterocolitis (NEC), or other gastrointestinal issues.
As Dr. O’Mara emphasised, a device must be safe, accurate, and easy to use, because even the best protocols can fail if the tools themselves are inadequately suited to the task.
In fast-paced NICU environments, complexity can lead to workarounds or skipped steps, especially when infants require frequent, small-volume medications throughout the day (up to 10 medications daily).
Critical Risks: Tubing Misconnections and Dosing Precision Challenges
To prevent misconnection errors, international standards now mandate unique tubing connectors for different body systems. While this improves safety by design, it does not directly address the critical issue of dosing accuracy.
There is currently no formal accuracy standard for oral or enteral syringes. While hypodermic syringes are held to a ±5% standard threshold (ISO 7886), enteral devices lack such regulation. A published expert consensus suggested that ±0-10% variance may be acceptable depending on the medication’s risk profile, with stricter expectations for high-risk drugs.
The commonly used ±10% benchmark for enteral syringe assessments originated from studies conducted by the ENFit manufacturer and may not be sufficient for neonatal use. It’s important to note that ENFit was developed for enteral nutrition delivery, not for medication administration, where precision is paramount.
Small Patients, Small Doses, Big Risks
When clinicians observe an unexpected patient response, such as a variation in medication effect, syringe accuracy is rarely questioned. As Dr. O’Mara noted, “We assume that once a device has reached the bedside, it has been tested, validated, and approved for reliable use”.
Yet, here is the alarming reality:
- 12.3% of prescribed liquid medication doses (enteral/IV) are reported as immeasurable with current dosage forms
- Nearly 25% of hospitalised paediatric patients, and even higher for neonates, receive doses ≤0.2 mL
One critical factor impacting syringe performance is dead space – the residual volume remaining after plunger depression:
- IV syringe: ~0.07 mL
- ENFit Standard: ~0.2 mL
- ENFit Low Dose Tip (LDT): ~0.15 mL
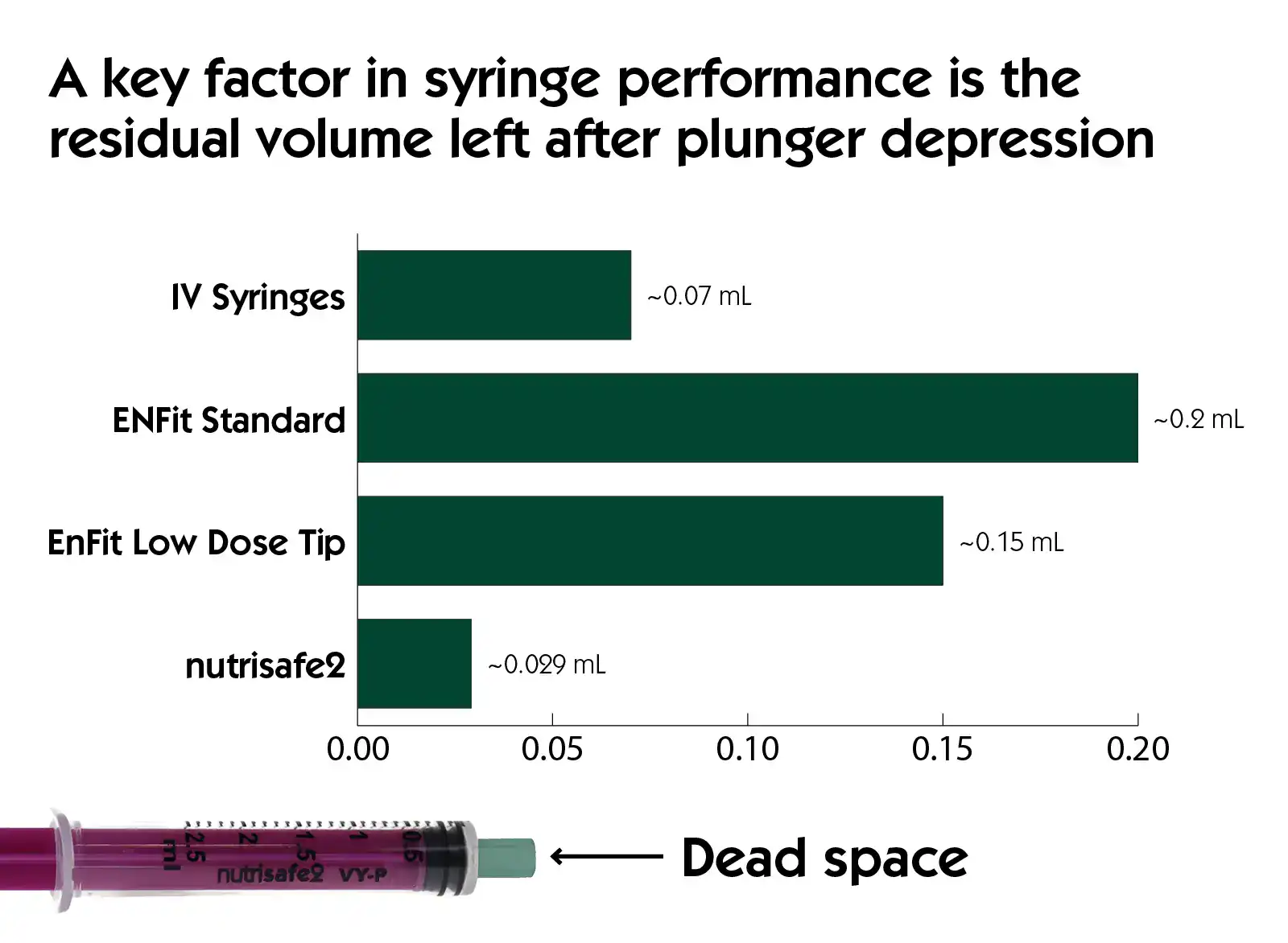
For neonates, where therapeutic doses often match or fall below these volumes, under- or overdosing becomes a real risk.
In parallel:
- 91% of neonatal admissions involve at least one medication error
- ~66% of medications used in NICUs are unlicensed for neonates
- Medications administered enterally include high-risk agents such as opioids, antihypertensives, diuretics, and immunosuppressants
With neonates unable to verbalise symptoms, accurate dosing is essential to interpret subtle clinical changes.
Testing Syringe Accuracy: Simulation vs. Reality
Two methods are commonly used to evaluate syringe performance:
- Computational Fluid Dynamics (CFD): Simulations using ideal conditions (e.g., water, perfect filling technique)
- Volumetric/Gravimetric Testing: Real-world assessments measuring liquid volumes drawn and delivered
While CFD can offer useful theoretical insights, the models used in ENFit testing simulated only water, excluded real-world variables like fluid viscosity, and assumed perfect technique by the caregiver, which is far from a clinical reality.
In studies, ENFit LDT syringes showed significant inaccuracy when used to deliver doses:
- CFD simulations showed up to 300% dosing variance.
- Real-world gravimetric testing showed ±10% dosing variance in nearly 40% of 0.5 mL tests and 25% of 1mL tests.
These clinical studies have shown that ENFit LDT syringes, created as a solution to the problem of standard ENFit (which has a dosage variance >10% for doses < 2 mL), fail to reliably improve dosage accuracy.
Although the FDA acknowledged the risk of overdose with LDT, the recommended mitigations, such as using filling adaptors or sterile water flushes, were not studied in the simulations. This casts doubt on their reliability and clinical feasibility, particularly in fragile neonates where flushing with water after every dose can run into some additional problems.
Nutrisafe2: a safe neonatal enteral system suited for preemies
Faced with the limitations of existing systems, particularly ENFit and ENFit LDT syringes in terms of accuracy for small volumes, a neonates-specific enteral system has been developed: Nutrisafe2. Designed specifically for newborns, this system aims to guarantee safety and accuracy while preventing connection errors, in accordance with standards.
Dr. O’Mara’s team conducted a comparative study of Nutrisafe 2 vs ENFit LDT. The findings were striking:
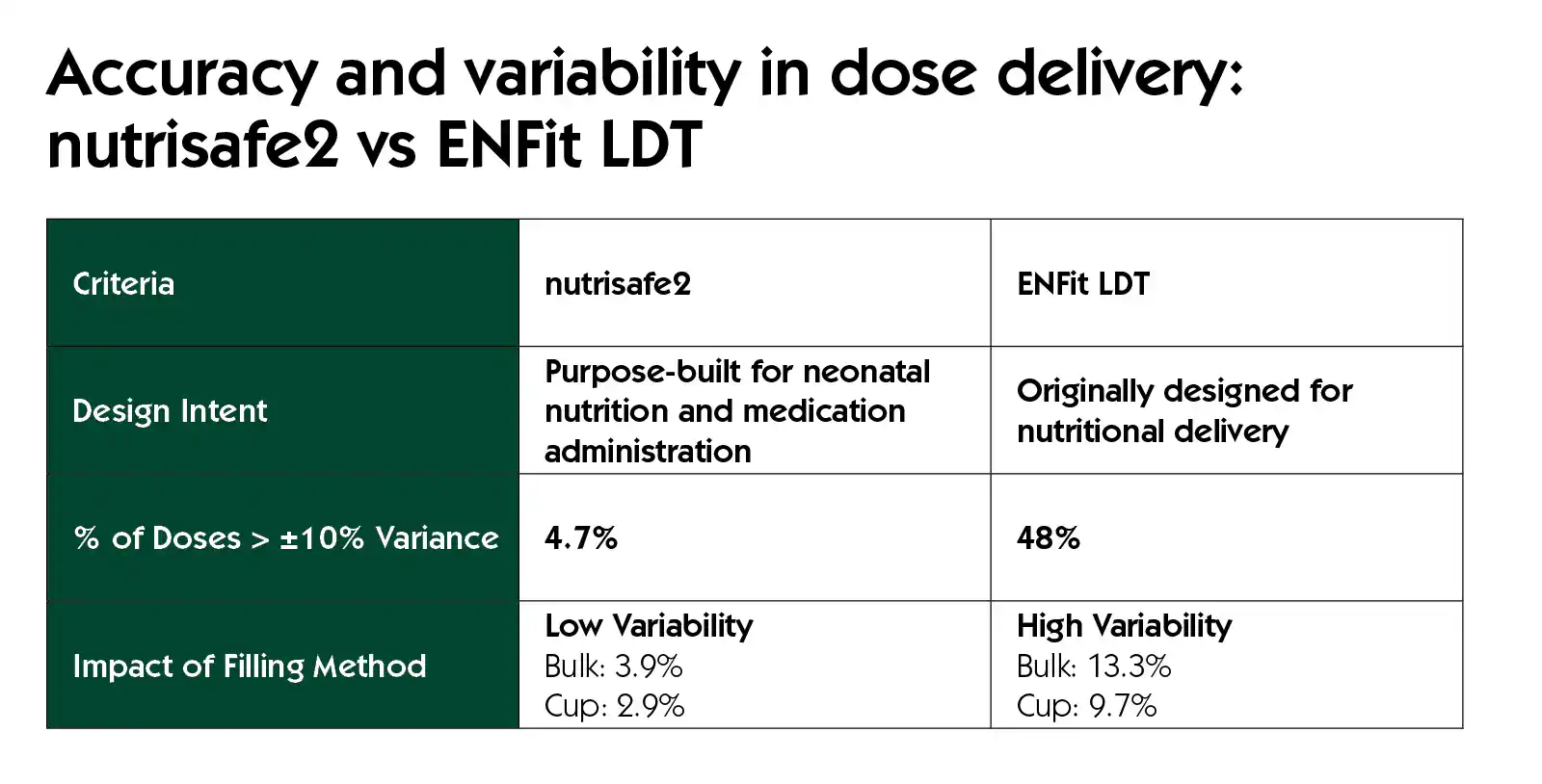
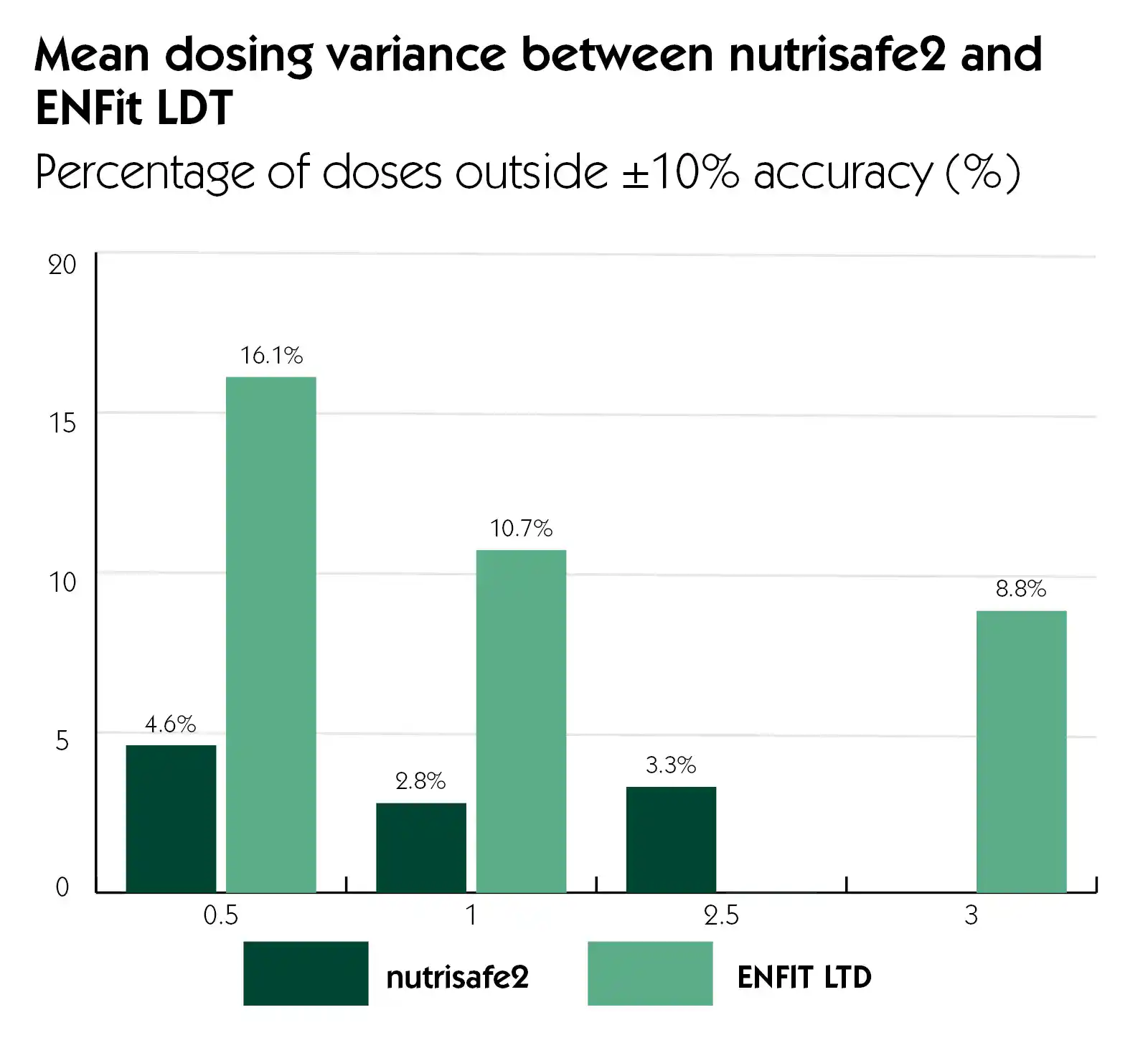
In short, Nutrisafe2 demonstrated:
- Superior precision
- Performance for Small volumes: Even in lower volume use (≤0.3 ml)
- Less variation according to the filling method used
- Dosing consistency: high reproducibility across conditions
- Significant reduction of dosing error
- Compliance with safety standards to prevent misconnections
Its neonatal-specific design appears to offer the level of accuracy required in NICUs.
Conclusion: Towards Safer Enteral Care
Neonates can’t tell us when something feels wrong. An underdose or overdose might manifest only as a subtle change in vitals, feeding behavior, or irritability. Yet in these vulnerable patients, such variations can make a life-altering difference.
Device performance matters, and the tools we use today may not be good enough.
While ENFit helped address misconnection risks, it falls short in dosing accuracy, particularly for neonates. Until global standards improve, adopting proven high-accuracy solutions like Nutrisafe2 is essential to reduce dosing errors, mitigate risk, and elevate safety in neonatal care.
Implementing devices designed specifically for this population is a crucial step towards safer, more effective enteral administration in neonatology.



