
Haemodynamic monitoring is essential in paediatric peri-operative and critical care medicine, guiding adequate tissue perfusion and oxygen delivery in the most vulnerable patients. Although basic parameters in paediatric anaesthesia such as heart rate, blood pressure, and pulse oximetry play an essential role in routine peri-operative monitoring, their ability to accurately reflect Cardiac Output (CO) and global perfusion is limited.
Children, particularly neonates and infants, differ significantly from adults in cardiovascular physiology.
- Their cardiac reserve is limited due to:
- Immature myocardium
- Reduced compliance
- Greater dependency on heart rate to maintain cardiac output
- Traditional vital signs are often poor surrogates for perfusion status:
- Normal blood pressure does not guarantee adequate CO or tissue oxygenation
- Tachycardia may reflect pain, fever, or stress rather than hypovolemia, only to name a few
Consequently, advanced haemodynamic monitoring and CO assessment are invaluable tools in guiding timely and precise interventions in the peri-operative period as well as later on in the PICU.
Strong reasons why extended cardiovascular monitoring including CO is recommended are:
- Direct assessment of systemic perfusion
- Early detection of circulatory instability before overt clinical signs appear
- Quantitative guidance for fluid therapy and/or vasoactive medication
- Evaluation of oxygen delivery relative to metabolic demand
The aim is not simply to optimise numbers but rather to individualise haemodynamic management, to prevent organ dysfunction, and improve outcomes.
Not every child requires extended cardiovascular monitoring. Extended CO monitoring is indicated in paediatric patients at risk of haemodynamic compromise, particularly when clinical assessment is insufficient or therapeutic decisions require precise data i.e. patients with significant comorbidities and/or patients undergoing major surgery where blood loss is possible or major haemodynamic instability could happen.
The following group of patients benefit from advanced haemodynamic monitoring: children suffering from congenital or acquired heart disease, septic shock or distributive shock, severe dehydration with ongoing fluid losses, patients with pulmonary hypertension, organ failure or multiorgan dysfunction, persistent hypotension or unexplained metabolic acidosis or undergoing major surgery.
Advanced Haemodynamic Monitoring is Highly Valuable in Children With:
Peri-operatively, cardiac output monitoring helps to optimise preload and afterload and detect haemodynamic deterioration at an early stage.
In the PICU, it supports tailored management of critically ill children with dynamic physiological changes. Particularly, neonates and infants benefit due to unstable physiology, narrow safety margins, and high vulnerability to fluid overload, especially in conditions like necrotising enterocolitis or diaphragmatic hernia repair.
Methods To Measure Cardiac Output
There are several methods to measure cardiac output.
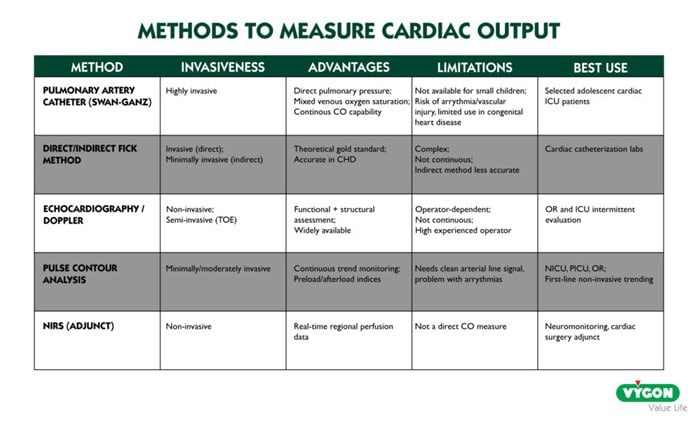
Looking specifically at newborns, infants and children, most of the practitioners are looking for less or non-invasive methods not to induce additional harm while using invasive methods or additional central catheters in those vulnerable patients.
Therefore, Pulse Contour Analysis methods like the PRAM (Pressure Recording Analytical Method) are highly interesting in this patient cohort. PRAM is a non-calibrated, beat-to-beat haemodynamic monitoring technique used to estimate cardiac output (CO) and other advanced haemodynamic parameters. The method uses the relationship between pressure variations and volume changes in the arterial system, integrating waveform shape, amplitude, and frequency content. It belongs to the family of pulse contour analysis technologies, but with a key difference.
PRAM does not require external calibration (e.g., thermodilution), making it extremely useful in paediatrics where invasive calibration methods are often limited. PRAM requires only an arterial line (i.e. radial or femoral) which is routinely placed in critically ill children or before major surgery. Unlike other arterial waveform systems PRAM is totally independent from any algorithm calibration with pre-estimated patient data or empirical constants. Its technology, based on the perturbation theory, allows clinicians to assess in real-time what is happening to the patient in that exact moment, taking information only from its arterial blood pressure waveform.
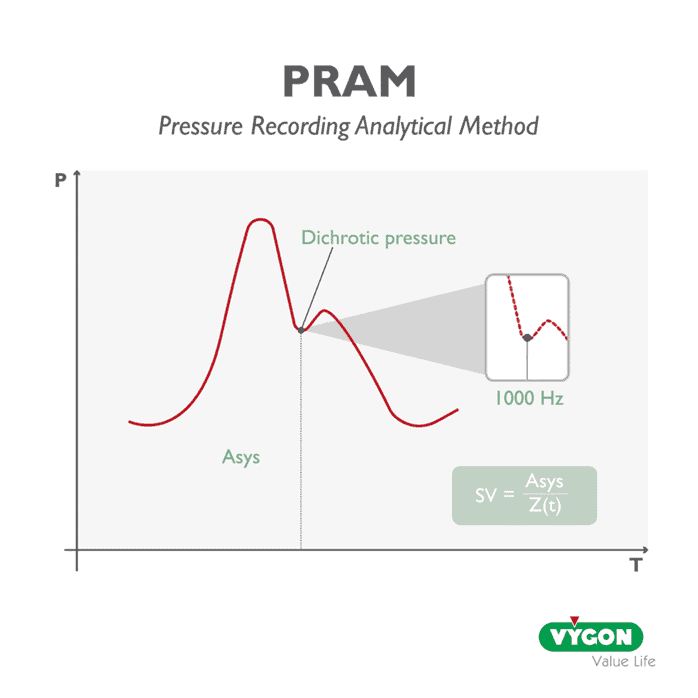
Despite the need for reliable arterial access and high-quality waveforms, it remains a highly attractive option in paediatrics, where minimising invasive techniques is crucial.
About the Author

Prof. Ehrenfried Schindler was elected to become the first Professor for Paediatric Anaesthesia in Germany on October 2019 at the University of Bonn. Before, he was head of the department for paediatric anaesthesia and later medical director at the Children’s Hospital of Sankt Augustin in Germany for 17 years. Prof. Schindlers main interest is care for critically ill children. His research focus on anaesthesia for children with congenital heart defects and the peri-operative setting. Additionally, he was one of the pioneers in introducing ERAS (enhanced recovery after surgery) strategies and ultra-fast track anaesthesia after operations with cardiopulmonary bypass in Germany. Besides that, he was hon. Treasurer and later President of the European Society for Paediatric Anaesthesiology (ESPA). Moreover, he is a well-known lecturer at scientific meetings in Europe and serving as Associate Editor for “Paediatric Anaesthesia” and of Springer’s Journal “Intensive Care Medicine – paediatric and neonatal”.
References
Alonso‐Iñigo J. M., Escribá F. J., Carrasco J. I., Fas M. J., Argente P., Galvis J. M., & Llopis J. E. (2016). Measuring cardiac output in children undergoing cardiac catheterization : comparison between the Fick method and PRAM (pressure recording analytical method). Paediatric Anaesthesia, 26(11), 10971105. https://doi.org/10.1111/pan.12997



