Extravasation can be defined as the accidental leakage of a chemotherapy infusion into the subcutaneous tissues, and exceptionally into the pleura or mediastinum.
It can be an absolute therapeutic emergency depending on the product that was used. Of all the possible complications of intravenous devices, it is one that is highly feared.
The golden rule is to immediately stop any infusion at the slightest tingling, pain, burning or redness, and even more so when swelling occurs. It is important for the staff but also for patients to be aware of these signs so that they can report any abnormal events.
-
Causes of extravasation
1- Poorly assessed blood reflux
Before any chemotherapy administration, reflux assessment is crucial. It proves that the catheter is patent.
When the port or the catheter is partially obstructed, dark and thick blood is withdrawn. It is important to keep in mind that blood reflux should be brisk. If it is slow or sluggish, this would need investigating.
 Photo 1: Excellent blood reflux
Photo 1: Excellent blood reflux
Moreover, if the patient has to change positions, turn their head or raise their arm, this can imply that there is a problem. (For more information, click here to access our article on “Mechanical complications of ports”).
Blood reflux is often only obtained after a gentle injection of Nacl, which can “unblock” the sedimentation that has formed at the tip of the catheter.
Full training of users of vascular access devices (nurses, interns, etc.) in all types of situations is essential.
In the absence of clear and brisk blood reflux, we recommend refraining from any chemotherapy infusion and making a diagnosis with required tools such as radiography.
2- A misplaced Huber needle
Learning how to access a port should be a key skill for healthcare professionals and doctors that are responsible for using these devices or training new staff. Users must know how to locate the edges of the septum and stretch the skin between the thumb and the forefinger leaving the device maintained. Then, you should puncture perpendicularly using a non-coring needle and feel that it touches the bottom of the port.
 Photo 2: Firm holding of the port during puncture
Photo 2: Firm holding of the port during puncture
Some ports can be challenging to use on patients with excess body fat because they can be too small or get too deep. In this case, we recommend asking for a change of the device.
3- A cracked catheter
During insertion, it is possible for a fracture to occur in the catheter due to catheter twisting.
 Photo 3: Catheter rupture due to the cutting cannula of the port
Photo 3: Catheter rupture due to the cutting cannula of the port
Sometimes the fissure is located a few centimetres downstream while reflux is still obtained.
The most typical case is the Pinch-Off Syndrome, a catheter crushed in the costo-clavicular clamp (between the clavicle and 1st rib). To find out more about this you can click here.
 Photo 4: Pinch-Off Syndrome
Photo 4: Pinch-Off Syndrome
4- Catheter-port disconnection
Port-catheter disconnection rarely occurs and is usually due to an attempt to flush the catheter using excessive force.
 Photo 5: Catheter-port disconnection
Photo 5: Catheter-port disconnection
5- Secondary needle displacement
Secondary needle displacement can occur after a patient unintentionally pulls the infusion line, or because of a needle that is too short or loose.
6- Extravasation in the pleura
Extravasation in the pleura is exceptional and is the consequence of an error of judgement during the implantation of the catheter which was intra-pleural from the start. It is not due to the secondary displacement of the catheter. We have recently observed a case of an intra-pleural PICC-line with an extravasation without dramatic consequences.
In summary, healthcare workers who use ports should be aware of these complications. Therefore, training is crucial. It is also important to organize sessions after the training to refresh memories. Not all extravasations are due to human errors but refresher courses and a will to improve can guarantee the safe use of these devices.
-
Products involved in extravasation and the procedure:
1- Products involved in extravasation:
The severity of extravasation depends on the product involved.
These products are classified by ascending order of lesions severity:
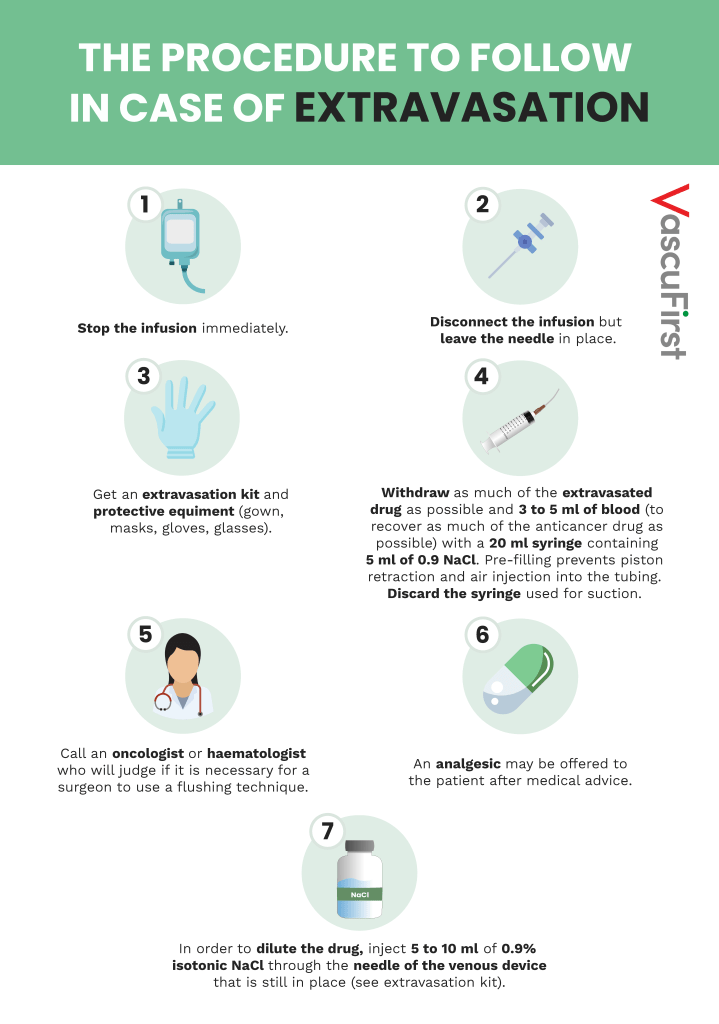
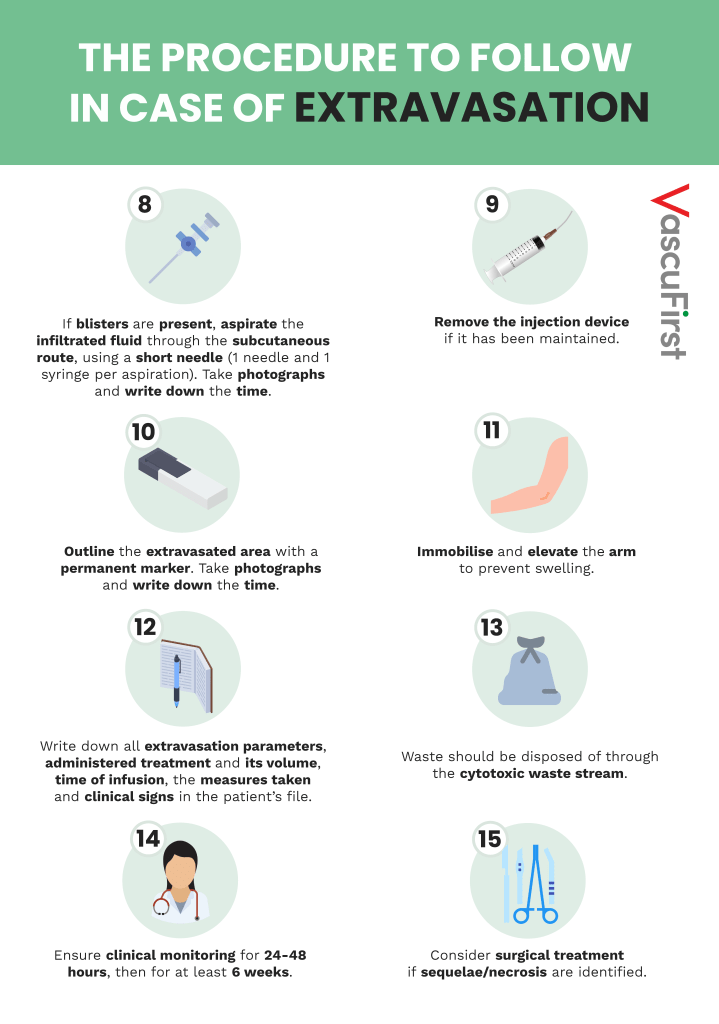
2- The procedure to follow in case of extravasation:
The procedure to follow when facing extravasation is clear no matter the product used. It is necessary to follow the steps below:
3- Extravasation kit:
Each hospital should have an Extravasation Kit that is usually stored in the pharmacy. Healthcare professionals and practitioners who apply the kit (surgeons, anaesthetists, radiologists, nurses) should be aware of its existence and have a 24-hour access to it.
In some countries such as France, the composition of the kit is as follows:
Immediate application of cold compresses is useful in an emergency. But in the case of extravasation of Vinca-Alkaloids (e.g. Vincristine), or Oxaliplatin, warm compresses should be applied.
In case of extravasation of Anthracyclines, the administration of Dexrazoxane (SAVENE) can be discussed. The protocol for administering this product will not be noted here, as it is detailed in the kit. In any case, it is necessary to act as soon as possible, and within six hours at most. If this is not possible, DMSO 99% (Dimethylsulfoxide) can be applied locally as soon as possible. 4 drops/10cm2 on both of the affected and surrounding area and for 7 days.
The following picture shows an extravasation of Anthracycline:
 Photo 10: Necrosis from Anthracycline extravasation
Photo 10: Necrosis from Anthracycline extravasation
This necrosis occurred when the infusion catheter was pulled. The pull was strong enough to dislodge the well-placed and secured needle from the port while the port remained in the subcutaneous space. This patient required flap surgery.
-
CONCLUSIONS
Chemotherapy extravasation is one of the most dreaded incidents in the patient’s life.
Unfortunately, it is often the result of a poor assessment of the blood reflux prior to catheter use, poor needle positioning or poor fixation. Extravasation can be avoided by continuous training of the staff and constant monitoring of the placement of the Huber needle.
Despite all these precautions, extravasation is still possible. Patients must be aware of the potential risks in order to prevent a secondary needle displacement due to sudden movements.
The staff must also be trained and know what to do in the event of extravasation.
BIBLIOGRAPHIE
-
Management of extravasation. INESSS (Institut National d’Excellence en Santé et en Services Sociaux), Québec, June 2014. Jim Boulanger.
-
Pharmacy of the University Hospitals of Geneva, http://pharmacie.hug-ge.ch/
-
Safe axillary-subclavian venous access, JJ Simon, VascuFirst, March 2022.
-
Mechanical complications of implantable ports, JJ Simon, Vascufirst, Oct 2022.