Why Ease of Use Matters
For anaesthesiologists, intensivists, and critical care nurses, time and cognitive bandwidth are limited resources. While traditional vital signs can be slow or nonspecific during early instability, continuous haemodynamic monitoring delivers real-time, operator-independent insights that help clinicians intervene earlier and with more confidence. Minimally invasive, calibration free methods reduce the procedural burden, making advanced monitoring more usable at the bedside. 13
When Usability is Poor, Adoption Drops
Hospitals that transitioned to uncalibrated, consumable-free arterial waveform monitoring reported reduced workload, fewer interruptions, and time savings, clear indicators that usability directly impacts daily practice. 2, 7
Poor usability typically manifests in four predictable ways:
1. Calibration Overhead
Systems requiring initial and repeated calibrations introduce delays, interrupt workflow, and increase cognitive load, precisely when clinicians need seamless, continuous data. Studies highlight calibration steps as a major barrier to adoption in minimally invasive cardiac output monitoring. 1,2 , 7
2. Dependence on Captive Disposables
Technologies tied to dedicated disposables increase supply‑chain dependency, setup friction, and operating costs. Comparative clinical work emphasises that methods not requiring indicator injections or specialised sensors remove a recurring logistical constraint, important for busy operating rooms and ICUs where rapid turnover and team rotation are common. 2,7
3. Operator‑Dependent Steps
Manual inputs and user-dependent manoeuvres increase variability across shifts. Minimising these inputs leads to more consistent measurements and easier teamwide adoption. 2
4. Loss of Trending Continuity
Any required recalibration or sensor exchange creates a break in data, reducing the clinical value of trends just when they are most needed. Early waveform research emphasised uninterrupted monitoring as critical for therapy titration.
Clinicians Want Simplicity
While technology continues to provide increasingly detailed haemodynamic data, clinicians face growing cognitive demands in time‑critical environments. From the user’s perspective, tools that are intuitive and easy to operate can make a decisive difference, as reflected in the following clinical insight:
“In contemporary anaesthesia practice, hemodynamic monitoring plays a key role in guiding individualized, physiology-based management throughout the perioperative period. When monitoring systems are easy to use, clinicians can rapidly interpret dynamic hemodynamic data, reduce cognitive workload, and make timely, informed decisions, particularly in time-critical situations, thereby supporting safer and more effective patient care”
Dr. Amélia Ferreira, Portugal
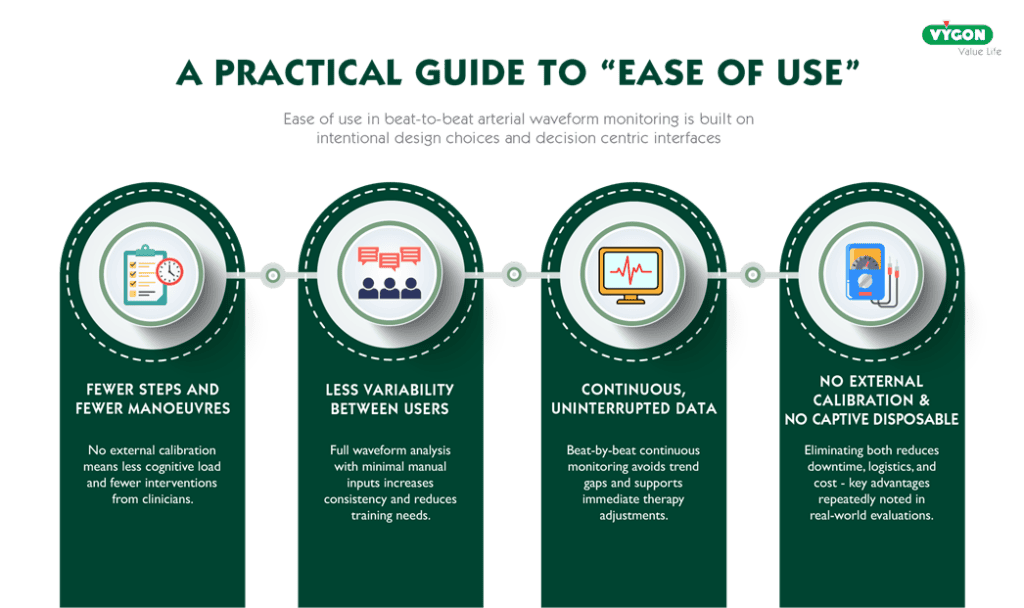
A Practical Guide to “Ease of Use”
In real clinical workflows, ease of use comes down to:
- Fewer steps and fewer manoeuvres: No external calibration means less cognitive load and fewer interventions from clinicians.
- Less variability between users: Full waveform analysis with minimal manual inputs increases consistency and reduces training needs.
- Continuous, uninterrupted data: Beat-by-beat continuous monitoring avoids trend gaps and supports immediate therapy adjustments.
- No external calibration, no captive disposables: Eliminating both reduces downtime, logistics, and cost, key advantages repeatedly noted in real-world evaluations.
Workflow Impact in Theatre and ICU
In the ICU, calibration-free, operator-independent systems promote consistent team adoption and reduce downtime. Large observational data confirm the feasibility of continuous waveform monitoring in unselected critically ill patients. 2, 3
Increasingly, researchers are trying to validate non‑calibrated haemodynamic techniques, often by comparing them with calibration‑dependent methods immediately after calibration. This trend reflects a growing demand for continuous monitoring solutions that eliminate the inconvenience of repeated calibrations while still ensuring reliability. In this context, the studies conducted highlight even more clearly that removing the calibration step in waveform-based methods significantly enhances both usability and workflow efficiency.”. 1,2, 7
Conclusion
Ease of use is not an accessory feature; it is the primary enabler of meaningful haemodynamic monitoring adoption. Systems designed to be calibration-free, operator-independent, and seamless to set up deliver faster starts, lower cognitive burden, fewer workflow interruptions, and broader team acceptance. The result: more continuous data, better clinical integration, and more reliable support for therapy decisions in both OR and ICU environments.
References
- Romano SM, Pistolesi M. Assessment of cardiac output from systemic arterial pressure in humans. Crit Care Med. 2002;30(8):18341841. doi:10.1097/00003246-200208000-00027. https://journals.lww.com/ccmjournal/Abstract/2002/08000/Assessment_of_cardiac_output_from_systemic.27.aspx [journals.lww.com]
- Romagnoli S, Franchi F, Ricci Z, Scolletta S, Payen D. The Pressure Recording Analytical Method (PRAM): Technical Concepts and Literature Review. J Cardiothorac Vasc Anesth. 2017;31(4):14601470. doi:10.1053/j.jvca.2016.09.004. https://europepmc.org/article/MED/28012725 [europepmc.org]
- Scolletta S, Romano SM, Biagioli B, Capannini G, Giomarelli P. Pressure recording analytical method (PRAM) for measurement of cardiac output during various haemodynamic states. Br J Anaesth. 2005;95(2):159165. doi:10.1093/bja/aei154. https://academic.oup.com/bja/article-abstract/95/2/159/313940 [academic.oup.com]
- Calamandrei M, Mirabile L, Muschetta S, Gensini GF, De Simone L, Romano SM. Assessment of cardiac output in children: A comparison between the pressure recording analytical method and Doppler echocardiography. Pediatr Crit Care Med. 2008;9(3):310312. doi:10.1097/PCC.0b013e31816c7151. https://journals.lww.com/pccmjournal/Abstract/2008/05000/Assessment_of_cardiac_output_in_children__A.12.aspx [journals.lww.com]
- Scolletta S, Franchi F, Romagnoli S, et al. Comparison Between DopplerEchocardiography and Uncalibrated Pulse Contour Method for Cardiac Output Measurement: A Multicenter Observational Study. Crit Care Med. 2016;44(7):13701379. doi:10.1097/CCM.0000000000001663. https://iris.univpm.it/handle/11566/235915 [iris.univpm.it]
- Zangrillo A, Maj G, Monaco F, et al. Cardiac Index Validation Using the Pressure Recording Analytic Method in Unstable Patients. J Cardiothorac Vasc Anesth. 2010;24(2):265269. doi:10.1053/j.jvca.2009.09.019. https://www.jcvaonline.com/article/S1053-0770(09)00357-7/abstract [jcvaonline.com]
- Donati A, Carsetti A, Tondi S, et al. Thermodilution vs pressure recording analytical method in hemodynamic stabilized patients. J Crit Care. 2014;29(2):260265. (Detalles en repositorio IRIS). https://iris.hunimed.eu/handle/11699/14681 [iris.hunimed.eu]
- Saxena R, Durward A, Puppala NK, Murdoch IA, Tibby SM. Pressure recording analytical method for measuring cardiac output in critically ill children: a validation study. Br J Anaesth. 2013;110(3):425431. doi:10.1093/bja/aes420. https://academic.oup.com/bja/article/110/3/425/249432 [academic.oup.com]
- Li MW, Wang SX, Zhang H, et al. The predictive value of pressure recording analytical method for the duration of mechanical ventilation in children undergoing cardiac surgery with an XGBoostbased machine learning model. Front Cardiovasc Med. 2022;9:1036340. doi:10.3389/fcvm.2022.1036340. https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2022.1036340/full [frontiersin.org]
- Scolletta S, Romano SM, Biagioli B, Capannini G, Giomarelli P. (Porcine model) Pressure recording analytical method validation across haemodynamic states. Br J Anaesth. 2005;95(2):159165. doi:10.1093/bja/aei154. https://ichgcp.net/es/clinical-trials-registry/publications/38269-pressure-recording-analytical-method-pram-for-measurement-of-cardiac-output-during-various
- MedTech Insights. Cardiac output monitors benefit patients and clinicians at Croydon hospital. Published February 12, 2025. https://med-tech-insights.com/2025/02/12/cardiac-output-monitors-benefit-patients-and-clinicians-at-croydon-hospital/. Accessed January 13, 2026.
- Giacomelli E, Dorigo W, Romano SM, et al. The Use of Pressure Recording Analytical Method in Patients Undergoing Endovascular Repair for Abdominal Aortic Aneurysm: The Impact on Clinical Decisions for the Appropriate Postoperative Setting and Cost‑effective Analysis. Acta Med Acad. 2024;53(1):10‑23. doi:10.5644/ama2006-124.442. https://europepmc.org/article/MED/38984696. Accessed January 13, 2026.
- Abusannuga, M., Attique, Z., Abdulla, S., Zulfiqar, H., Almohannadi, M., & Shajahan, F. (2025). Advanced Hemodynamic Monitoring: Pros, Cons, and the Future. IntechOpen. doi: 10.5772/intechopen.1011933
- Peng M, Ning Y, Zhang J, He Y, Xu Z, Li D, Yang Y, Ren T-L. Wearable Sensing Systems for Multi-Modal Body Fluid Monitoring: Sensing-Combination Strategy, Platform-Integration Mechanism, and Data-Processing Pattern. Biosensors. 2026; 16(1):46. https://doi.org/10.3390/bios16010046



