Enteral nutrition is the preferred method for delivering nutrients to patients who are unable to consume them orally. While it is associated with fewer complications compared to other nutritional methods, it is not entirely risk-free.
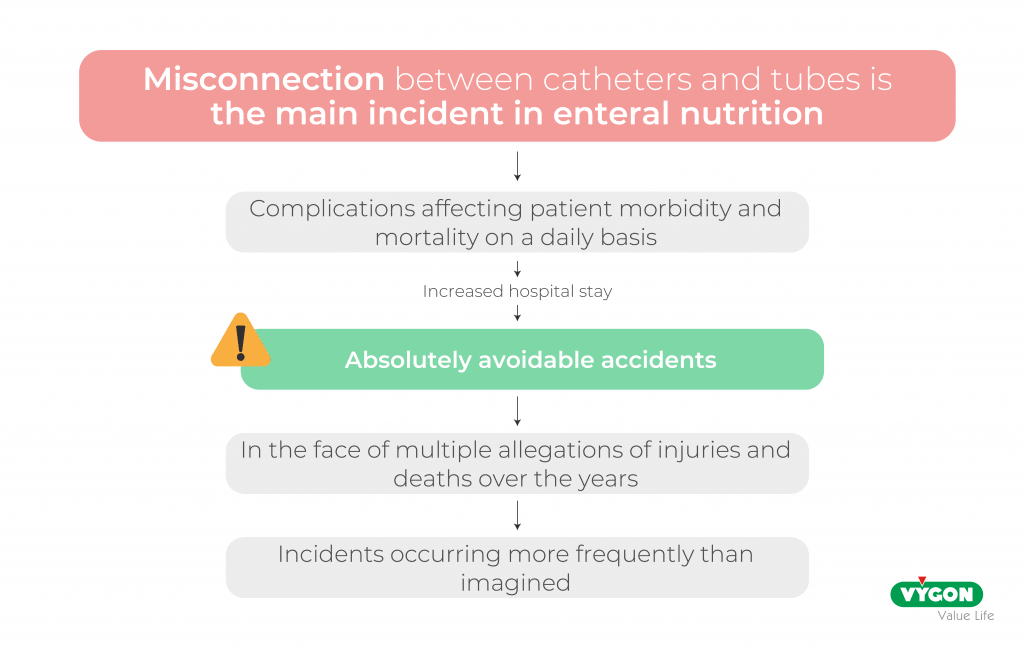
One of the most critical incidents related to enteral nutrition is potentially fatal errors in tubing connections with an IV line or the ventilation system. These misconnections can result in severe harm, including patient death. Fortunately, devices designed to prevent misconnections are available, even though these safety systems are still not widely implemented in many countries.
The prevalence of such incidents has raised significant concerns among global organizations such as the World Health Organization (WHO) and the Food and Drug Administration (FDA), prompting them to highlight the urgent need to address this issue.
With the aim of reflecting on this circumstance that endangers the safety of neonatal patients, we spoke with Rosa Collado, manager of Pediatric and Neonatal Patient Care at the Quirón Salud Group’s Hospital Universitario de Cataluña.
In the interview, Rosa explains the importance of creating a culture of safety within the NICU and the transformation that this implies in the routine procedures of the unit. In addition, she tells us about the fatal events that happened in Spain and led to the adaptation of safe connection systems for enteral nutrition. She also explains the benefits and the learning derived from this change.
You can see the complete interview via this link (only available in Spanish):
MISCONNECTION
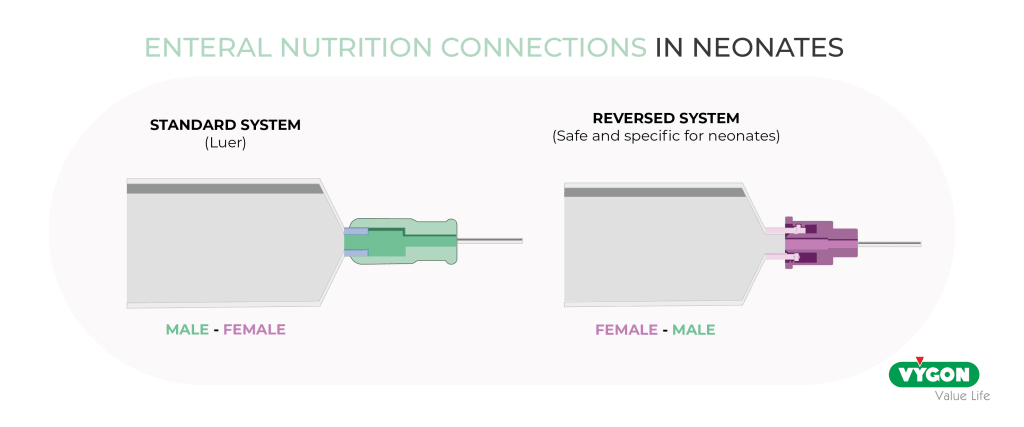
By “misconnection,” we refer to the mistake of connecting a catheter, probe, or tube from two unintended delivery systems, resulting in fluids being infused through the wrong route. Such errors are entirely preventable, as specific and secure connection systems are available to eliminate this type of mistake.
FACTORS FAVORING THE MISCONNECTION
These incidents are often the result of adverse and common circumstances in Intensive Care Units (ICUs), where several factors contribute to the likelihood of accidents:
- Frequent handling of newborns: Newborns undergo constant manipulation, which increases the risk of human error.
- Advancements in neonatal care: Medical progress has enabled the survival of infants in extremely critical conditions. However, this has led to an increase in the number of medical device connections required for these patients, along with multiple access points for different administration routes, creating opportunities for misconnection.
- High-pressure environment: Neonatal Intensive Care Units (NICUs) are high-stress environments due to the vulnerability of the patients and the frequent occurrence of sudden emergencies.
- Insufficient training: In some cases, healthcare professionals may lack the necessary education or training to care for critical patients, such as premature newborns.
- Challenging environmental conditions: Factors like poor lighting in the NICU can make it easier for certain errors to go unnoticed.
- Patient communication limitations: The inability of newborns to communicate errors further increases the risk of mistakes.
Human errors and system failures are unavoidable, making it essential to establish safeguards such as protocols and the adoption of safety devices. These measures aim to foster a culture focused on error prevention rather than error correction, as the consequences of some mistakes cannot always be rectified.
Such consequences can have a direct impact on patient morbidity and mortality, leading to embolisms, sepsis, acute cardiac and respiratory failure, permanent neurological damage, and even death.
THE RYAN CASE, THE FATAL ERROR THAT PROMPTED THE CHANGE TO SAFE CONNECTIONS FOR ENTERAL NUTRITION
In Spain, the use of safe connection systems designed to prevent the administration of fluids through incorrect routes is now widespread and standardized through established protocols. However, this shift toward a culture of safety and the adoption of specific connectors was driven by a tragic event known as the Ryan Case.
The story of little Ryan captured the attention of the public, media, and policymakers for months. Ryan’s mother, who was 29 weeks pregnant, became the first pregnant woman in the country to contract Influenza A. She gave birth prematurely to Ryan, who was extremely vulnerable due to his young age, and tragically passed away shortly thereafter. Days later, a sequence of preventable events led to Ryan’s death as well.
At the Gregorio Marañón Hospital in Madrid, where Ryan was being treated for his prematurity, an emergency occurred in a room adjacent to his. The specialized staff in the unit were occupied addressing this crisis. In response to the high-pressure situation, a nurse from another department volunteered to assist with the care of the remaining patients, including Ryan.
This nurse was supposed to connect an enteral nutrition to Ryan but mistakenly connected it to an intravenous line, a fatal error that ultimately led to the patient’s death.
At that time, only the individual error was taken into account, and the nurse was accused of medical negligence, without considering that the hospital did not have the protocols and specific safety devices that would have made it possible to avoid human error.
IMPLEMENTATION OF A SAFETY AND SPECIFIC CONNECTION SYSTEM
This incident led to the mobilization and awareness of public opinion and healthcare professionals. Many professionals were already aware that misconnections could occur, as literature highlighting the consequences of such errors had existed since the 1970s. Furthermore, testing methods to prevent these errors had been developed, but these methods were not infallible.
The lack of reliable safety measures also affected the confidence of healthcare professionals, creating an additional obstacle to effective patient care.
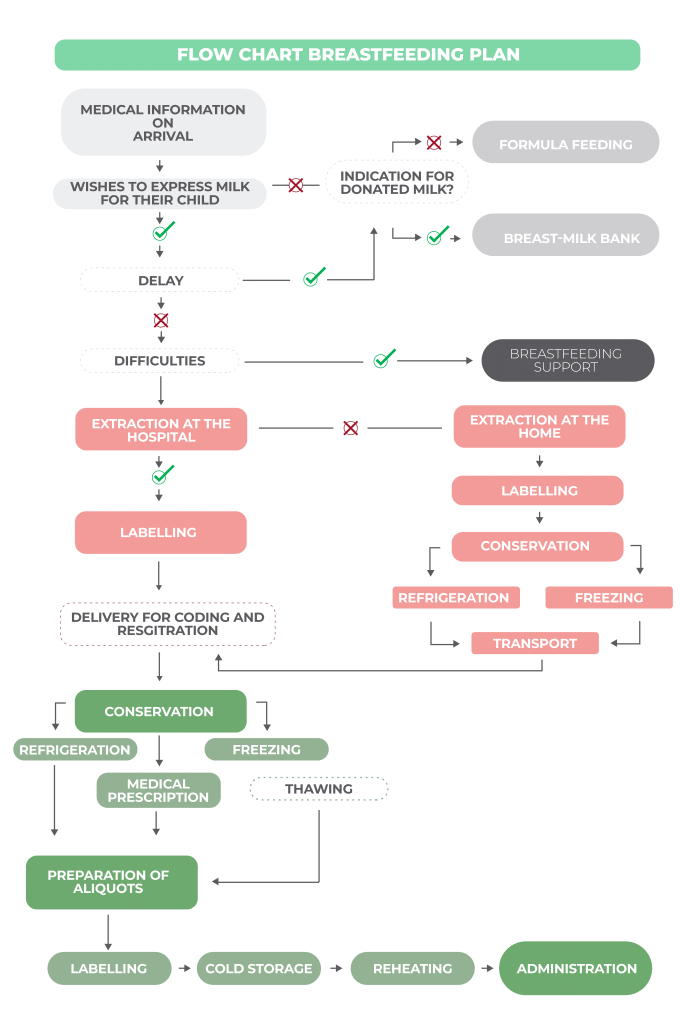
This turning point underscored the critical importance of using safety connection devices in neonatal units. Some units have even begun adopting more advanced systems that not only meet safety standards but also address two additional key requirements: meeting the specific preterm patient needs and ensuring accuracy in the dose administration.
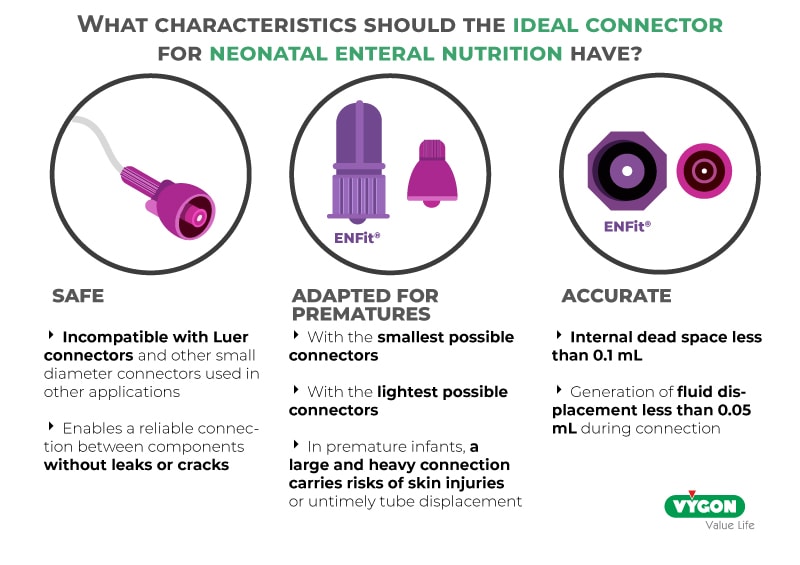
This shift marked a pivotal step toward fostering a culture of safety. As with any change, there has been a learning curve; however, it has been relatively smooth. The teams responsible for enteral nutrition quickly recognized the advantages of these changes in terms of both workflow efficiency and patient safety.
The implementation of these safety devices has also driven the development of new protocols, created through collaboration among all professionals involved in the enteral nutrition process. These protocols have proven especially valuable for new staff members, helping them adapt to the unit’s practices and routines. They also serve as a reliable reference to address any uncertainties that may arise during their work.
SAFETY CULTURE IN THE NICU
Professionals are increasingly taking an active role in fostering a culture of safety within their units. The introduction of specialized roles, such as safety reference nurses, has significantly enhanced the knowledge, training, and application of scientific evidence among healthcare teams. These advancements have translated into meaningful improvements in clinical practice. Moreover, the presence of these roles has helped cultivate a culture of openness and accountability regarding errors. By encouraging the acceptance and reporting of mistakes, healthcare teams can learn from them and implement the necessary safeguards to prevent their recurrence.
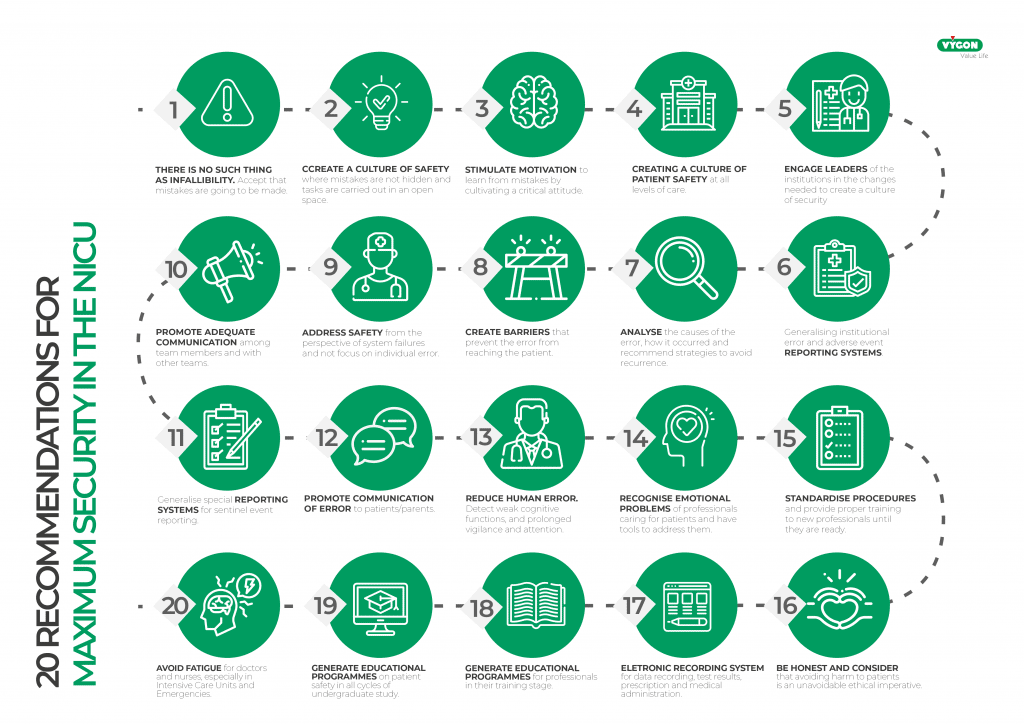
However, it is important to continue this work and to oblige all healthcare professionals to be committed to patient safety, without relying on fixed working methods dictated by routine or economics.
The team that works with patients on a daily basis is best placed to understand the specific needs of the unit. It is up to them to implement the necessary changes, using the literature, scientific evidence and real-life experience of the NICU.
It’s crucial not to become overwhelmed by the familiarity of everyday life, because healthcare practice and knowledge must constantly evolve. Adopt a culture of safety in your department and focus on the use of safe, specific devices for administering enteral nutrition to newborns!





