Occlusion is one of the most common complications associated with vascular access devices (VADs). A blocked device can interrupt treatment, preventing the delivery of essential medications, fluids, or nutrition. This can lead to a rapid deterioration in the emergency patient’s condition as well as the development of other complications such as infections.
Preventing occlusions is crucial for ensuring patient safety, reducing discomfort, and minimizing anxiety. Prevention not only helps maintain treatment efficacy but also reduces the need for unnecessary interventions.
This article focuses specifically on port occlusion. It covers its types and signs, then provides essential best practices to help reduce the risk of complications.
Read on to learn about how to mitigate the risk of port occlusion.
Types of port occlusion
When a catheter is patent, it allows for free flushing and aspiration without resistance. Occlusion can however present in two key ways:
- Partial occlusion: the presence of sluggish flow.
- Persistent withdrawal occlusion: ability to flush but inability to aspirate from the catheter.
- Total occlusion: inability to flush or aspirate from the catheter.
Signs of port occlusion
Signs of occlusion include:
- A sluggish blood return,
- Inability to flush freely,
- Sluggish flow,
- Resistance felt on flushing,
- Inability to infuse fluids or medications,
- Frequent alarms indicating occlusion,
- Swelling at insertion site,
- Leakage at insertion site.
How to prevent port occlusion
To reduce occlusive complications in ports and maintain the safety of the patient, the following ten practice points should be considered:
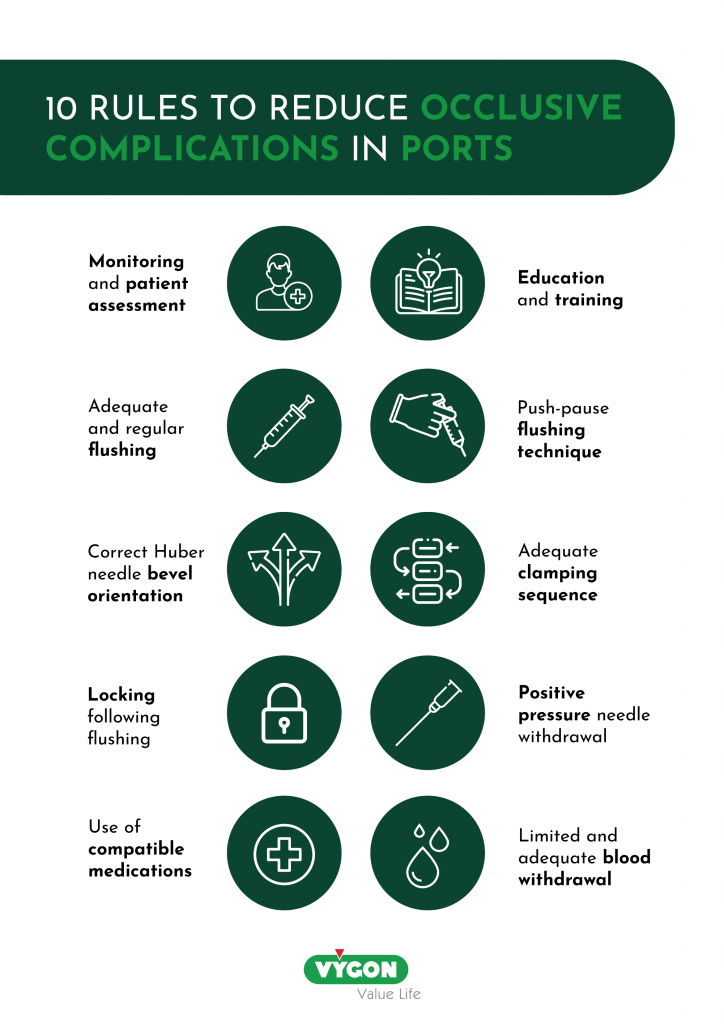
Monitoring and patient assessment
The patient should be monitored regularly for signs of occlusion. Early detection of occlusion can prevent further complications, such as infections.
Recommendations:
- Regular monitoring and maintenance of the port can identify any problems before they become severe, which can help to prevent occlusions and other complications.
- Adequate hydration and nutrition levels help to maintain the conditions necessary for the prevention of port occlusion.
- Proper positioning can prevent kinking or pressure on the catheter, which can cause occlusion.
- Adhere to the care plan as recommended by the healthcare team to ensure that the port remains functional.
Education and training
There is evidence to suggest that appropriate education and training for HCP who work with VAD can improve patient outcomes13. It is indeed important that HCP adhere to practice guidelines when accessing and flushing VADs. This approach can improve safety and reduce the incidence of catheter related complications, such as occlusion10.
Recommendations:
- Establish protocols to ensure that flushing and locking procedures are standardised across institutions.
- Follow the manufacturer’s protocol and IFUs for the use and care of ports. This will help to maintain the integrity of the device and help to prevent device occlusion.
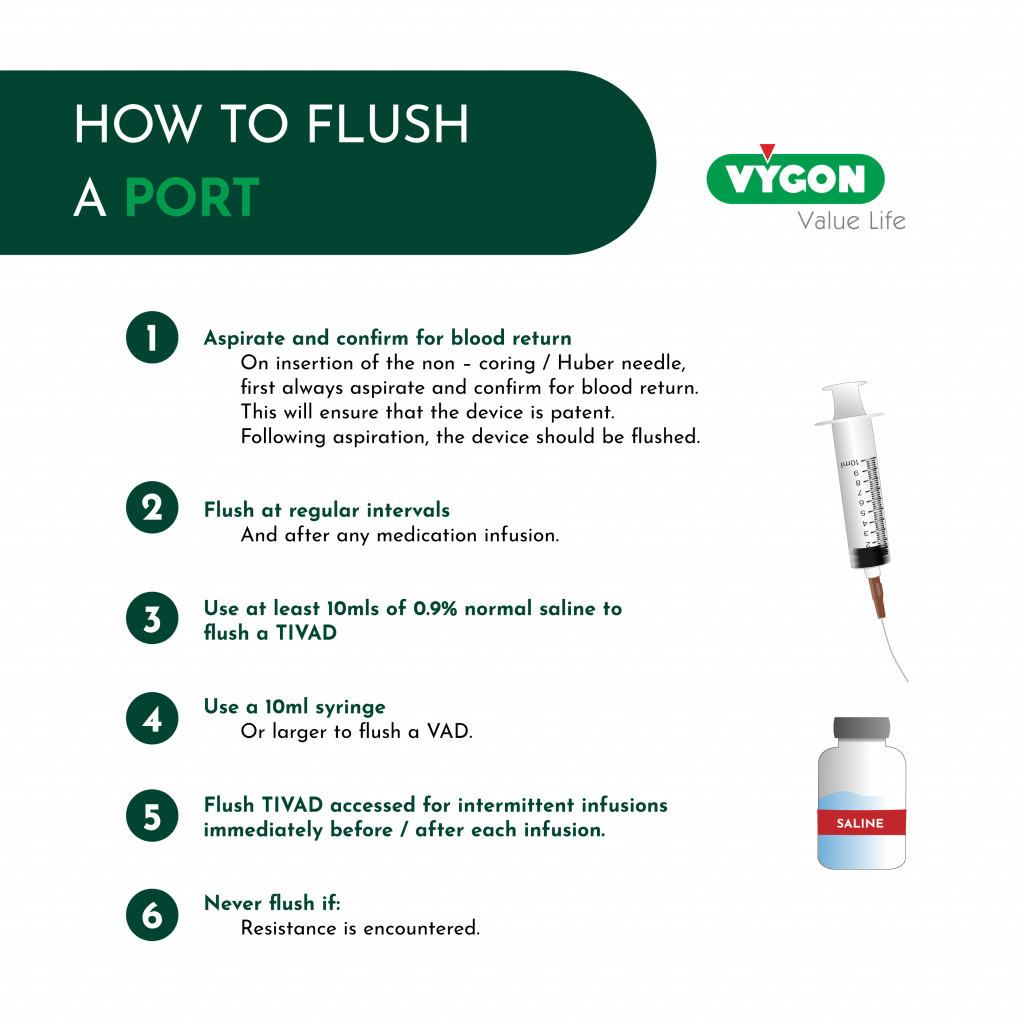
Adequate and regular flushing
Adequate and regular flushing is one of the key practice points to help prevent occlusion. This involves using a saline solution to clear the device of any residue and to prevent blood and biofilm from building up within the device.
Effective flushing technique
The act of flushing, or clearing, when performed correctly, represents a key procedure in maintaining device patency and reducing the risk of occlusion16.
Recommendation:
Use a push – pause, pulsatile turbulent flush as this technique helps to clear the catheter and port of biofilm.
A pulsatile flush involves a fast stop – start or push – pause technique as the saline is injected into the catheter. Research demonstrates that the turbulence created within the catheter is more effective in rinsing the catheter lumen and port compared to a constant, laminar injection17. This technique is also associated with a reduction in bacterial attachment and growth in VADs3.
Huber needle bevel orientation
When flushing a port, the bevel of the non-coring / Huber needle should be orientated in the opposite direction from the outflow channel where the catheter is attached to the port body. The evidence for this was demonstrated in In vitro testing that confirmed that a greater amount of protein was removed when the bevel was orientated in this direction8.
Correct clamping sequence
The sequence in which the port is clamped is important in the fight to reduce catheter occlusion. The sequence of clamping and syringe disconnection is dependent on the type of needle free device in situ. Therefore, it is fundamental that HCP are aware of this information prior to working with VADs.

Locking
Locking refers to the installation of fluid into the lumen of a catheter following flushing6. This is in the attempt to maintain catheter patency or to reduce infective risks. Types of locking solutions include saline, heparin, antibiotics, thrombolytics, citrate, ethanol, and bicarbonate solutions14.
Traditionally, heparin was used as a locking agent for most VADs. Recently however, a meta – analysis concluded that there was little high-quality evidence to suggest that the use of heparin to lock VAD reduced the incidence of occlusions. In addition, there was no evidence that the use of heparinised saline resulted in fewer VAD occlusions11. Guidance from the National Institute for Health and Care Excellence (NICE) suggest that a sterile 0.9% injection to flush and then lock the catheter is adequate15.
Positive pressure needle withdrawal
The withdrawal of Huber needles from a port can cause blood to reflux into the tip of the catheter which can result in intraluminal occlusion. When the Huber needle is removed from the port body, the septum is slightly lifted. When the septum returns to its original position this causes a small influx of blood at the catheter tip. This has been demonstrated in a study by Lapalu (2010).
In this study, the application of positive pressure (achieved by the injection of additional solution) during Huber needle withdrawal reduced the incidence of reflux by nearly 80%. This study demonstrated the value of positive pressure needle withdrawal to reduce reflux, compared to turbulent flushing and a positive pressure clamping sequence alone.
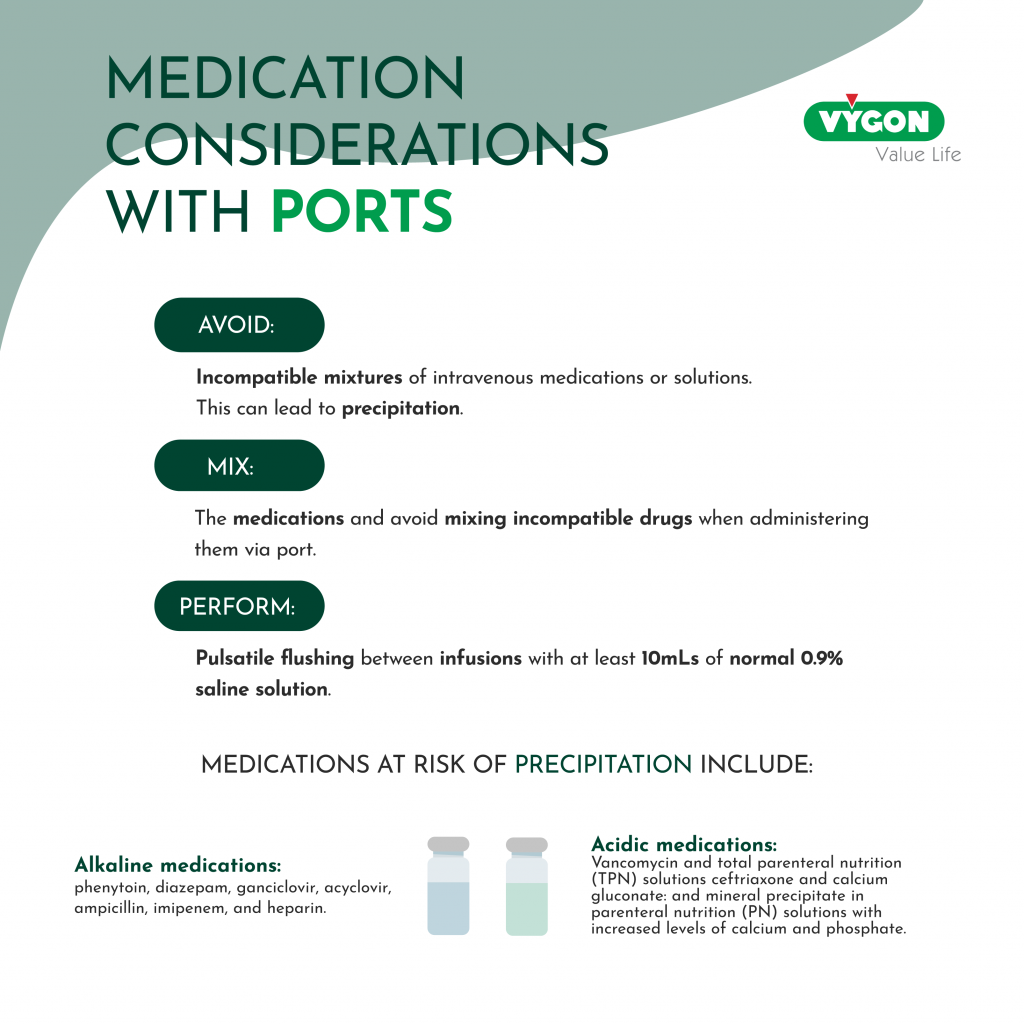
Medication considerations
Blood withdrawal
- Limit the number of blood draws to the necessary minimum, as each access increases the risk for infection or occlusion.
- Adequate flushing and locking following blood withdrawal is crucial to help prevent occlusive complications.
- Flush the port with at least 20mls of 0.9% normal saline, using a turbulent flush technique, following blood withdrawals.
There are many effective ways to prevent occlusions in ports. By implementing the ten practice points detailed in this article, HCP can ensure that the device remains patent. Subsequently, patients can experience optimal outcomes and avoid the potential ramifications of port occlusion.
References
- Cia-Arriaza M, Cabrera-Jaime S, Cano-Soria R, Manzano-Castro M, Domínguez-Gómez M, Prieto-Arenas DM, Benito-Yagüe A, Sánchez-Martín A, González-Alonso C, Fernández-Ortega P. Evidence on port-locking with heparin versus saline in patients with cancer not receiving chemotherapy: A randomized clinical trial. Asia Pac J Oncol Nurs. 2022 May 21;9(9):100085. doi: 10.1016/j.apjon.2022.100085. PMID: 35935884; PMCID: PMC9345785.
- Denton et al. Royal College of Nursing. Standards for infusion therapy. 2016. http://tinyurl.com/y2le48zm (accessed 13 June 2023)
- Ferroni A, Gaudin F, Guiffant G, Flaud P, Durussel JJ, Descamps P, Berche P, Nassif X, Merckx J. Pulsative flushing as a strategy to prevent bacterial colonisation of vascular access devices. Med Devices (Auckl). 2014;7:379–83.
- Goossens GA, Jérôme M, Janssens C, Peetermans WE, Fieuws S, Moons P, Verschakelen J, Peerlinck K, Jacquemin M, Stas M. Comparing normal saline versus diluted heparin to lock non-valved totally implantable venous access devices in cancer patients: a randomised, non-inferiority, open trial. Ann Oncol. 2013;24(7):1892–9.
- Goossens GA. Flushing and locking of venous catheters: available evidence and evidence deficit. Nurs Res Pract. 2015;2015:985686.
- Gorski LA, Hadaway L, Hagle ME, Broadhurst D, Clare S, Kleidon T, Meyer BM, Nickel B, Rowley S, Sharpe E, Alexander M. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021 Jan-Feb 01;44(1S Suppl 1):S1-S224. doi: 10.1097/NAN.0000000000000396. PMID: 33394637.
- Guiffant G, Durussel JJ, Flaud P, Vigier JP, Merckx J. Flushing ports of totally implantable venous access devices, and impact of the Huber point needle bevel orientation: experimental tests and numerical computation. Medical Devices (Auckland, N.Z.). 2012 ;5:31-37. DOI: 10.2147/mder.s30029. PMID: 23166455; PMCID: PMC3500975.
- Guiffant G, Durussel JJ, Merckx J, Flaud P, Vigier JP, Mousset P. Flushing of intravascular access devices (IVADS)—efficacy of pulsed and continuous infusions. J Vasc Access. 2012B;13(1):75–8.
- Jabaley T, Xiong N, Conley S, Mazeika T, Johnson D, Biggins BA, Hilton N, Hong F. Transitioning from heparin to saline locks for central venous access devices in oncology: An evidence-based practice approach. Can Oncol Nurs J. 2022 Apr 1;32(2):286-293. doi: 10.5737/23688076322286293. PMID: 35582245; PMCID: PMC9040787.
- Krzywda EA, Andris DA. Twenty-five years of advances in vascular access: bridging research to clinical practice. SAGE J; 2005.
- López-Briz E, Ruiz Garcia V, Cabello JB, Bort-Martí S, Carbonell Sanchis R, Burls A. Heparin versus 0.9% sodium chloride locking for prevention of occlusion in central venous catheters in adults. Cochrane Database Syst Rev. 2018 Jul 30;7(7):CD008462. doi: 10.1002/14651858.CD008462.pub3. Update in: Cochrane Database Syst Rev. 2022 Jul 18;7:CD008462. PMID: 30058070; PMCID: PMC6513298.
- Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto J, Wilcox M, UK Department of Health. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014 Jan;86 Suppl 1:S1-70. doi: 10.1016/S0195-6701(13)60012-2. PMID: 24330862; PMCID: PMC7114876.
- Moureau NL. Safe patient care when using vascular access devices. Br J Nurs. 2013;22(1):S14–21.
- Moureau et al (2019) Vessel Health and Preservation: The Right Approach for Vascular Access. Vessel Health and Preservation: The Right Approach for Vascular Access | SpringerLink. (Accessed 13th June 2023)
- National Institute for Health and Care Excellence (NICE) Infection prevention and control 2014. Quality statement 5: Vascular access devices | Infection prevention and control | Quality standards | NICE (accessed 13th June 2023)
- Royon L, Durussel JJ, Merckx J, et al. The fouling and cleaning of venous catheters: a possible optimisation of the process using intermittent flushing. Chem Eng Res Des. 2012;90(6):803–7.
- Vigier JP, Merckx J, Coquin JY. The use of a hydrodynamic bench for experimental simulation of flushing venous catheters: impact of the technique. ITBM-RBM. 2005;26(2):147–9.







