Ever since their creation, vascular access teams dedicated to PICC placement have proven to be efficient in reducing catheter-related complications. However, as Nancy Moureau commented in a clinical case on thrombosis in 2016, there are still complications that can become very serious.
Among the adverse issues that can occur with a PICC catheter, partial or total loss of patency is very common. Despite often being asymptomatic, they are still incidents whose consequences can put the patient’s treatment and health at risk.
Therefore, it is key to know what causes a PICC malfunction when administering intravenous therapy.
OBSTRUCTION
Definition
PICC occlusion is one of the most common complications and can lead to serious consequences: the catheter can be unusable which can delay treatment and, in the worst case, make it necessary to remove and/or replace it.
As it is a long catheter with a reduced diameter when compared to a central catheter, the probability of obstruction is higher if the maintenance of the device is not conducted correctly.
Signs of an occlusion
PICCs can lead to 2 types of occlusions:
- Partial: checking for blood reflux is difficult or impossible but infusion through the catheter is possible
- Total: inability to obtain blood reflux and to inject substances through the lumen of the vascular access
Causes
PICCs can be obstructed by an internal clot, thrombus from the vein, or a fibrin sleeve formed in the catheter. The cause of the occlusion can have several origins:
- Improper maintenance: insufficient flushing and/or incorrect technique, improper sealing, or improper disconnection of Luer systems can result in blood or drug residues.
- A traumatic insertion and/or one that took place after a longer time
- A misplaced catheter tip (the PICC tip must be located in the lower 1/3 of the vein)
- Other factors may come into play: related to the patient (advanced age, obesity, coagulation status) and the type of drug
Prevention
Training of the nursing staff who handles PICCs is particularly important in this case. The vascular access team is responsible of ensuring adequate and continuous training to achieve the best possible level of prevention among all the professionals involved.
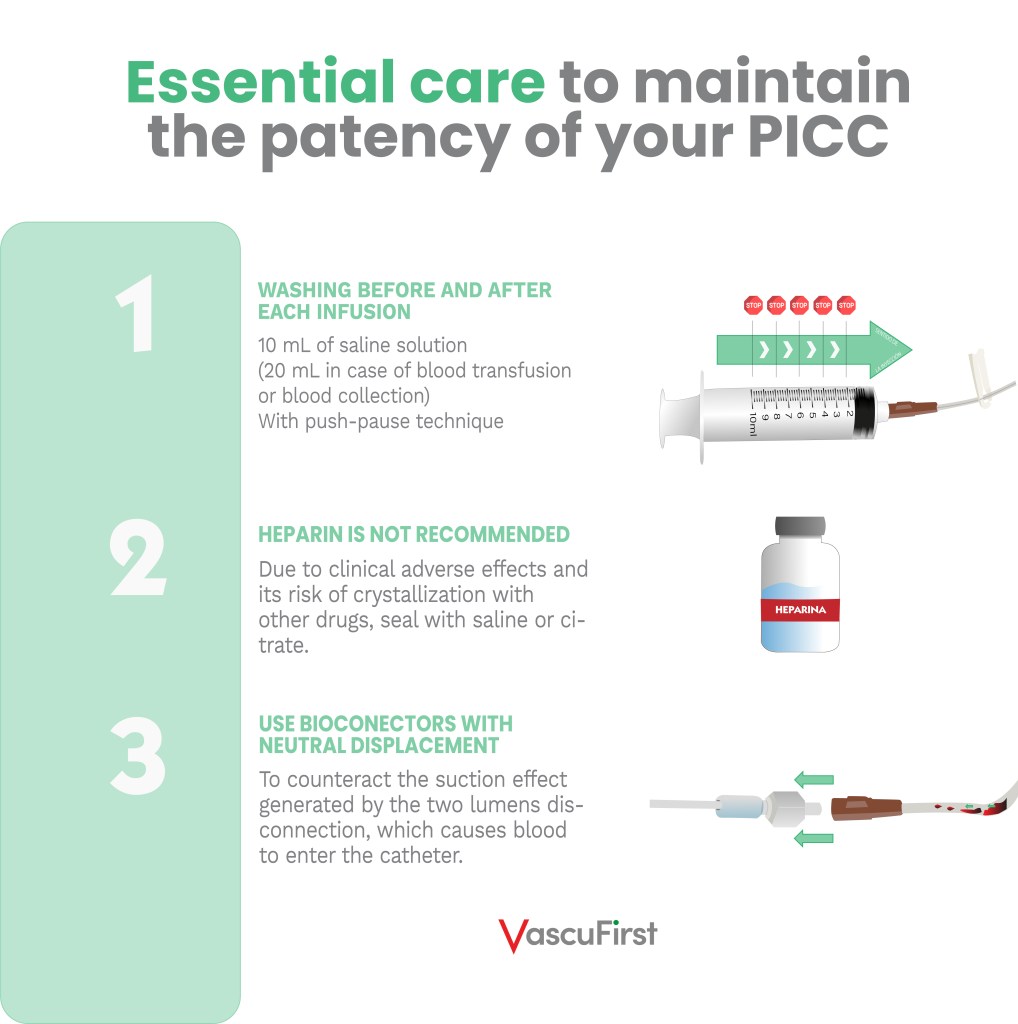
To maintain the patency of the catheter, some simple but important guidelines must be followed:
It is important to note that to avoid obstruction of the pathway by thrombus, it is important to meet the criteria below:
- An adequate placement of the device
- Minimal invasiveness
- A correct location
It is also important to assess whether the use of a multi-lumen PICC catheter is essential. Using this type of device means administering therapies through smaller lumens and consequently, with a higher probability of occlusion.
THROMBOSIS
Definition
Thrombosis consists of the formation of a clot in a vessel and consequently reducing its flow or completely preventing blood circulation. It can be particularly serious when the thrombus migrates which can lead to pulmonary embolism.
The thrombus forms because of the endothelial damage created during PICC placement.
There are several ways to classify catheter-related thrombosis. It can be by location and severity:
- Superficial (or proximal) venous thrombosis when the affected vessels are shallow, such as those of the upper and lower limbs.
- Deep (or distal) vein thrombosis when the affected vessels are deep, such as the subclavian vein, the brachiocephalic trunk or the superior vena cava.
Thrombosis can also be classified in another way which takes into account the catheter:
“CVC-associated thrombosis can be classified into three types based on the location of thrombus formation:
– Pericatheter thrombosis
– Thrombotic obstruction of the catheter lumen
– Mural thrombosis, either superficial (SVT) or deep (DVT)”
Signs and symptoms of a thrombosis
Thrombus can cause the same patency problems as catheter occlusion seen above. In most cases, when there is a malfunction of the device, the distal thrombosis (i.e., located near the tip of the catheter) causes a PWO (Persistent Withdrawal Occlusion). It still allows the injection of solutions and drugs.
However, it should be noted that thrombosis is silent in 60% of affected patients
When it comes to an occlusive or extensive thrombosis, the patient may suffer from the following symptoms:
- Edema in the arm (or shoulder)
- Erythema
- Ipsilateral pain (arm, shoulder, neck, face corresponding to the side of the catheter)
- Collateral circulation
- Symptoms of SVC obstruction
- Difficulty drawing blood from the catheter
Causes
Regarding catheter-related thrombosis, the GAVeCeLT Reference group explains the causes of its appearance as follows:
“Catheter-related thrombosis means that the section in which the catheter is inserted presents a venous thrombosis due to an endothelial injury caused by the penetration of the catheter into the vein or by the mechanical and/or chemical trauma caused by catheter tip on the endothelium.”
According to Virchow’s triad, the risk factors for thrombosis are divided into 3 types:
Prevention
As thrombosis is due to endothelial trauma caused by the insertion of the vascular access device, it is vitally important to be clear about the vascular access decision protocol and proceed with placement using an appropriate technique:
- Choose a catheter whose diameter represents 1/3 of the lumen of the vein. It has been shown that the more space the catheter occupies in the vein, the higher the risk of thrombosis. There is currently a debate regarding the catheter diameter/venous calibre ratio: the American recommendations speak of 45% which has been recently supported by a study by the AVATAR group. While the European guidelines speak of 33% according to the Menéndez study, it is essential to follow this guideline in paediatrics.
- Be as non-invasive as possible when placing the device, choosing the best possible vein and puncture site (ultrasound is an essential tool)
- Check the correct location of the tip with an intraprocedural method, ECG being preferable
- Make sure that the device is correctly fixed. Extensive literature supports subcutaneous anchorage and shows that it is the most effective system in this regard.
FIBRIN SLEEVE
A fibrin sleeve is cells and debris that form and overlay a catheter at least after several days.
Signs of presence of fibrin sleeve
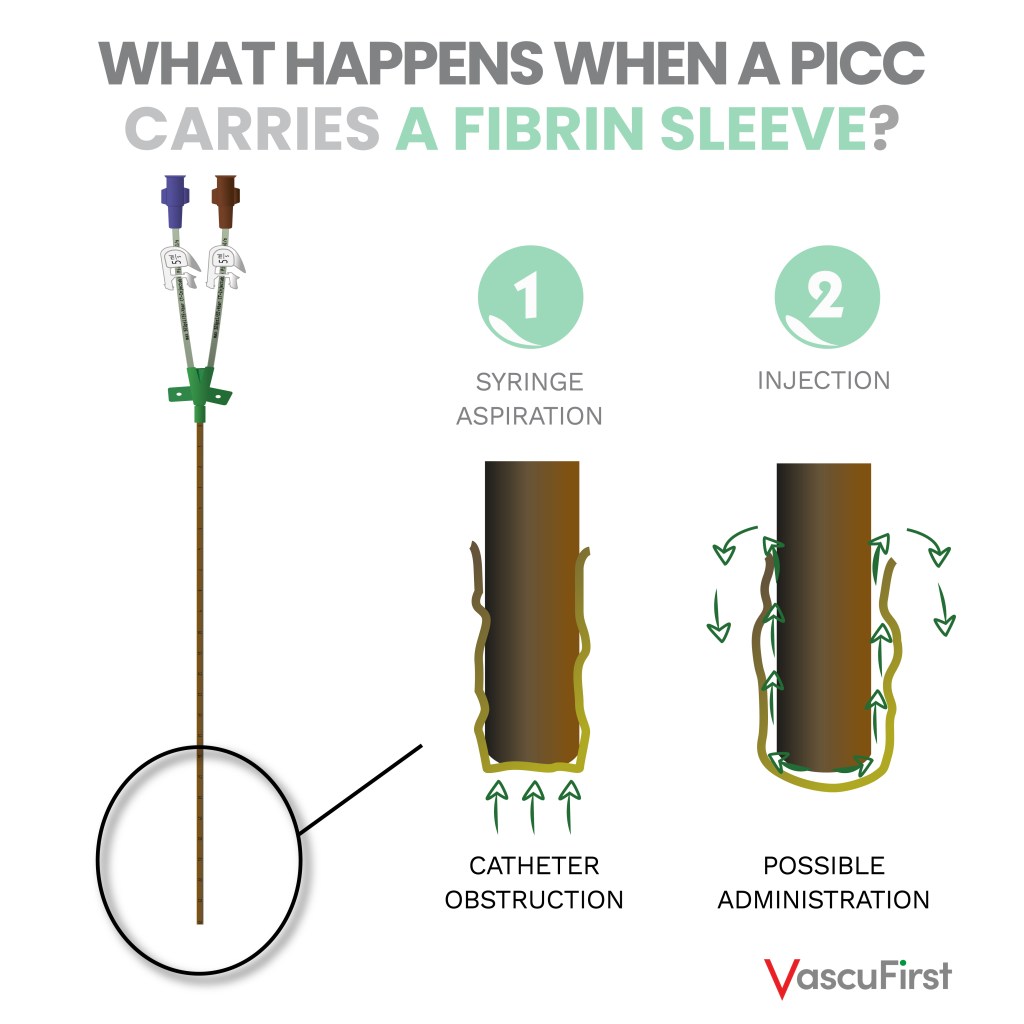
A fibrin sleeve appears when a layer covers the external part of the catheter and its tip, causing a PWO. When aspirating, the sleeve occludes the PICC and when injecting the solution circulates as follows:
Causes
It is the pathophysiological response of the organism to a foreign body, in this case the catheter.
Prevention
There is no method to prevent the formation of a fibrin sleeve as it is a reaction to a foreign body.
The use of heparin or thrombolytics to solve it is completely useless: the sleeve is made up of connective tissue (fibronectin and fibroblasts), it is not a clot.
However, the GAVeCeLT manual proposes recommendations to reduce the risk of fibrin sleeve:
– Avoid the use of valved PICCs: the valve located at the end of the catheter can cause further dysfunction by easily interfering with the fibrin sleeve
– Ensure the correct positioning of the catheter tip: in general, PICCs with dysfunction regarding their patency due to the fibrin sleeve are too short or poorly positioned.
To guarantee the maintenance of patency and therefore the proper functioning of the catheter, the correct placement technique is essential. But do not forget that catheter care is just as important. The training of nursing staff not specialized in vascular access is a key point to anticipate these problems.
A very interesting piece of information given by the Grau et.al study on complications in PICCs suggests that complications are higher in the hospital than at home with this type of device.
As the PICC is a resource that has been used for years in a multitude of hospital centres, vascular access teams have shown that when a proficient level of training is achieved, the benefit is twofold:
– The patient does not suffer delay in treatment or (worse) collateral damage.
– The nurses in charge of maintaining the catheter do not waste time unblocking the line with the additional costs that this entails.
Bibliography
-
Nancy Moureau, Preventing PICC Complications: Whose Line Is It? Patient Safety Network, AHRQ web, december 2012 – consultation made in september 2021
-
Michigan Hospital Medecine Safety Consortium, The C.L.O.T tool for identifying strategies to prevent PICC catheter occlusions – 2018
-
SEOM, Profilaxis y tratamiento de la trombosis asociada a catéter venoso central – 2017
-
Rooden, Risk assessment of thrombosis associated with central venous catheters, thesis doctoral, Leiden University – february 2006
-
GAVeCeLT manual on PICC and midline, Edra Edition – 2016
-
Steele et.al, Cutting peripherally inserted central catheters may lead to increased rates of catheter-related deep vein thrombosis, Journal of Infusion Nursing – Nov-december 2014
-
Blann et. al, How a damaged blood vessel wall contibutes to thrombosis and hypertension, Pathophysiol Haemost Thromb – September 2004, December 2004
-
Sharp et.al, 2021, Catheter to vein ratio and risk of peripherally inserted central catheter (PICC)-associated thrombosis according to diagnostic group: a retrospective cohort study, BMJ Open – july 2021
-
Menéndez et.al, Incidence and risk factors of superficial and deep vein thrombosis associated with peripherally inserted central catheters in children, J Thromb Haemost – october 2016
-
Mogi et.al, Fibrin sheath of a peripherally inserted central catheter undepicted with gray-scale (real-time B-mode) ultrasonography: A case report, Radiol Case Rep. – june 2018
-
Grau et.al, Complications with peripherally inserted central catheters (PICCs) used in hospitalized patients and outpatients: a prospective cohort study, Antimicrob Resist Infect Control. – january 2017