Healthcare professionals working with oncology patients are used to handling fully implanted catheters. In recent years, PICC-port has proven to be very useful in the field.
However, any vascular access device can become a problem if its placement has not been optimal and/or its maintenance is not being done properly.
Its proper use depends on the patient being able to conclude their treatment safely and in the estimated time.
In this article, we propose 6 measures that will help us to ensure that their performance is optimal.
During the insertion of a PICC-port
Ultrasound-guided puncture
There is no other way to understand the relationship between the vein and catheter calibres than using ultrasound. Of course, it is also essential to perform a single puncture on the first attempt.
We know that repeated punctures in the same vein can increase the risk of thrombosis by up to 80%. The use of ultrasound will allow us to choose the vein with the largest calibre available in the arm, generally in the yellow area.
The vein of choice in this case is the basilic vein whose course is straighter (compared to the cephalic vein). It usually offers an adequate calibre and is far from structures to be avoided (arteries, nerves).
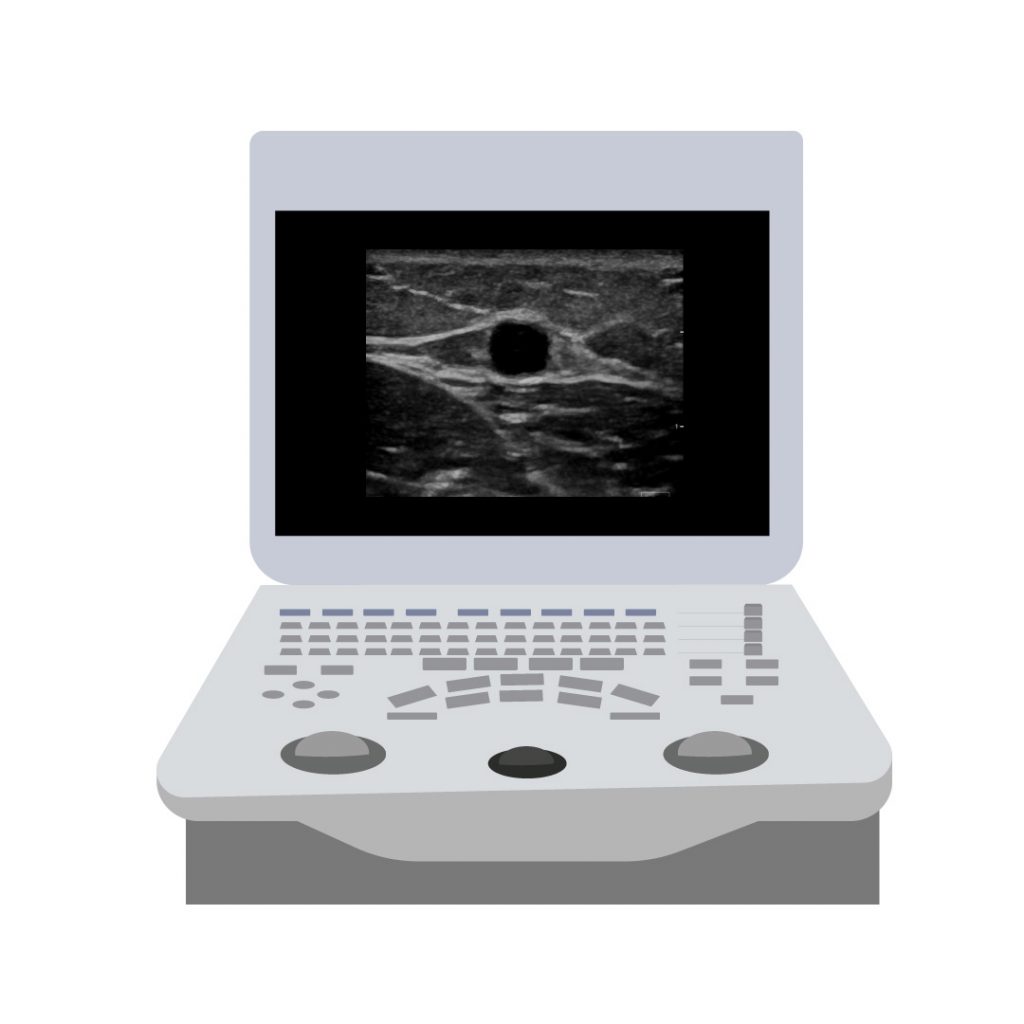
Basilic vein. Ultrasound image: Fujifilm-Sonosite.
However, it is necessary to scrupulously assess each vein when using the RaPeVA method as others may be more suitable for puncture due to diameter or location:
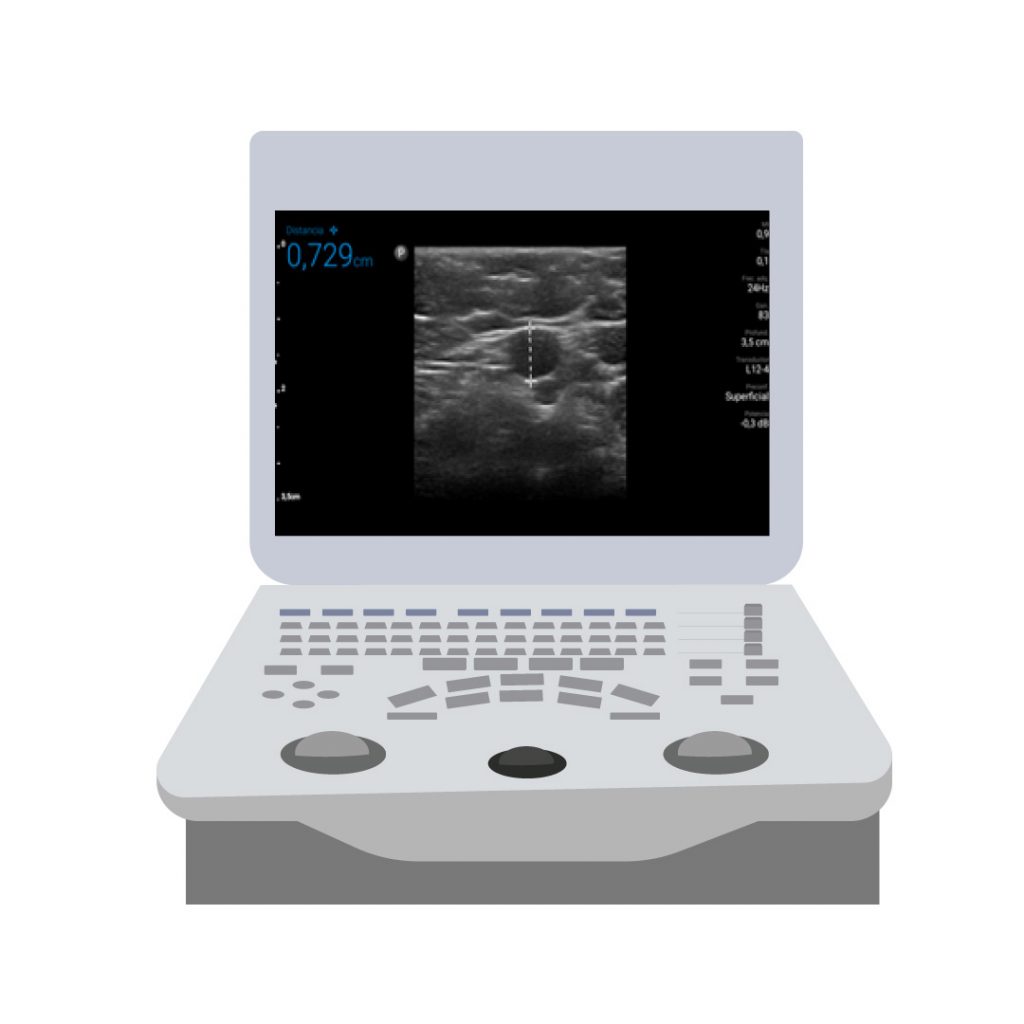
Brachial axillary vein, 7.29 mm in diameter. Source: Gloria Ortiz.
An area to avoid is the one where the group formed by the brachial artery, the 2 brachial veins and the median nerve is located. It is called the Mickey Mouse sign.
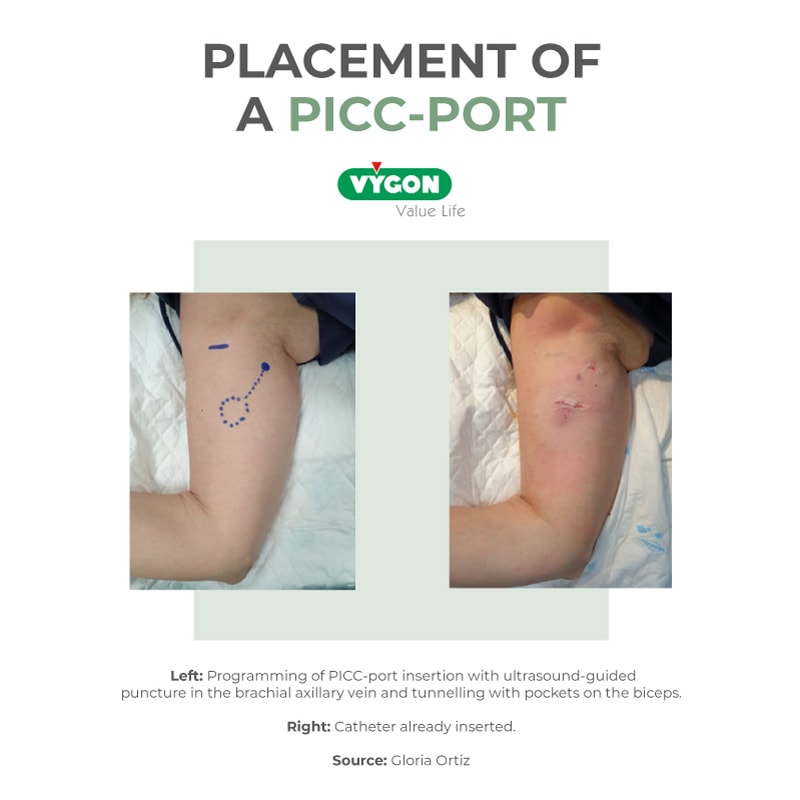
Tunnelling in the green zone and the pocket over the biceps
Although puncture in the yellow zone of the arm generally allows a greater venous calibre to be obtained, since the brachial axillary vein is punctured, it is necessary to obtain a safer and more comfortable zone for venous access management.
In the case of PICC-port, keeping the port in the yellow zone (where there is more humidity and more hair follicles) may eventually lead to its accidental exit.
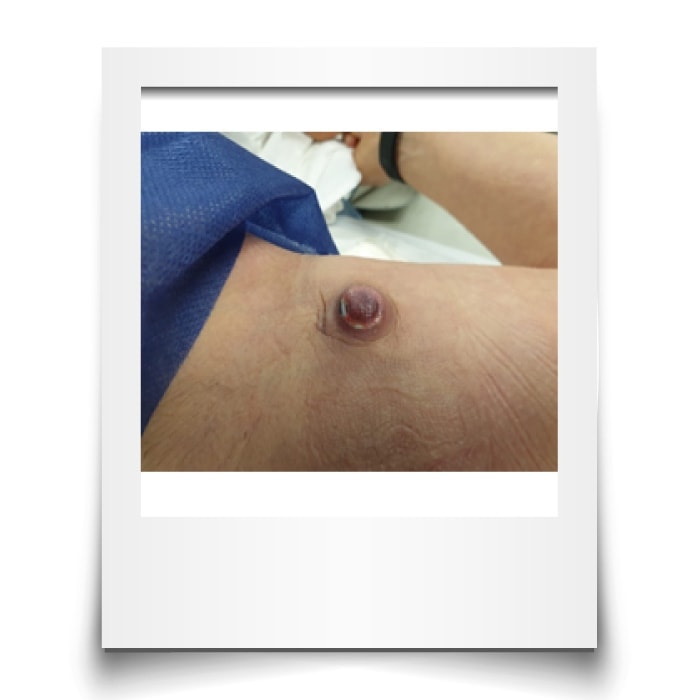
PICC-port extrusion in the yellow zone. Source: Gloria Ortiz.
This complication is easily solved by planning and performing a tunnelling to the green zone of the arm:
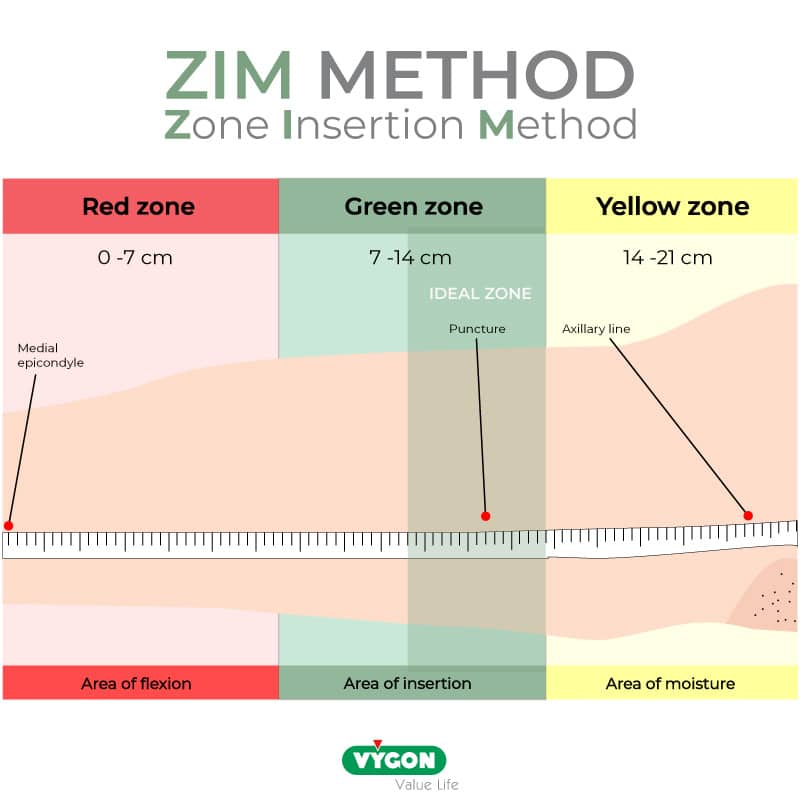
Thus, by placing the port on top of the biceps muscle, we provide a natural support. It will be easier to puncture later thanks to the stable base provided by the muscle itself.
Intracavitary echocardiography
A catheter tip that is not properly positioned in the lower third of the superior vena cava is susceptible to several complications such as malfunction, risk of venous thrombosis and superior vena cava syndrome, vein wall erosion, among others.
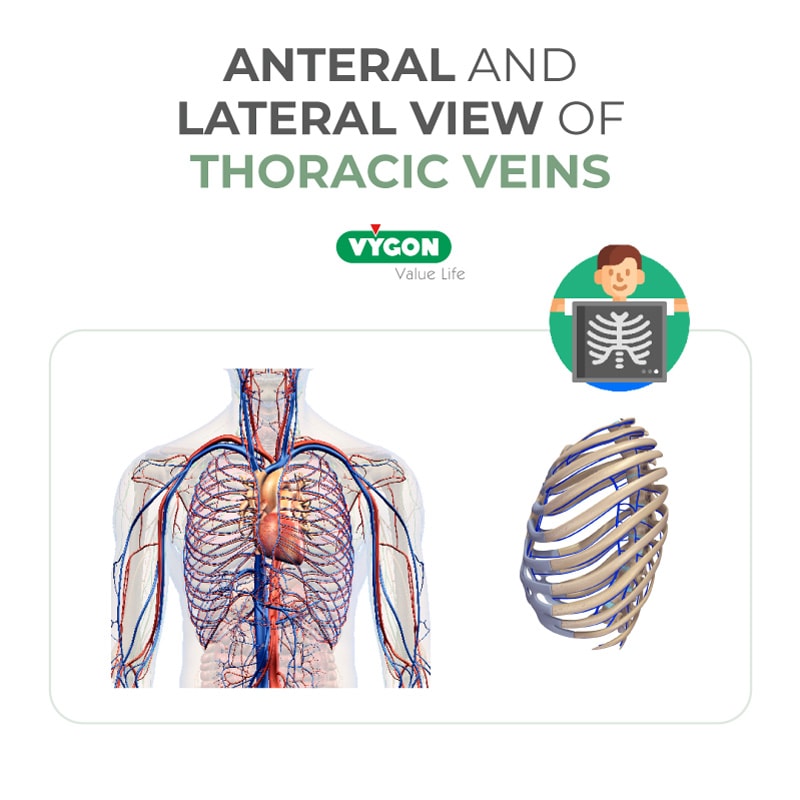
The use of chest X-rays to confirm the position of the tip, although still very common, has been superseded by other methods.
The problem with radiography is that it is impacted by the effect of overlapping planes: in an anteroposterior image it may appear that the catheter is placed in the superior vena cava when in fact, it is in a more superficial vein (such as the internal mammary vein, also called internal thoracic vein, which runs anterior to the superior vena cava) or a deeper vein (such as the azygos vein, which runs posterior to the superior vena cava) but which are in the same plane as the superior vena cava.
Therefore, if there is no other resource than radiology confirmation, it is always good practice to perform a lateral x-ray to be able to see through this effect.
Another way to intraoperatively confirm the catheter tip is through the intracavitary ECG, which is based on the principle of the electrical potential of the heart and its reading. It is cheaper, more precise and radiation-free. The changes in the P wave can be observed, which will indicate the distance of the catheter tip from the cavoatrial junction. As the catheter tip approaches the sinus node, the P wave of the intracavitary tracing increases.
The correct position is when the P wave has reached its maximum amplitude which corresponds to a location in the lower third of the superior vena cava.
The only way to know when its amplitude is maximal is to continue advancing the catheter until a negative P wave is seen. At this point, the catheter is retracted and left in the position where the P wave was fully positive and maximal.
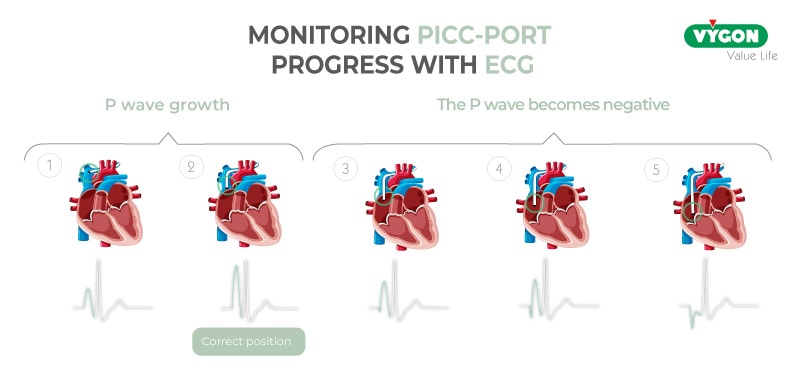
This method is gaining strength over the years and is recommended by international guidelines.
During the management of a PICC-port
Any port should be punctured with a non-coring needle, also known as Huber needle.
This type of needle has the particularity of not removing silicone micro portions from the septum. They ensure that the catheter does not leak through the self-sealing silicone, which would occur if carotid needles were used.
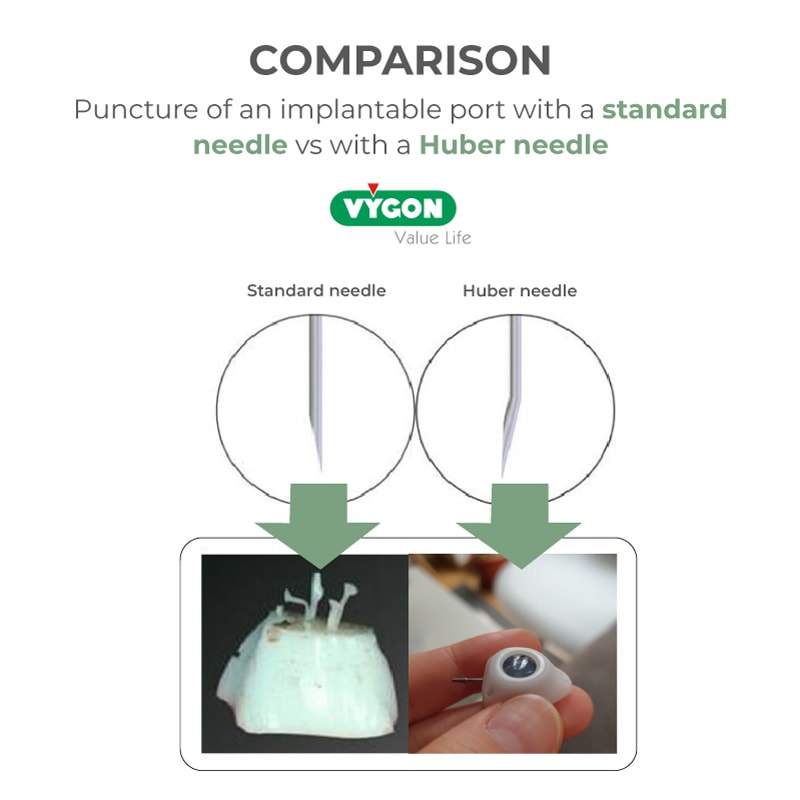
When the PICC-port is placed, a Huber needle is always included in the catheter kit to check the correct functioning of the catheter after its immediate insertion. For subsequent use, the Huber needles on the market have a 90º angle for greater patient comfort.
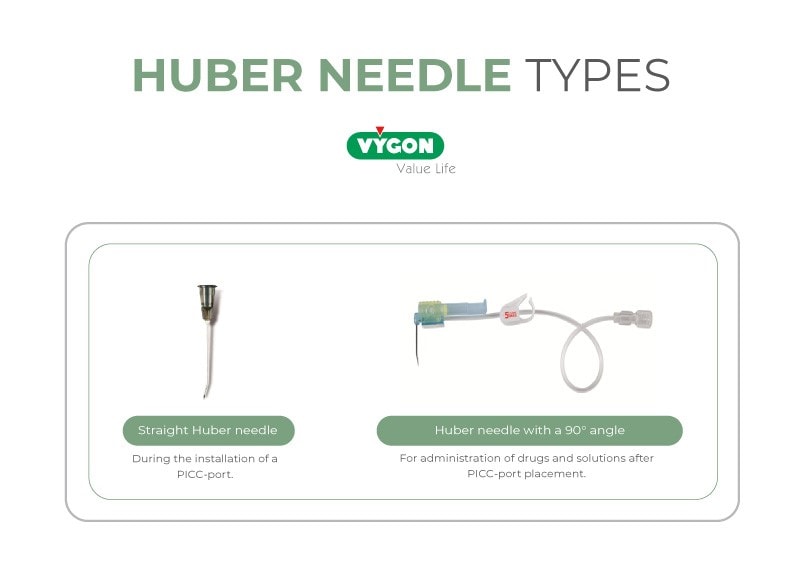
Huber needles have different Gauges and lengths. It is always recommended to use the smallest needle gauge necessary and with a length that is as adapted as possible to the height of the port, so that the needle does not remain outside the skin.
Pulsed washing before and after using a PICC-port
It is essential to check the permeability of the PICC-port before use, both in aspiration and administration.
Washing with serum is the simplest and most direct way to check for resistance to the entry of the liquid. If there are difficulties in blood extraction, it would indicate to the professionals that there is some type of complication (complete or partial obstruction, fibroblastic sheath).
In addition, when the usage of a PICC-port is no longer needed like PICCs or any type of CVC, it should be flushed in a pulsed manner with at least 10 ml of sterile saline to wash out the remnants of previous administrations.
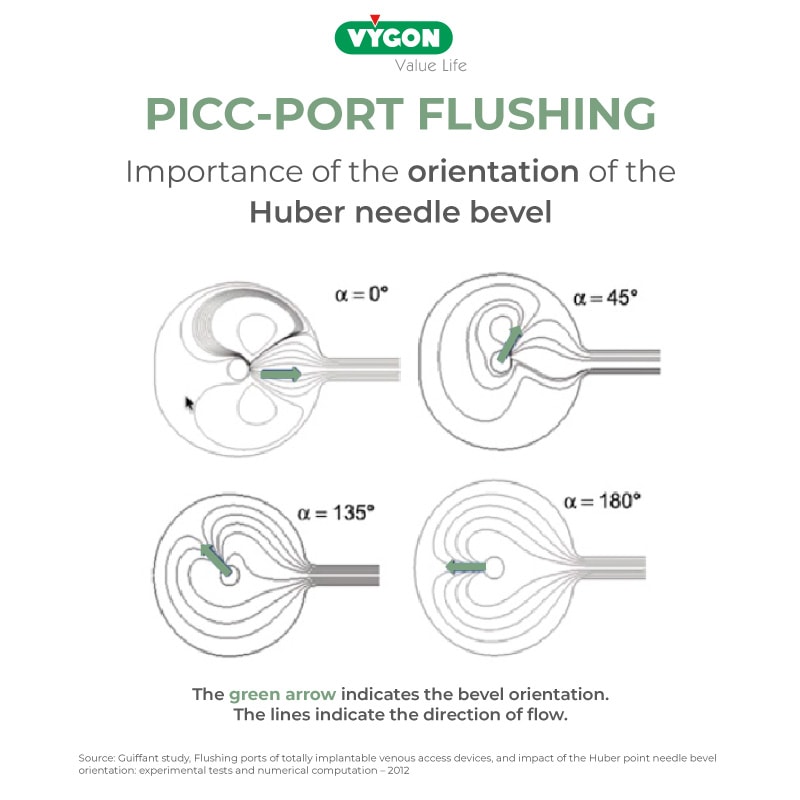
In the case of the reservoir, it is also important to monitor the orientation of the bevel of the Huber needle which, when it is removed, should face the lower wall of the port, opposite the connection of the catheter with the port, in order to produce a circular and very effective flushing of any debris remaining in the port.
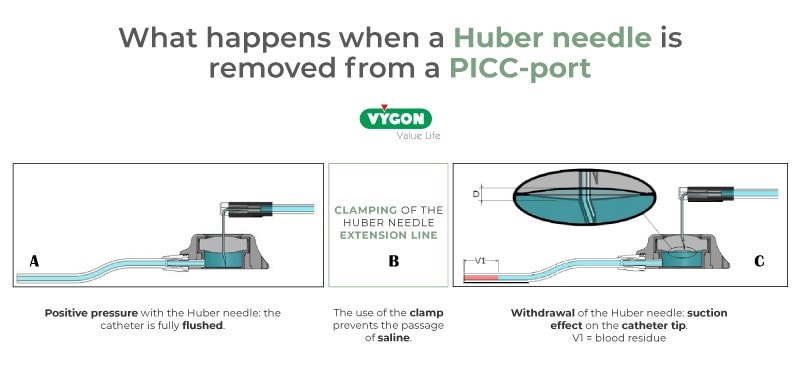
Needle withdrawal with positive pressure
In addition to flushing with positive pressure (i.e. infusing while closing the catheter clamp and before withdrawing the needle), we must bear in mind that in the case of PICC-ports and ports in general, when the Huber needle is withdrawn, a movement of the silicone in the port is made to go with the exit of the needle.
This movement can cause blood to enter the catheter, which could obstruct it, despite proper flushing of the catheter. For this reason, it is advisable to use positive pressure Huber needles which, when withdrawn, provide a minimal positive infusion of the sealing liquid that guarantees that no blood enters the catheter.
Training is a critical element for both correct placement and proper maintenance of PICC-port. Minimizing device management measures or not knowing them well can lead to increased complications.
These recommendations are very important points to achieve success with PICC-ports. They can help the healthcare professional in charge of its insertion but also the nurses responsible for the administration of intravenous treatments.
BIBLIOGRAPHY
- INS 2021 Guidelines.
- Santacruz et al. Placement of peripherally inserted central catheters (PICC) by intracavitary electrocardiographic monitoring (ECG-IC) of the catheter tip. Nutr. Hosp. 2018; 35(5): 1005-8.
- Bertoglio et.al, PICC-PORT totally implantable vascular access device in breast cancer patients undergoing chemotherapy. J Vasc Access. 2020 Jul;21(4):460-466. doi: 10.1177/1129729819884482. Epub 2019 Nov 1. PMID: 31674857.
- Bertoglio et.al, A multicenter retrospective study on 4480 implanted PICC-ports: A GAVeCeLT project. J Vasc Access. 2022 Jan 17:11297298211067683. doi: 10.1177/11297298211067683. Epub ahead of print. PMID: 35034480.



