Author: Neus Monmeneu Salavert
In cancer patients, choosing an appropriate venous access device is crucial for effective treatment, minimising complications, and reducing healthcare costs.
Key management decisions, such as the timing of device removal after therapy, can affect clinical outcomes. Given that current international guidelines lack specific directives on these issues, a global consensus of experts from different countries was deemed appropriate.
A group of 11 experts from three continents, including oncologists and healthcare professionals, was selected. After a thorough review of clinical trials and guidelines on central venous access devices (CVAD) in oncology published between January 2013 and December 2023, specific recommendations were developed for the selection and management of CVAD in cancer patients.
Thus, a consensus was reached on 10 considerations related to: indications for a CVAD, available options for CVAD, the role of staff and patients in choosing the CVAD, factors influencing the selection of a port versus an external catheter, logistical requirements for inserting the port and external catheter, stakeholders responsible for inserting the port and external catheter, factors determining the removal of a port after completing definitive therapy, and recommended flushing frequency when the CVAD is not in use.
10 Considerations: 10 Options
When is a CVAD indicated?
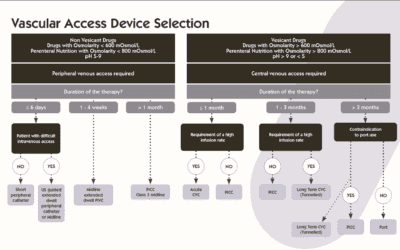
The use of a CVAD is especially recommended in cancer patients who require the administration of vesicant or irritant drugs, as these can cause serious complications if administered peripherally. Its use should also be considered when peripheral venous access is insufficient or difficult, even with ultrasound guidance. In these cases, the CVAD helps reduce the risk of phlebitis, extravasation, and tissue damage.
What options exist?
Available devices include external catheters (PICC, CICC, FICC, tunnelled or not) and fully implantable devices (thoracic, brachial, or femoral ports). The choice depends on the duration of treatment, frequency of use, and the patient’s clinical setting.
Who should decide the type of device?
The selection of the CVAD should be a collaborative decision involving the prescribing professional, the vascular access team, the patient, the device maintenance team, and, when necessary, caregivers. This decision should be based on a deep understanding of the patient’s clinical status, device characteristics, possible complications, and the suitability of the CVAD for the intended therapy.
Port or external catheter?
External catheters are preferable for medium-duration vascular access (less than 3–4 months) or for frequent long-term access (daily or weekly). In contrast, fully implantable ports are ideal for infrequent long-term access (every 2–3 weeks). They are also recommended for patients living in environments with lower hygiene or privacy, or who value aesthetics and comfort, such as those who swim.
What is needed to insert a port?
Port insertion requires device availability, access to appropriate facilities (with aseptic equipment, imaging, and monitoring), and the presence of professionals trained in venous access procedures. Additionally, informed patient consent is essential.
Who should insert a port?
Only healthcare professionals with specific and appropriate training should do so, such as surgeons, interventional radiologists, anaesthesiologists, oncologists, intensivists, advanced practice nurses, and nursing staff, always within the regulatory framework of the corresponding healthcare system.
What is needed to insert an external catheter?
Logistical requirements are similar to those for a port: device availability, appropriate facilities, trained personnel, and informed patient consent. Access to the medical history and coordination with other hospital services is also important.
Who should insert external catheters?
They should be inserted by healthcare professionals with specific training, including physicians, clinical nurses, physician assistants, and nursing staff, always within the corresponding regulatory framework.
When should a port be removed?
Ports should be removed after completing definitive therapy in patients at low risk of early relapse, when short-term venous access is not anticipated. This decision should consider patient preference, the risk of complications if the port remains in place, and the difficulty of future reinsertion.
How often should an inactive CVAD be flushed?
Ports should be flushed every 4 to 12 weeks, according to local protocols. External catheters require weekly flushing. In both cases, exclusive use of saline solution is recommended, except for devices used for haemodialysis or apheresis, which may require anticoagulant solutions.
Limitations of the International Consensus on CVAD in Oncology
Although this consensus represents a significant advance in standardising the use of central venous access devices (CVAD) in cancer patients, it is important to recognise its limitations. First, despite its international nature, some key regions such as Brazil and other South American countries were not represented on the expert panel, which could limit the global applicability of the recommendations.
Second, the consensus did not address specific technical aspects related to device insertion, such as the most appropriate surgical or interventional techniques for each type of CVAD. These topics, although fundamental to clinical practice, are covered in other specialised guidelines and texts published in recent years.
Furthermore, recommendations on the prevention and management of complications associated with CVADs, such as infections or venous thrombosis, were also not included. These aspects have been analysed in previous high-quality consensus documents, but their exclusion in this work leaves a gap that should be complemented by other sources.
Conclusion
Central venous access devices are essential tools in modern cancer treatment. Their correct selection, insertion, and maintenance not only optimise therapeutic efficacy but also improve patient quality of life and reduce the risk of complications.
This international consensus provides a clear, evidence-based guide to address the most critical aspects of CVAD use in oncology. By promoting interdisciplinary collaboration, respect for patient preferences, and the implementation of standardised protocols, safer, more efficient, and patient-centred care is facilitated.
The recommendations collected here offer healthcare professionals a solid foundation for clinical decision-making, adaptable to different healthcare and cultural contexts. Their application will help improve clinical outcomes and establish quality standards in the management of CVADs in cancer patients.
Bibliography
Jahanzeb, M., Wu, C., Lim, H., Muro, K., Xu, L., Somashekhar, M., Somashekhar, S. P. S. P., Zhang, X., Qiu, X., Fu, Y., & Pittiruti, M. (2024b). International experts consensus on optimal central vascular access device selection and management for patients with cancer. The Journal Of Vascular Access. https://doi.org/10.1177/11297298241300792